Kawasaki disease (KD) is a common systemic vasculitis that predominantly affects children younger than 5 years old. A recent epidemiological survey from China showed that the average annual incidence of KD was 94.7 per 100,000 children aged 0–4 years in the period from 2013 to 2017, and 9.1% of cases were complicated with coronary artery lesions (CAL) [1]. In addition, it has been reported that KD can also be associated with other organ lesions, such as aseptic meningitis, anterior uveitis, arthritis, cranial nerve palsies, pancreatitis, hepatic dysfunction and Grisel syndrome (GS) [2–4]. GS, also known as non-traumatic atlantoaxial subluxation, is usually caused by inflammatory conditions of the upper neck and otorhinolaryngology procedures [5]. Liu et al. [4] reviewed the clinical data of 1582 Chinese patients with KD, and discovered that only 0.6% of them suffered from GS. In the present report, we encountered an unusual case of KD in an older boy with GS and peripheral arthritis.
A previously healthy 7-year-old Chinese boy was referred to our department with a 4-day history of fever, neck pain and limited mobility. He had no history of head or neck trauma. On admission, his blood pressure was 110/62 mm Hg, heart rate was 102 beats per minute, axillary temperature was 38.5°C and respiratory rate was 22 breaths per minute. Physical examination revealed head turned to the left, limited neck range of motion and enlarged bilateral cervical lymph nodes. Cardiac and neurologic physical examinations were both unremarkable. His initial blood counts were as follows (Table I): white blood cells (WBC), 22.52 × 109/l with 86.44% neutrophils and 4.74% lymphocytes; hemoglobin, 112 g/l; and platelets, 291 × 109/l. Other blood chemistry values included: C-reactive protein (CRP), 187.33 mg/l; procalcitonin (PCT), 1.3 ng/ml; erythrocyte sedimentation rate (ESR), 88 mm/h; alanine aminotransferase, 52 U/l; and aspartate aminotransferase, 37 U/l. The ultrasound identified cervical lymph nodes measuring 2.2 × 1.2 cm in the maximum diameter. Results from the patient’s admission blood culture were negative. Echocardiography revealed no significant abnormality in internal diameter of the coronary artery; however, the ejection fraction exhibited a marked reduction on day 5, and was restored on day 10 (Table I). X-ray showed asymmetry in the atlantoaxial joint (Figure 1 A). Cervical computed tomographic (CT) scan demonstrated atlantoaxial subluxation with an atlantodental interval (ADI) of 2.73 mm (Figure 1 B). The patient was given anti-infection therapy and neck braces to immobilize his neck. On day 5 after admission, he presented with bilateral conjunctival congestion, cracked lips, strawberry tongue and right hip joint pain. Magnetic resonance imaging (MRI) showed bilateral hip joint effusion-synovitis and right ankle joint effusion (Figures 1 C, D). On day 10, the fever, bilateral conjunctival congestion, cracked lips, strawberry tongue and right hip joint pain had subsided, whereas peeling skin was found on his hands, buttocks and feet. Repeated blood counts and the inflammatory detections indicated that WBC was 6.61 × 109/l, hemoglobin was 101 g/l, platelet count was 476 × 109/l, CRP was 19.66 mg/l, PCT was 0.067 ng/ml and ESR was 86 mm/h. Based on clinical and laboratory findings, the patient was diagnosed as having typical KD, combined with GS and peripheral arthritis simultaneously. Since the course of the disease lasted over 10 days and the inflammatory reaction significantly resolved, intravenous immunoglobulin (IVIG) was not used and aspirin (4 mg/kg/day) was initiated. On day 12, GS was relieved and the patient was discharged. Two months later, repeated echocardiography demonstrated no abnormal findings.
Table I
Laboratory test performed in hospitalization
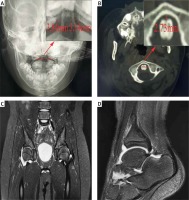
Figure 1
Imaging findings of patient. A – Open mouth radiograph showed asymmetry of the odontoid process in relation to the lateral masses of the atlas. B – CT scan demonstrated atlantoaxial subluxation with ADI of 2.73 mm. C – MRI showed bilateral hip joint effusion-synovitis. D – MRI revealed right ankle joint effusion
Arthritis is not uncommon in KD patients, whereas axial joint involvement as the initial manifestation in KD patients is even rarer. Guleria et al. [6] retrospectively reviewed the clinical records of 865 KD patients from 1994 to 2019 in India, and identified that 4.6% of patients manifested arthritis; and among them, 30 patients had knee involvement, 15 patients had ankle involvement, 14 patients had hip involvement, and only 1 patient had cervical spine involvement. In the present report, we encountered an unusual case of KD in a 7-year-old boy with GS and peripheral arthritis. The pathogenesis of GS in KD may be attributed to neck inflammatory processes leading to ligament hypermobility with expansion and abnormal flabby ligaments surrounding the neck joint and sternomastoid spasm. GS can be alleviated with inhibition of the systemic inflammatory response and local fixation. In addition, Liu et al. [4] reported that GS in KD occurred mainly in the age group between 4 and 8 years, commonly higher than the peak age of KD. We speculated that older children might be a potential risk factor for GS in KD.
In this case, the patient was 7 years old. KD occurs mainly in infancy or early childhood, and 85.3% of patients present when younger than 5 years old, with an average age of 32.78 ±27.41 months in China [7]. It is uncommon in older children. High-dose IVIG combined with aspirin serves as the first choice to inhibit continuing systemic inflammation and prevent CAL in the acute phase of KD. According to the 2017 American Heart Association guidelines for KD, IVIG usually should not be given to patients with delayed diagnosis (after 10 days of illness) in the absence of fever, coronary artery abnormalities, or notably elevated inflammatory markers [2]. In this report, the patient was diagnosed with KD on day 10 after admission. On this occasion, peeling skin occurred, body temperature and WBC had declined to baseline, and CRP, PCT and ESR had significantly decreased; thus IVIG was not used. However, aspirin (4 mg/kg/day) was initiated owing to the elevated platelets and hypercoagulability. Since there is no specific diagnostic test for KD, it is often challenging to discriminate KD from infectious febrile disease. Our previous study [8] including 254 KD children showed that the proportion of KD patients with a PCT concentration below 0.25 ng/ml was 11-fold higher than that of sepsis patients, indicating that PCT concentration below 0.25 ng/ml may be a useful biomarker for discriminating KD from sepsis. More persuasively, Liu et al. [9] established a novel nomogram model to differentiate KD from sepsis and found that PCT ≤ 0.5 ng/ml was a strong predictor for KD and associated with a 3.41-fold increase in KD probability. It is worth noting that the involvement of the cardiovascular system should also be closely monitored during the subsequent follow-up.



