Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
OBSTETRICS AND GYNAECOLOGY / CLINICAL RESEARCH
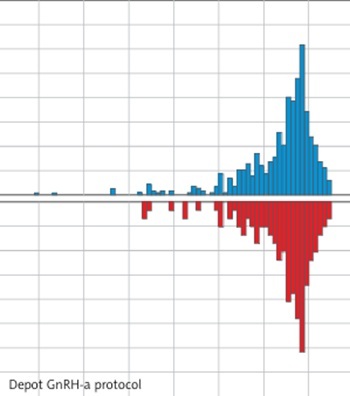
GnRH antagonist versus depot GnRH agonist protocol in polycystic ovary syndrome (PCOS): analysis using propensity score matching
1
Jiangxi Maternal and Child Health Hospital Affiliated to Nanchang University,
Nanchang, China
2
Columbia College of Art and Science, the George Washington University,
Washington, USA
Submission date: 2020-12-10
Final revision date: 2021-02-07
Acceptance date: 2021-02-21
Online publication date: 2021-03-20
Corresponding author
Qiongfang Wu
Jiangxi Maternal and Child Health Hospital Affiliated to Nanchang University Nanchang, China
Jiangxi Maternal and Child Health Hospital Affiliated to Nanchang University Nanchang, China
KEYWORDS
polycystic ovary syndromein vitro fertilizationGnRH antagonist protocoldepot GnRH agonist protocolpropensity score matching
TOPICS
ABSTRACT
Introduction:
Women with polycystic ovary syndrome (PCOS) have been reported to have a low pregnancy rate and high ovarian hyperstimulation syndrome (OHSS) risk in in vitro fertilization (IVF) programs due to the decreased endometrial receptivity and high ovarian reserve. The GnRH antagonist (GnRH-ant) protocol has been widely accepted as a prominent intervention to reduce the risk of OHSS, and been recommended as the preferred protocol. The depot GnRH agonist (dGnRH-a) protocol is believed to improve endometrial receptivity and increase the pregnancy rate of fresh embryo transfer. There have been no previous studies comparing the two protocols.
Material and methods:
This was a retrospective cohort study that included 2164 women with PCOS undergoing assisted reproductive technology (ART) treatment between January 2014 and April 2019. Among them, 2018 women received dGnRH-a protocol treatment and 146 women received GnRH-ant protocol treatment. The two groups were matched by propensity scores with a ratio of 4 : 1 to account for potential confounding factors. The primary outcomes were the live birth rate (LBR), incidence of moderate-to-severe OHSS and the cost of controlled ovarian hyperstimulation (COH). Live birth rate was defined as live births per treatment cycle after the first fresh or frozen embryo transfer.
Results:
The live birth rate per treatment cycle was higher in the dGnRH-a group than in the GnRH-ant group (58.22% vs. 41.78%, p = 0.0004), as was the live birth rate per fresh transfer (64.42% vs. 44.64%, p = 0.0045). However, the live birth rate per frozen transfer was similar in the two groups. There were no significant differences in the incidence of moderate-to-severe OHSS (4.28% vs. 2.05%, p = 0.333), the incidence of severe OHSS (0.17% vs. 0%, p = 1) and the cost of COH (RMB: 7736.9 vs. 8046.54, p = 0.113) between the two groups.
Conclusions:
Our results indicated that the dGnRH-a protocol had a higher live birth rate than the GnRH-ant protocol, and the difference was mainly due to fresh embryo transfer. Regarding safety and economic cost, the incidence of moderate-to-severe OHSS and cost of COH were similar in the two groups. The incidence of moderate-to-severe OHSS in the dGnRH-a group was higher than in the GnRH-ant group, but without statistical difference. A subsequent prospective randomized controlled study is needed to confirm these results.
Women with polycystic ovary syndrome (PCOS) have been reported to have a low pregnancy rate and high ovarian hyperstimulation syndrome (OHSS) risk in in vitro fertilization (IVF) programs due to the decreased endometrial receptivity and high ovarian reserve. The GnRH antagonist (GnRH-ant) protocol has been widely accepted as a prominent intervention to reduce the risk of OHSS, and been recommended as the preferred protocol. The depot GnRH agonist (dGnRH-a) protocol is believed to improve endometrial receptivity and increase the pregnancy rate of fresh embryo transfer. There have been no previous studies comparing the two protocols.
Material and methods:
This was a retrospective cohort study that included 2164 women with PCOS undergoing assisted reproductive technology (ART) treatment between January 2014 and April 2019. Among them, 2018 women received dGnRH-a protocol treatment and 146 women received GnRH-ant protocol treatment. The two groups were matched by propensity scores with a ratio of 4 : 1 to account for potential confounding factors. The primary outcomes were the live birth rate (LBR), incidence of moderate-to-severe OHSS and the cost of controlled ovarian hyperstimulation (COH). Live birth rate was defined as live births per treatment cycle after the first fresh or frozen embryo transfer.
Results:
The live birth rate per treatment cycle was higher in the dGnRH-a group than in the GnRH-ant group (58.22% vs. 41.78%, p = 0.0004), as was the live birth rate per fresh transfer (64.42% vs. 44.64%, p = 0.0045). However, the live birth rate per frozen transfer was similar in the two groups. There were no significant differences in the incidence of moderate-to-severe OHSS (4.28% vs. 2.05%, p = 0.333), the incidence of severe OHSS (0.17% vs. 0%, p = 1) and the cost of COH (RMB: 7736.9 vs. 8046.54, p = 0.113) between the two groups.
Conclusions:
Our results indicated that the dGnRH-a protocol had a higher live birth rate than the GnRH-ant protocol, and the difference was mainly due to fresh embryo transfer. Regarding safety and economic cost, the incidence of moderate-to-severe OHSS and cost of COH were similar in the two groups. The incidence of moderate-to-severe OHSS in the dGnRH-a group was higher than in the GnRH-ant group, but without statistical difference. A subsequent prospective randomized controlled study is needed to confirm these results.
REFERENCES (34)
1.
Chang WY, Knochenhauer ES, Bartolucci AA, Azziz R. Phenotypic spectrum of polycystic ovary syndrome: clinical and biochemical characterization of the three major clinical subgroups. Fertil Steril 2005; 83: 1717-23.
2.
Ainehchi N, Khaki A, Ouladsahebmadarek E, et al. The effect of clomiphene citrate, herbal mixture, and herbal mixture along with clomiphene citrate on clinical and para-clinical parameters in infertile women with polycystic ovary syndrome: a randomized controlled clinical trial. Arch Med Sci 2020; 16: 1304-18.
3.
Lopes IM, Baracat MC, Simoes MJ, Simoes RS, Baracat EC, Soares JJ. Endometrium in women with polycystic ovary syndrome during the window of implantation. Rev Assoc Med Bras (1992) 2011; 57: 702-9.
4.
Schulte MM, Tsai JH, Moley KH. Obesity and PCOS: the effect of metabolic derangements on endometrial receptivity at the time of implantation. Reprod SCI 2015; 22: 6-14.
5.
Ng EHY, Tang OS, Ho PC. The significance of the number of antral follicles prior to stimulation in predicting ovarian responses in an IVF programme. Hum Reprod 2000; 15: 1937-42.
6.
Lin H, Li Y, Li L, Wang W, Yang D, Zhang Q. Is a GnRH antagonist protocol better in PCOS patients? A meta-analysis of RCTs. Plos One 2014; 9: e91796.
7.
Toftager M, Bogstad J, Bryndorf T, et al. Risk of severe ovarian hyperstimulation syndrome in GnRH antagonist versus GnRH agonist protocol: RCT including 1050 first IVF/ICSI cycles. Hum Reprod 2016; 31: 1253-64.
8.
Hwang JL, Chen SU, Chen HJ, et al. Feasibility of corifollitropin alfa/GnRH antagonist protocol combined with GnRH agonist triggering and freeze-all strategy in polycystic ovary syndrome patients. J Formos Med Assoc 2018; 117: 535-40.
9.
Nakamura K, Oosawa M, Kondou I, et al. Menotropin stimulation after prolonged gonadotropin releasing hormone agonist pretreatment for in vitro fertilization in patients with endometriosis. J Assist Reprod Genet 1992; 9: 113-7.
10.
Tu J, Lin G, Lu C, Gong F. A novel modified ultra-long agonist protocol improves the outcome of high body mass index women with polycystic ovary syndrome undergoing IVF/ICSI. Gynecol Endocrinol 2014; 30: 209-12.
11.
Ren J, Sha A, Han D, Li P, Geng J, Ma C. Does prolonged pituitary down-regulation with gonadotropin-releasing hormone agonist improve the live-birth rate in in vitro fertilization treatment? Fertil Steril 2014; 102: 75-81.
12.
Gong F, Li X, Zhang S, et al. A modified ultra-long pituitary downregulation protocol improved endometrial receptivity and clinical outcome for infertile patients with polycystic ovarian syndrome. Exp Ther Med 2015; 10: 1865-70.
13.
Mourad S, Brown J, Farquhar C. Interventions for the prevention of OHSS in ART cycles. an overview of Cochrane reviews. Cochrane Database Syst Rev 2017; 1: D12103.
14.
Rotterdam ESHRE/ASRM-Sponsored PCOS consensus workshop group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril 2004; 81: 19-25.
15.
Golan A, Ron-el R, Herman A, Soffer Y, Weinraub Z, Caspi E. Ovarian hyperstimulation syndrome: an update review. Obstet Gynecol Surv 1989; 44: 430-40.
16.
Balen AH, Morley LC, Misso M, et al. The management of anovulatory infertility in women with polycystic ovary syndrome: an analysis of the evidence to support the development of global WHO guidance. Hum Reprod Update 2016; 22: 687-708.
17.
Lambalk CB, Banga FR, Huirne JA, et al. GnRH antagonist versus long agonist protocols in IVF: a systematic review and meta-analysis accounting for patient type. Hum Reprod Update 2017; 23: 560-79.
18.
Surrey ES, Silverberg KM, Surrey MW, Schoolcraft WB. Effect of prolonged gonadotropin-releasing hormone agonist therapy on the outcome of in vitro fertilization-embryo transfer in patients with endometriosis. Fertil Steril 2002; 78: 699-704.
19.
Zikopoulos K, Kolibianakis EM, Devroey P. Ovarian stimulation for in vitro fertilization in patients with endometriosis. Acta Obstet Gynecol Scand 2004; 83: 651-5.
20.
Tian LF, Tan J, Zou Y, et al. Mild starting dosage ovarian stimulation combined with a modified prolonged GnRH-a protocol improved IVF/ICSI outcomes in normal ovarian responders. Arch Med Sci 2019; 15: 1294-300.
21.
Xu B, Geerts D, Hu S, et al. The depot GnRH agonist protocol improves the live birth rate per fresh embryo transfer cycle, but not the cumulative live birth rate in normal responders: a randomized controlled trial and molecular mechanism study. Hum Reprod 2020; 35: 1306-18.
22.
Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika 1983; 70: 41-55.
23.
Cao H, Li H, Zhu X, et al. Three non-invasive ventilation strategies for preterm infants with respiratory distress syndrome: a propensity score analysis. Arch Med Sci 2020; 16: 1319-26.
24.
Hughes EG, Fedorkow DM, Daya S, Sagle MA, Van de Koppel P, Collins JA. The routine use of gonadotropin-releasing hormone agonists prior to in vitro fertilization and gamete intrafallopian transfer: a meta-analysis of randomized controlled trials. Fertil Steril 1992; 58: 888-96.
25.
Lin LS, Roberts VJ, Yen SS. Expression of human gonadotropin-releasing hormone receptor gene in the placenta and its functional relationship to human chorionic gonadotropin secretion. J Clin Endocrinol Metab 1995; 80: 580-5.
26.
Casan EM, Raga F, Polan ML. GnRH mRNA and protein expression in human preimplantation embryos. Mol Hum Reprod 1999; 5: 234-9.
27.
Nishihara S, Fukuda J, Ezoe K, et al. Does the endometrial thickness on the day of the trigger affect the pregnancy outcomes after fresh cleaved embryo transfer in the clomiphene citrate-based minimal stimulation cycle? Reprod Med Biol 2020; 19: 151-7.
28.
Onogi S, Ezoe K, Nishihara S, Fukuda J, Kobayashi T, Kato K. Endometrial thickness on the day of the LH surge: an effective predictor of pregnancy outcomes after modified natural cycle-frozen blastocyst transfer. Hum Reprod Open 2020; 2020: hoaa060.
29.
Edwards RG. Clinical approaches to increasing uterine receptivity during human implantation. Hum Reprod 1995; 10 (Suppl. 2): 60-6.
30.
Maheshwari A, McLernon D, Bhattacharya S. Cumulative live birth rate: time for a consensus? Hum Reprod 2015; 30: 2703-7.
31.
Chen ZJ, Shi Y, Sun Y, et al. Fresh versus frozen embryos for infertility in the polycystic ovary syndrome. N Engl J Med 2016; 375: 523-533.
32.
Benmachiche A, Benbouhedja S, Zoghmar A, Humaidan P. Low LH level on the day of GnRH agonist trigger is associated with reduced ongoing pregnancy and live birth rates and increased early miscarriage rates following IVF/ICSI treatment and fresh embryo transfer. Front Endocrinol (Lausanne) 2019; 10: 639.
33.
Raju GA, Chavan R, Deenadayal M, et al. Luteinizing hormone and follicle stimulating hormone synergy: A review of role in controlled ovarian hyper-stimulation. J Hum Reprod Sci 2013; 6: 227-34.
34.
Westergaard LG, Laursen SB, Andersen CY. Increased risk of early pregnancy loss by profound suppression of luteinizing hormone during ovarian stimulation in normogonadotrophic women undergoing assisted reproduction. Hum Reprod 2000; 15: 1003-8.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.