Introduction
Probiotics favour commensal bacterial colonisation and inhibit pathogenic bacterial colonisation in the gastrointestinal tract. They increase the immunoglobulin A response in the mucosal lining of the gastrointestinal tract and have been reported to both improve enteral nutrition tolerance and modulate immune responses [1–3]. The World Health Organization defines probiotics as ‘live microorganisms that, when ingested in sufficient amounts, confer a health benefit on the host’ [4].
Premature infants are very prone to feeding intolerance due to their immature gastrointestinal function and the incomplete establishment of intestinal flora. Symptoms such as vomiting, abdominal distension, and gastric retention occur during feeding, seriously interfering with normal development and prolonging hospitalisation [5, 6]. It has long been believed that probiotics are beneficial for feeding intolerance, although a few randomised clinical trials have evaluated their effects, and data supporting their effects, especially in the treatment of feeding intolerance in preterm infants, are limited. In addition, the evidence for comparisons between probiotics and placebos or other laxatives is sparse and of poor quality [7, 8].
Lactobacillus reuteri DSM 17938 is a gram-positive bacterium that resides naturally in the gut of mammals. It was first described in the early 1980s and has been used safely in both infants and adults [9]. Lactobacillus reuteri DSM 17938 has been shown to reduce feeding intolerance and sepsis and shorten hospitalisation [10–14].
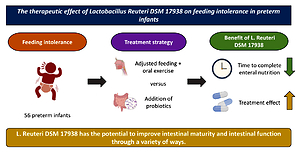
Preclinical studies have shown that this probiotic improves gut microenvironment dysbiosis and promotes gastrointestinal motility by interacting with intestinal mucosal cells [15]. This study aimed to observe the therapeutic effect of L. reuteri DSM 17938 on feeding intolerance in premature infants.
Material and methods
Study design and population
This study included 56 premature infants who were delivered in our hospital between January 2016 and May 2022 and admitted to the NICU. These premature infants were clinically diagnosed as having premature infant feeding intolerance and were divided into scheme A and scheme B according to the treatment method. Those in treatment scheme A received conventional treatment, while those in scheme B were supplemented with L. reuteri DSM 17938 on the basis of scheme A.
Inclusion criteria: With reference to the Clinical Diagnosis and Treatment Guidelines for Feeding Intolerance in Preterm Infants (2020) [16], all premature infants met the diagnostic criteria for feeding intolerance in preterm infants.
Exclusion criteria: (1) use of probiotics and other drugs before treatment, (2) family history of premature infants, (3) serious congenital diseases and (4) the outcome was death.
This study has been approved by the Ethics Committee of Beijing United Family Hospital (2022-03-008-k08). Written informed consent was obtained from all participants. All the families of the included premature infants signed an informed consent form. During the selection process, there were no serious congenital diseases or deaths in our centre.
Sample size calculation
The sample size for this study was estimated based on the formula for comparing two independent proportions using a two-tailed α of 0.05 and a power (1−β) of 0.80. Considering possible randomisation failures, a conservative 10% nonadherence factor was included in the sample size calculation using the method described by Lacin [17]. Based on these assumptions, at least 25 infants per group were required, which, considering a 10% loss-to-follow-up rate, were ultimately determined to include 28 infants in each scheme, with a total of 56 infants.
Methods
Conventional treatment scheme
Those in treatment scheme A were given conventional treatment and breast milk or powdered formula for premature infants (amino acid powder or deeply hydrolysed protein formula powder for severe feeding intolerance). The principles of micro-feeding and intermittent feeding were followed. To prevent overfeeding of the premature infants, a slow increase rate of 10–20 ml/kg per day was used. At the same time, oral exercise interventions, including non-nutritive sucking and oral massage, were used, and the feeding amount was increased gradually with the improvement in tolerance. Treatment was given continuously until discharge.
Oral exercise interventions:
(1) Non-nutritive sucking: By placing a dummy in the mouth of the preterm baby, the process of sucking or chewing on the dummy was induced. Sterile cotton was stoppered inside the dummy, preventing the infant from drawing in too much air and causing gastrointestinal discomfort and other conditions.
(2) Oral massage: Wearing sterile gloves, massage was conducted in the following order: left and right cheeks (the cheek was massaged from the earlobe to the corner of the mouth for 2 min), the upper lip (massaged from the centre of the nasal floor to the centre of the lips, right massage from the nasal floor to the upper right of the lips and left massage from the nasal floor to the upper left of the lips for 1 min), the lower lip (massaged from the centre of the upper gum to the centre of the lip, from the right of the mentum to the lower right of the lip and from the left of the mentum to the lower left of the lip for 1 min), the tongue (massaged from the hard palate to the soft palate on the front and from the middle of the upper gum to the middle of the mouth) and the palate (massaged from the middle of the upper gum to the left and right corners of the mouth for 1 min). For perioral massage, all of the mobile index finger was completed. For massage inside the mouth, all the mobile little fingers were completed. All the massage procedures were repeated three times.
Conventional treatment combined with probiotic treatment
Those in scheme B were given specific probiotics on the basis of scheme A. When feeding, L. reuteri DSM 17938 was added to powdered formula or breast milk (a few children with severe feeding intolerance were given amino acid powder or deeply hydrolysed protein formula powder) at a rate of five drops every day. Treatment was given continuously until discharge.
Both groups were followed up by telephone for 3 to 6 months after discharge.
Observation indicators
The treatment effect was evaluated by comparing the duration of vomiting and the duration of full enteral feeding (all fluids and nutrition were administered orally) between the two groups.
Statistical analysis
A statistical analysis of the data was performed using SPSS 26.0 software (IBM Corp. Silicon Valley, CA, USA). For continuous data with a normal distribution and homogeneity of variance, a parametric test (an independent-samples t test) was used for comparisons between the two groups and expressed as mean ± standard deviation; for non-normally distributed data, a Mann-Whitney U test was used for comparisons between the two groups. The median and quartile values were determined; categorical data count data were analysed using the χ2 test or Fisher’s exact test and expressed in terms of frequency (rate). Differences were considered statistically significant when p < 0.05 for a two-sided test.
Results
Baseline data and overall population analysis
As shown in Table I, there were 28 cases in scheme A, including 18 male and 10 female infants; the gestational age was 31.35 ±3.22 weeks, and the birth weight was 1,569.46 ±529.66 g. There were 28 cases in scheme B, including 13 male and 15 female infants; the average gestational age was 32.64 ±3.11 weeks, and the birth weight was 1,793.57 ±497.80 g. The baseline data of the two schemes were compared, and no significant difference was found (p > 0.05). In addition, there were 8 premature infants under 28 weeks, 48 premature infants over 28 weeks, 19 premature infants with a birth weight of less than 1,500 g and 37 premature infants with a birth weight of more than 1,500 g.
Table I
General data analysis
Among these subgroups, the gender, gestational age and birth weight of the premature infants in schemes A and B were compared, and it was found that the baseline data of the two treatment groups were also comparable between subgroups, with no significant difference (all p > 0.05). For the total population, as shown in Table II, compared with scheme A, the addition of L. reuteri DSM 17938 in scheme B significantly reduced the duration of vomiting (5.0 (3.0–12.5) days vs. 14.5 (5.5–25.8) days) and the time to reach total parenteral nutrition (14.0 (7.0–19.8) days vs. 30.5 (15.0–55.0) days). The differences were statistically significant (p = 0.005 and p = 0.013, respectively).
Table II
Observational metrics analysis
| Index | Whether to add probiotics | t/Z-value | P-value | |
|---|---|---|---|---|
| Yes | No | |||
| Total population, n | 28 | 28 | ||
| Vomiting time [days] | 5.0 (3.0, 12.5) | 14.5 (5.5, 25.8) | –2.434 | 0.015* |
| Time to reach full enteral feeding [days] | 14.0 (7.0, 19.8) | 30.5 (15.0, 55.0) | –2.957 | 0.003** |
| Under 28 weeks, n | 3 | 5 | ||
| Vomiting time [days] | 27.7 ±1.6 | 36.0 ±6.9 | –1.305 | 0.240 |
| Time to reach full enteral feeding [days] | 49.3 ±4.0 | 65.4 ±8.4 | –3.032 | 0.023* |
| 28+ weeks, n | 25 | 23 | ||
| Vomiting time [days] | 4.0 (3.0, 10.0) | 12.0 (3.0, 21.0) | –2.283 | 0.022 |
| Time to reach full enteral feeding [days] | 13.0 (7.0, 17.5) | 17.0 (11.0, 53.0) | –2.621 | 0.009 |
| Below 1500 g, n | 6 | 13 | ||
| Vomiting time [days] | 21.0 (6.0, 49.5) | 26.0 (19.0, 32.5) | –0.132 | 0.895 |
| Time to reach full enteral feeding [days] | 46.5 (37.8, 50.8) | 55.0 (53.0, 62.0) | –2.638 | 0.008** |
| Above 1500 g, n | 22 | 15 | ||
| Vomiting time [days] | 3.5 (2.8, 7.0) | 10.0 (3.0, 14.0) | –1.455 | 0.146 |
| Time to reach full enteral feeding [days] | 11.5 (7.0, 15.5) | 15.0 (8.0, 17.0) | –1.420 | 0.156 |
Below 28 weeks
A total of eight premature infants with a gestational age of below 28 weeks were divided into group A (n = 5) and group B (n = 3). Compared with those in group A, those in group B had a significantly shorter time to reach full enteral feeding after supplementation with L. reuteri DSM 17938 (49.3 ±4.0 days vs. 65.4 ±8.4 days, p = 0.023). There was no statistically significant difference in the time to vomiting (27.7 ±1.6 days vs. 36.0 ±6.9 days, p = 0.240).
More than 28 weeks
A total of 48 premature infants with a gestational age of above 28 weeks were divided into group A (n = 23) and group B (n = 25). Compared with those in group A, after supplementation with L. reuteri DSM 17938, those in group B had a significantly shorter duration of vomiting (4.0 (3.0–10.0) days vs. 12.0 (3.0–21.0) days, p = 0.022). The difference in duration of total parenteral nutrition (13.0 (7.0–17.5) days vs. 17.0 (11.0–53.0) days, p = 0.009) was statistically significant.
Below 1,500 g
A total of 19 premature infants with a birth weight below 1,500 g were divided into group A (n = 13) and group B (n = 6). Compared with those in group A, those in group B had a significantly shorter time to reach full enteral feeding after supplementation with L. reuteri DSM 17938 (55.0 (53.0–62.0) days vs. 46.5 (37.8–50.8) days, p = 0.008), but there was no significant effect on vomiting time (26.0 (19.0–32.5) days vs. 21.0 (6.0–49.5) days, p = 0.895).
Above 1,500 g
A total of 37 premature infants with a birth weight above 1,500 g were divided into group A (n = 15) and group B (n = 22). Compared with those in group A, in the group B who were fed with L. reuteri DSM 17938, the duration of vomiting (3.5 (2.8–7.0) days vs. 10.0 (3.0–14.0) days, p = 0.146) did not show significant statistical significance. Similarly, there was no significant improvement in the time to reach full enteral feeding (11.5 (7.0–15.5) days vs. 15.0 (8.0–17.0) days, p = 0.156).
Discussion
This study mainly explored the therapeutic effect of L. reuteri combined with conventional strategies on feeding intolerance in preterm infants, and the main findings were as follows: (1) In the whole population, compared with conventional strategies, treating the preterm infants with feeding intolerance significantly reduced the duration of vomiting and the time to achieve full enteral feeding. (2) For premature infants with a gestational age of more than 28 weeks, supplementation with L. reuteri DSM 17938 significantly reduced the duration of vomiting and the time to reach full enteral feeding compared with using conventional strategies, but for premature infants with a gestational age of below 28 weeks, supplementation with L. reuteri DSM 17938 only reduced the time to reach full enteral feeding. (3) For premature infants with a birth weight of less than 1,500 g, compared with using conventional strategies, supplementation with L. reuteri DSM 17938 significantly reduced the time to reach full enteral feeding without affecting the duration of vomiting. For premature infants with a birth weight above 1,500 g, supplementation with L. reuteri DSM 17938 did not have an impact on the time to reach full enteral feeding or the duration of vomiting compared to using conventional strategies.
The novelty of this study is that the use of specific probiotics can shorten the time to complete enteral nutrition without adverse reactions. Lactobacillus reuteri DSM 17938 is expected to be an effective strategy for the treatment of feeding intolerance in premature infants and can help children return to normal feeding as soon as possible.
Preterm infants are live infants born at a gestational age of below 37 weeks, and most have a birth weight of less than 2,500 g. Compared with full-term infants, the organ functions and the adaptability of preterm infants are poor. To improve the survival rate, special care is required. Feeding intolerance in premature infants refers to the occurrence of milk indigestion disorders after enteral feeding, resulting in abdominal distension, vomiting, gastric retention, etc. There are many reasons for feeding intolerance in premature infants, mainly physiological; some of the feeding intolerances in such infants are caused by certain diseases, such as necrotising enterocolitis and sepsis [17]. The clinical treatment of feeding intolerance in premature infants is mostly conservative. A series of comprehensive nursing intervention measures were implemented as soon as possible, including breastfeeding, early micro-feeding, non-nutritive sucking, adjustment of body position and laxatives; however, the effect was not good, and the children still grew slowly.
The microbes that live in the gut constitute a huge ecosystem, and the interaction between these gut microbes and the host may affect a variety of diseases. Most commercially available probiotic products are derived from food, especially fermented dairy products. The variety of such microorganisms is still growing and includes strains of lactobacilli, such as Lactobacillus and Bifidobacterium, and non-pathogenic strains of Escherichia coli, such as E. coli Nissle 1917, Clostridium butyricum, Streptococcus salivarius and Saccharomyces boulardii [18]. The intestinal flora of full-term infants can maintain homeostasis between the flora and the host by preventing pathogen colonisation, promoting digestion, improving intestinal barrier function, regulating the immune response and promoting regulation of the gut-brain axis.
The gastrointestinal dysfunction that occurs with feeding intolerance in premature infants destroys the coordination and unity between bacteria in the gut and other bacteria and between bacteria and the host, resulting in microecological disorders of the gut. Premature infants have low intestinal immune function and are extremely sensitive to changes in gut flora. Changes in floral content and diversity and changes in bacterial composition will have a great impact on intestinal function [19, 20]. Lactobacillus reuteri DSM 17938 is one of the first probiotics in the naturally formed microbiota of neonates and can persist in the digestive tract [21]. In 2003, L. reuteri was approved as a probiotic strain for use in health foods according to the Probiotic Health Food Review Regulations; in 2014, an announcement updating the list of strains that can be used in infant food included L. reuteri DSM 17938.
In 2019, Xuewei et al. [22] evaluated the effects of L. reuteri on vomiting, gastric retention, reflux frequency, maximum feeding amount, weight gain, nosocomial infection and occurrence of neonatal necrotising enterocolitis (NEC) in premature infants. Therefore, to evaluate the role of L. reuteri on early feeding tolerance, growth and development, and infection prevention in premature infants. In the study, oral supplementation with L. reuteri DSM 17938 improved feeding tolerance in preterm infants, shortened hospital stays and accelerated growth and development (length, weight and head circumference were monitored). Oncel et al. [23] found that L. reuteri DSM 17938 could significantly reduce the incidence of sepsis in very-low-birth-weight infants with a gestational age of < 32 weeks.
In the present study, there was a statistically significant difference in the time to reach full enteral feeding in the subgroup with a gestational age of ≤ 28 weeks (8 cases in total), indicating that L. reuteri DSM 17938 can improve the enteral nutrition status of patients with a gestational age of ≤ 28 weeks. Regarding the clinical efficacy of feeding intolerance in preterm infants, that is, ultra-premature infants, considering that there was only a small number of participants, we will include more samples for analysis in future studies to obtain more valuable conclusions. There was no significant difference in the duration of vomiting or the time to reach full gastrointestinal nutrition in the group with a weight of > 1,500 g, which was considered to be closely related to the low incidence of feeding intolerance in large premature infants. There was no statistically significant difference in the length of vomiting in the group with a body weight of ≤ 1,500 g. Considering that vomiting is related to various factors, such as gastroesophageal reflux, there was a statistically significant difference in the time to achieve total gastrointestinal nutrition, which confirms that the use of L. reuteri DSM 17938 can improve the clinical efficacy of feeding intolerance in very-low-birth-weight infants. The group with a gestational age of > 28 weeks had statistically significant differences in the duration of vomiting and the time to reach full enteral feeding, which confirms that the use of L. reuteri DSM 17938 on the basis of general treatment can improve the clinical efficacy of feeding intolerance in premature infants. This is because there is no close relationship between feeding intolerance and intestinal flora in premature infants.
The appropriate administration of intestinal probiotics can regulate intestinal flora, help digestion and absorption and solve the problem of gastrointestinal intolerance. Lactobacillus reuteri DSM 17938 has anti-microbial and anti-toxin effects, will not be destroyed by gastrointestinal fluid and other antibacterial drugs after consumption, is safe, and there is no concern over it causing serious adverse reactions when used in premature infants [24]. As a common microbial preparation, L. reuteri DSM 17938 can promote the growth and reproduction of normal microflora, regulate intestinal function and rapidly establish intestinal microecological balance [25].
This study has certain limitations. First, it was a single-centre small-sample study. Although the baseline data of children between the two schemes were comparable, the results of the study may have been affected by selection bias. Large-sample multi-centre randomisation is required in the future. A controlled study was conducted to verify the results of this study. Second, the initial design of this study had certain flaws, as it focused only on the duration of vomiting and the time to reach full enteral feeding. In future studies, we will include more analytical factors, such as the incidence of infection, the incidence of NEC, and long-term growth and development, and include more samples for analysis. Finally, the follow-up time of this study was short; therefore, the follow-up will continue in the future to observe the long-term efficacy of continuous probiotic supplementation.
In conclusion, L. reuteri DSM 17938 combined with the routine treatment of premature infants with feeding intolerance has a better effect. Returning to normal feeding as soon as possible can reduce the incidence of gastrointestinal complications and promote growth in preterm infants.