Introduction
Low back pain (LBP) is the most common reason for physiotherapy consultation. It affected 619 million people globally in 2020 and driven by aging it is estimated that this number will increase to 843 million cases by 2050 [1–3].
One of the important aims of orthopedic medicine is to classify patients with LBP into sub-groups and in consequence to provide the appropriate therapy. The literature suggests that specific treatment for specific sub-groups resulted in better therapeutic outcomes after the intervention [4].
Worldwide there are many types of therapeutic approach, from drug prescription through physical therapy and mechanical therapy to surgical procedures. Among physical therapies there are manual therapies such as integrated neuromuscular inhibition technique (INIT) and spray and stretch technique [5]. Moreover, in the case of enhanced patients’ care education and constant training, new technologies are used [6].
In the group of mechanical therapy is the McKenzie Method, also known as Mechanical Diagnosis and Therapy (MDT). It is currently one of the most well-known methods for diagnosing and treating spinal and limb pain syndromes. One of the most valuable parts of the method is the patient’s examination and broad interview, which lead, after mechanical diagnostics, to the division of the patients into sub-groups. The examination procedure is very specific and it is based on the McKenzie Institute Lumbar Spine Assessment. In the part connected to the symptom characteristics during daily activities, patients answer the questions about their perception of the pain and other symptoms. This part of the examination is valuable in two aspects: understanding the perception of the patient and beginning to find the specific role of the movement in the worsening or improvement of the symptoms.
McKenzie therapy places particular emphasis on the patient’s understanding of the entire rehabilitation process and their conscious and independent replication of it in home settings, making them co-responsible for the therapy process and the return to functional and pain-free functioning in daily life [7]. Each patient is given a prescription for frequency and duration of exercises based on his or her classification, including expectations, safety guidelines, and warning signs [8]. In LBP therapy it is very important to control the treatment in the centralization phenomenon [9–14]. Patients with directional preference (DP) specific to a current incident of LBP may control their symptoms while exercising the specific movement. It should lead to the centralization of the symptoms. It usually occurs with restoration of range of motion in the lumbar part of the spine. The most desired therapeutic result is the pain-reduction effect.
The distribution in the McKenzie classification shows that the most common is derangement in patients with directional preference. It was observed that the most common direction causing the centralization was extension of the lumbar spine, but the different directions were also significant in treatment, so the pain-relief effect exercise needs to be prescribed only after the specific examination [15–17].
The aim of the study is to compare the information from the interview (specifically regarding symptom characteristics, commonly worsening or improving the symptoms) with the applied therapeutic procedures due to centralization of the symptoms in patients with derangement syndrome.
The following research questions were formulated:
How can patients characterize their symptoms during everyday movements?
In which classification of derangement syndrome (DS) did patients with pain most commonly present to the therapist, divided according to gender, type of occupation, and age?
What therapeutic procedures were most frequently used in patients with DS?
What therapeutic direction was applied in patients with DS, based on interview information regarding symptoms experienced in different positions during daily activities?
Material and methods
Research methods
The study was conducted after obtaining approval from the Bioethics Committee at the Piastów Śląskich Medical University in Wrocław, under protocol number KB – 305/2020.
A retrospective study was conducted based on the therapeutic records of patients treated using the McKenzie method. The records were completed and the therapy was administered by a certified McKenzie therapist.
The study examines the relationship between the therapeutic procedures used for the lumbar spine treatment and the interview information regarding the worsening and improvement of symptoms observed by the patient throughout the day during specific movements. A total of 400 patients’ records were analyzed. Thirty-three records were excluded due to missing data, and 65 records were excluded due to a different level of injury (cervical or thoracic). Ultimately, 302 patients were included in the study. In order to verify the hypotheses formulated within the study, statistical analyses were conducted. The data were compiled in various schemes: gender, age range, type of occupation, classification, positional variations, and the implemented directional procedures.
The first part of the patient’s examination included a detailed medical history interview, enabling the identification of the topography and symptoms, as well as the characteristics of symptoms during changes in body position. The interview took place with the patient seated in a chair, allowing observation of the position assumed by the patient. The initial stage of the interview involves gathering information about the patient. Questions are asked regarding the patient’s age, occupation, and activities during leisure time. A significant piece of information for the therapist is the level of functional disability. The patient describes their type of work and physical activities undertaken.
The second part of the questionnaire provides information about the symptoms. First and foremost, the patient describes the symptoms of the current episode, which brought them to the therapist, including those experienced over the past few days. The description of symptoms includes precise locations of pain, paresthesia, differentiation between central, symmetrical, unilateral, and asymmetrical pain, as well as the extent of radiating pain [17]. Depending on the issue, pain can occur locally or radiate peripherally. This indicates, among other things, the level of the problem that the person has encountered [18–20]. Any information provided by the patient is then mapped by the therapist onto a human figure and confirmed by the patient once again. The third part of the subjective examination focuses on the characteristics of previous episodes of pain. In the fourth part of the interview, special questions are asked related to tingling, numbness, muscle weakness, or gait disturbances. Functional diagnostics in the McKenzie Method begin with the seated correction test. This procedure allows conclusions to be drawn and brings us closer to reaching a final diagnosis. The next examination, the repeated movement test, aims to classify the patient into one of three clinical syndromes. McKenzie distinguishes between postural syndrome, dysfunction syndrome, and derangement syndrome [11, 21, 22]. In therapy, the derangement syndrome is the most commonly encountered.
Derangement syndrome manifests as pain associated with disruption of the internal structures within the intervertebral disc [11].
McKenzie distinguishes three categories of derangement syndrome:
D1: Central and symmetrical pain syndrome in the lower back (low back pain – LBP), rarely accompanied by buttock or thigh pain, without deformity.
D3: Unilateral pain syndrome in the lower back, may cause pain in the buttocks or thigh above the knee.
D5: Unilateral pain syndrome in the lower back, pain in the buttock or thigh extending below the knee [9].
Results
Characteristics of the study participants
A total of 302 individuals took part in the study. Among them, 58% were women and 42% were men.
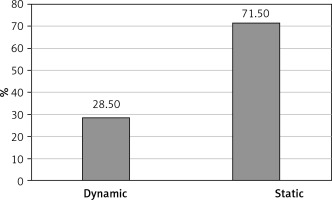
The age range of the study participants was 16 to 88 years. The participants were allocated to three age groups. Group I (16-40 years), Group II (41–60 years), and Group III (61–88 years). Group I comprised 35.3% of the participants, Group II comprised 49.3%, and Group III comprised 15.3% (Figure 1). The average age was 47 years.
Figure 1
A pie chart illustrating the number of individuals divided into three age groups. Group I (16–40 years), Group II (41–60 years), and Group III (61–88 years)
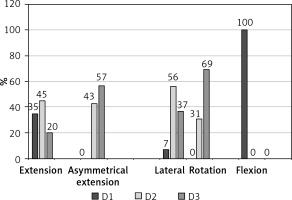
Dynamic work was performed by 28.50% of the participants, while static work was performed by 71.50% of the participants (Figure 2).
The applied directional preference in relation to interview information regarding symptoms experienced in different positions during daily activities (section worse/better/no change)
During the interview, patients were asked in which positions their pain symptoms worsened, improved, or remained unchanged. The individuals treated with the extension directional preference most commonly reported an increase in pain symptoms during sitting, bending, and standing (over 50% of participants), and a reduction in pain symptoms while walking and lying on their back (less than 30% of participants). Pain sensations did not change while lying on the stomach (75% of participants), lying on the right, left side, getting up, and lying on their back (over 50% of responses).
Individuals treated with the asymmetrical extension procedure reported an increase in pain symptoms during walking, sitting, and standing (over 50% of participants), while a reduction in symptoms was reported during lying on their back and on the right side (over 20% of responses). No changes in pain sensations were observed in the following positions: lying on the stomach (over 81% of participants), lying on the left side, getting up, lying on the right side, lying on the back, and bending (over 50% of responses).
In the group of individuals treated with lateral DP, worsening of symptoms was observed during sitting, standing, and walking (over 50% of responses), as well as during bending (reported by 49% of participants). A reduction in pain symptoms was noted during lying on the right side (over 20% of participants), lying on the back, and while walking (20% of responses). Patients in this group did not observe changes in pain intensity in the following positions: lying on the stomach (83% of participants), getting up, lying on the right and left sides, lying on the back, and bending (over 50% of responses).
In the group of individuals with a rotational directional preference, significant worsening of symptoms was observed during sitting (60% of participants) as well as standing, bending, walking, and getting up (ranging between 30% and 50%). Improvement in pain sensations was noted during lying on the stomach (20% of participants) and while walking (17% of responses). Patients assigned the category of “no change” to the positions of lying on the right and left sides, lying on the back, lying on the stomach, getting up, bending, and standing (over 50% of participants).
Flexion DP was only applied to one person (0.003%). In this individual, an exacerbation of pain symptoms was observed during bending, sitting, getting up, walking, and standing, while a reduction in pain symptoms was noted during lying on the right and left sides. However, there were no changes in pain symptoms in the positions of lying on the stomach and lying on the back.
The data described above demonstrate that the position most frequently mentioned in the “worse” category was sitting, followed by standing. In the “better” category, the responses were more varied, but certain positions, such as lying on the back, walking, and lying on the right side, were mentioned repeatedly in some therapeutic directions. Positions where patients most commonly did not perceive a change in pain intensity were lying on the stomach, lying on the right side, and lying on the left side (Table I).
Table I
Comparison of the type of applied directional preference and patients’ pain sensations in a given position
Distribution of the classifications among the study participants
Classification within the derangement syndrome. Among all participants, 25% were classified as D1, 44% were classified as D3, and 30% were classified as D5.
In response to the question of which classification of derangement syndrome (D1-D5) patients with low back pain most commonly presented to the therapist, both among women and men, the D3 classification was predominant. The D1 classification was least common among women, while the D5 classification was least common among men.
Comparison of symptoms divided by type of occupation indicates that symptoms indicating the D3 classification were observed to a similar extent in both the static and dynamic work groups.
Among the study participants, divided by age groups, the D3 classification was predominant in age groups I and II, while the D5 classification dominated in age group III. With increasing age, the number of individuals classified as D1 decreased, while the number of individuals classified as D5 increased.
This indicates that centrally located symptoms in the lower back region were more common among younger patients, whereas pain extending below the knee was more frequent among older individuals (Table II).
Table II
Comparison of the impact of detailed variables on the allocation of patients to a specific classification of derangement syndrome
Therapeutic procedures
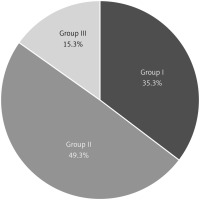
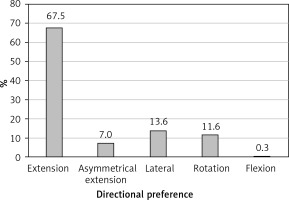
In response to the question of which therapeutic procedures were most commonly used in patients with derangement syndrome, among all participants, the extension directional procedure was applied in the vast majority (67.5%) of cases. The lateral and rotational directional procedures were subsequently used (13.6% and 11.6%, respectively).
Detailed data are presented in Figure 3.
Figure 3
A bar chart illustrating the percentage distribution of the applied directional preferences among the study participants
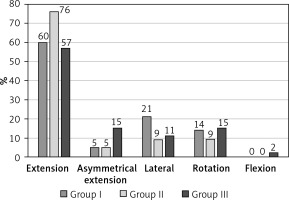
To obtain detailed information regarding the applied therapeutic procedures divided by age, the data were analyzed within the three age groups. In each age group, the extension directional preference was dominant. It was observed that in the oldest age group, the use of extension as a therapeutic procedure was least common, while the number of other therapeutic DP increased. Detailed results are illustrated in Figure 4.
Figure 4
A bar chart illustrating the frequency of applied therapeutic procedures divided by age groups
While dividing the participants based on the type of therapeutic procedure, it was observed that among those treated with the extension directional preference, the majority had symptoms extending to the knee (D3), followed by central pain, and the fewest had the D5 classification. Asymmetrical extension was used to treat individuals with symptoms below the knee (D5), and to a lesser extent with D3. This procedure was not applied to patients with central symptoms. Individuals treated with lateral DP were predominantly classified as D3, and the fewest belonged to D1. The rotational directional preference was applied to individuals with symptoms classified as D5, followed by D3. No patient with central symptoms had the rotational procedure recommended. The flexion DP was used only for one person with the D1 classification. Detailed results are illustrated in Figure 5.
Discussion
Lower back pain is considered one of the most common ailments in modern times [1]. Many studies have shown that almost every adult, at least once in his life, has experienced an incident causing painful symptoms in the lumbar region. Such a condition affects the psychosocial and physiological aspects of the patient [23]. The lumbar spine is considered the most susceptible to injuries [24]. According to Zawadka et al., spinal pain is a problem that affects 80% of the population at least once in their lifetime [25]. It intensifies the experience of pain and reduces the ability to work. The present lifestyle significantly impacts the functioning of our spine, particularly in performing its main functions.
The aim of the study was to compare the information from the interview (specifically regarding symptom characteristics, commonly worsening or improving the symptoms) with the applied therapeutic procedures due to centralization of the symptoms in patients with derangement syndrome.
The surveyed patients, regardless of their directional preference during therapy, indicated that sitting and standing positions increased their pain symptoms. They reported a reduction in symptoms when lying on their back, on their right side and during walking. Positions that did not affect their pain sensations were lying prone and lying on their right and left sides. These findings suggest that patients most commonly identified static positions as exacerbating their pain symptoms. Interestingly, the patients were able to clearly identify which positions increased their pain symptoms but were not able to determine which positions contributed to symptom reduction.
The next research question was about the classification of the symptoms (D1, D3, D5) of DS in patients according to gender, type of occupation, and age. Both in women and men, classification D3 was dominant (47% of women and 41% of men). The study included a higher proportion of women (58% of participants) than men (42%), which may indicate higher susceptibility of the female gender to back pain. Similarly, in many studies, women tended to report low back pain more frequently than men [26–29]. This hypothesis requires confirmation in other studies.
The occurrence of pain in the lumbar region is largely associated with repetitive movements at work and prolonged working hours. In our study, there were more individuals engaged in static work (71.5% of participants) compared to those in dynamic work (28.5% of participants). Also in the study of Augustyniuk et al. [30] it was found that based on the assessment and scale of spinal pain problems in the group of traders, it can be inferred that they are a professional group particularly prone to experiencing pain syndromes. A similar trend is described by Pramesti et al. [26], indicating a relationship between prolonged sitting at work and back pain. Individuals who spent more than 4 h in a seated position reported greater lower back pain compared to those who worked for less than 4 h. According to a study conducted by Klimaszewska et al. [31], out of 22.44% of participants reported an increase in pain during work involving movement, while 19.87% of participants reported pain exacerbation during seated work.
Referring to age, the occurrence of the LBP in the middle-aged patients (Group II 41–60 years old) was the highest. In this age group, the D3 classification was the most frequent (51% of the representants). With age the symptoms become peripheralized and in the 61-88 age group the D5 classification dominated (47% of representants).
Moreover, the dominance of classification D3 was observed in individuals engaged in both static and dynamic work.
In the derangement syndrome, the patients perform movements in the direction in which the symptoms decreased or centralized. We distinguish extension, asymmetrical extension, lateral, rotation, and flexion. Among the surveyed patients, the therapeutic direction most frequently applied was extension (67.5% of participants). The subsequent order of frequency was lateral (13.6% of participants), rotational (11.6% of participants), asymmetrical extension (7% of participants), and flexion (0.003% of participants). With age, the number of individuals treated with extension decreased, while the number of other therapeutic procedures increased. This could be due to an accumulation of painful incidents with age and/or inadequate treatment methods, leading to the progression of damage and the spread of painful symptoms.
In terms of the preference direction used as a therapeutic procedure, individuals classified as D1 were treated with extension, lateral, and flexion directions. Patients classified as D3 received each directional preference except flexion and a similar but different distribution was observed for patients classified as D5. These data demonstrate the dominance of D3 classification and the extension direction, but patients with D3 classification were also treated with various therapeutic directions. A similar trend was observed by Hefford [32]. The study of May et al. showed the same trend, and the authors emphasized that because patients’ symptoms respond positively to treatment only when treated with a specific DP, mechanical assessment is crucial to properly tailor the procedure to the patient’s condition [16].
McKenzie created a specific assessment and classification of patients that verifies their symptoms, including the most common, among others, the structural disorder group called “derangement” [15]. By conducting a thorough interview that involves detailed knowledge about the patient, including their type of work, activities performed outside of work, pain symptoms, and their pain responses in specific positions, a physiotherapist can approach determining the appropriate therapeutic direction to be applied to the individual. The article by Zadro [33] demonstrates the importance of physiotherapists providing appropriate advice and educating patients in order to prevent the onset of spinal conditions. Only when the interview is combined with precise diagnostics can conclusive conclusions be drawn to establish an accurate and targeted diagnosis and apply the appropriate treatment.
In conclusion, patients are not able to indicate certainly the movements which decrease the symptoms, while the movements which increase the symptoms are better recognized. Patients need to be treated by a certified physiotherapist and be educated about the centralization phenomenon and directional preference. While extension movements generally lead to a reduction in reported pain symptoms among patients with back pain, they are not the only directions that can centralize symptoms and should not be applied without a thorough symptom and mechanical examination of the patient.