Introduction
Amyotrophic lateral sclerosis (ALS) is a progressive neuromuscular disease that causes skeletal muscle weakness, including muscles involved with respiration. Amyotrophic lateral sclerosis belongs to a group of neurological diseases, and affects the upper and lower motor neurons. It is one of the most common motor neuron diseases, and can occur individually or as a hereditary family illness. The most common cause of death in these patients is respiratory failure, often in the period of 2–5 years, with a small percentage of patients surviving up to 10 years and more. Accordingly, monitoring respiratory status is critical to ALS management. Pulmonary function tests (PFTs) are used for evaluation of respiratory impairment and decision-making including the timing of noninvasive ventilation. Recognizing different respiratory tests in relation to disease progression and survival may help determine which tests are most suitable [1].
Poor prognosis and decreased survival time of patients with ALS correlate with their nutritional status. Various studies have evaluated weight, body mass index (BMI), survival time and ALS Functional Rating Scale-Revised (ALSFRS-R) in order to determine the best nutrition management methods for this patient population [2].
The aim of the study was to determine the significance of pulmonary function tests in prediction of mortality and define indications for noninvasive mechanical ventilation (NIMV).
Material and methods
This cross-sectional retrospective study was performed at the Clinic of Pulmonology, Clinical Centre of Serbia in the period from January 2015 to December 2017. Approval granted by the local ethics committee was not required. Patients with a diagnosis of ALS established according to El Escorial criteria were included [3]. The diagnosis of disease was made at the Clinic of Neurology, Clinical Centre of Serbia.
The following PFTs were performed in all patients: spirometry, impulse oscillometry, maximal inspiratory and expiratory mouth pressures, and arterial blood gases analysis. Spirometry was performed by means of a Lilly’s pneumotachometer (MasterScreen Pneumo, Viasys Healthcare, Germany), impulse oscillometry and maximal inspiratory and expiratory pressures (PImax and PEmax) at the mouth during occlusion were performed using commercial systems (MasterScreen IOS, Viasys Healthcare, Germany, and MasterScreen Body, Viasys Healthcare, Germany, respectively). The analysis of the arterial blood gasses was also performed on a commercial analyzer (ABL5, Radiometer, Denmark). All PFTs were performed according to European Respiratory Society/American Thoracic Society joint recommendations [4–8].
Informed consent was not obtained because all study procedures were routinely performed in all patients with ALS at our clinic.
The current criteria for assigning the noninvasive mechanical ventilation (NIMV) in our country are forced vital capacity (FVC) less than 50% of the predicted, and global respiratory failure or elevated bicarbonate levels (more than 27–28 mmol/l) in arterial blood gases analyses. The criteria were determined by the Republic Fund of Health Insurance, which has been providing non-invasive mechanical ventilation devices for home treatment to insured persons since 2007. Since that time, these criteria have been widely accepted as indications for home ventilation in our country.
Blood samples were collected from patients for laboratory analysis (urea (normal values 2.5–7.5 mmol/l), creatinine (normal values 45–84 μmol/l), creatine kinase (CK) (normal values 0–150 U/l), CK-MB (normal values < 25 U/l)); all tests were performed in an Accredited Medical Laboratory, ATC03-001, SRPS EN 150 15189-2014.
Primary outcome was the time from diagnosis to the establishment of indications for NIMV, as well as the secondary outcome – the time from diagnosis to death.
The outcome was determined by direct contact with patients or their families during regular clinical visits or by telephone contact or with family members when returning the NIMV device.
Statistical analysis
Descriptive statistics was calculated for the baseline demographic and clinical features. Normality of distribution was tested using graphical and mathematical methods. Continuous variables were presented as means with standard deviations or median with 25th–75th percentile, if required. Categorical variables were reported in numbers and percentages. Differences between groups were analyzed using Student’s t-test for normally distributed continuous variables or the Mann-Whitney test for non-normally distributed continuous variables and Pearson’s χ2 test for categorical variables.
Survival was computed by means of Kaplan-Meier survival analysis, and two groups were compared using the log-rank test. Cox-regression analysis was used to determine factors influencing survival. The level of significance was set at 0.05. Statistical analysis was performed using the IBM SPSS 21 (Chicago, IL, 2012) package.
Results
The clinical characteristics of patients are presented in Table I. The study included 76 patients with ALS, 50 (65.8%) with spinal and 26 (34.2%) with bulbar form of disease. There was no difference in age, gender or BMI between these two groups. Forced vital capacity and forced expiratory volume in 1 s (FEV1) were higher in spinal form of ALS, and the difference was statistically significant when compared to bulbar form. There was no difference in R5HZ, R20HZ, PImax or PEmax between the groups. Laboratory parameters – urea, creatinine and creatine kinase (CK) – did not differ between the groups. CK-MB was higher in spinal form, and the difference was statistically significant in comparison with bulbar form.
Table I
Clinical characteristics of amyotrophic lateral sclerosis patients
| Factor | Spinal n = 50 Mean ± SD | Bulbar n = 26 Mean ± SD | P-value |
|---|---|---|---|
| Age | 54.3 ±8.3 | 53.9 ±10.2 | 0.870 |
| Sex (male)* | 26 (52.0%) | 10 (38.5%) | 0.262 |
| BMI | 25.7 ±6.6 | 27 ±8.5 | 0.484 |
| FVC | 93.8 ±31.2 | 78.7 ±26.7 | 0.039 |
| FEV1 | 94.6 ±32.2 | 77.4 ±27.9 | 0.024 |
| R5HZ | 83.4 ±41.8 | 93.3 ±43 | 0.336 |
| R20HZ | 73.4 ±34.6 | 73.7 ±28.4 | 0.976 |
| PImax | 37.3 ±17.4 | 32.6 ±12.1 | 0.173 |
| PEmax | 39.7 ±25.2 | 42 ±25.5 | 0.707 |
| Urea | 5.1 ±1.5 | 5 ±1.4 | 0.832 |
| Creatinine | 58.6 ±15.9 | 58.6 ±19.7 | 0.997 |
| CK | 153.5 ±60.4 | 131.8 ±55.8 | 0.131 |
| CK-MB | 4.6 ±1.3 | 4 ±1.3 | 0.047 |
Mean follow-up time was 31.1 (minimum–maximum 2.0–81.0) months. Overall median survival was 32.0 (95% CI: 28.1–35.9) months from ALS diagnosis to outcome.
A non-invasive ventilation machine (NIVM) was introduced after a median of 23.0 (12.0–31.0) months in spinal and 13.5 (8.0–23.0) months in bulbar form of disease (p < 0.05).
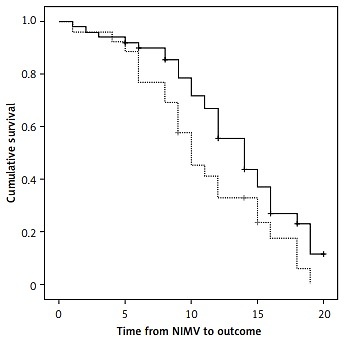
Median survival from NIMV introduction to outcome was 12.0 (95% CI: 9.98–14.03) months. Median survival from NIMV introduction to final outcome (death) in patients with spinal form was 14.0 (95% CI: 11.36–16.64), and 10.0 (95% CI: 7.64–12.35) months in patients with bulbar form of disease (Figure 1). According to the log-rank test, this difference was statistically significant (p < 0.05).
Median survival from diagnosis to final outcome (death) in patients with spinal form was 37.0 (95% CI: 29.74–44.26) months, and 25.0 (95% CI: 20.20–29.80) months in patients with bulbar form of disease (Figure 2). According to the log-rank test, this difference was statistically significant (p < 0.05).
Figure 2
Survival from amyotrophic lateral sclerosis (ALS) diagnosis between the spinal and bulbar form

Cox-regression analysis was performed to determine the effect of pulmonary function parameter values recorded at the time of making the ALS diagnosis to survival, the results being presented in Table II.
Table II
Factors influencing survival at the time of amyotrophic lateral sclerosis diagnosis
Form of disease, FVC < 70%, PImax < 50 and PEmax < 50 were significant factors for survival. R20HZ < 120 and R5HZ < 120 were not significant factors for survival in patients with ALS. The patients with bulbar form of disease had 2.17 (95% CI: 1.26–3.75) higher risk for death. The patients with FVC < 70% of disease had 1.94 (95% CI: 1.02–3.71), PImax < 50 and PEmax < 50 1.96 (95% CI: 1.01–3.77) higher risk.
Discussion
Our study showed that the patients with FVC less than 70% at the time of making their diagnosis as compared to the expected values carried two times higher risk of a lethal outcome. In addition, it was noted that the values of PImax and PEmax lower than 80% in relation to the expected values represented a twice-higher risk of lethal outcome. On the other hand, impulse oscillometry parameters did not show any significant association with the length of survival of these patients.
A large number of former cross-section studies have pointed to FVC limitations in detecting an early respiratory dysfunction. It is questionable whether the employment of the FVC value is a relevant criterion as well as whether its value should be confined to the decision on timely application of NIMV [9–12]. In the study by Gordon et al., 50 patients having required tracheotomy underwent spirometry tests and their FVC values were recorded 30 days prior to the aforesaid event; FVC was 50% of the expected value or higher in 11 patients, 60% of the expected value or higher in 7 patients and 70% of the expected value or higher in 5 patients. All the aforementioned data indicate a possible disadvantage of FVC as a tool for evaluation of patient survival [13].
Longitudinal follow-up of ALS patients by Polkey et al. confirmed that the differences in FVC values showed low amplitudes either until death occurred or need for NIMV appeared, while the values of respiratory muscle tests manifested significant amplitudes; accordingly, it directly suggested that the measurement of respiratory muscle strength could be a more beneficial marker for assessing the most optimal timing of NIMV application [14].
Forced vital capacity values during the maneuver of spirometry testing with the patient assuming a recumbent position designated the preservation of diaphragmal musculature strength. Lechtzin et al. recommended applying NIMV in all patients with FVC < 70% recorded during spirometry in a lying position [12]. Polkey et al. underlined the inferiority of the FVC value in ALS patients. This study pointed to worse prognosis in patients whose value of this parameter was even higher than 80% and in whom the NIMV was not started yet [14–16].
Measurement of the maximum static inspiratory pressure that a subject can generate at the mouth (PImax) or the maximum static expiratory pressure (PEmax) is a simple way to gauge inspiratory and expiratory muscle strength. The pressure measured during these maneuvers reflects the pressure developed by the respiratory muscles (Pmus), plus the passive elastic recoil pressure of the respiratory system including the lung and the chest wall (Prs) [17–21].
When respiratory muscle weakness occurs, PImax can be more sensitive than VC because the relationship between VC and PImax is curvilinear, so that decreases in respiratory muscle strength which develop before decreases in lung volume can be identified [22, 23].
Different studies have confirmed that the strength of respiratory muscles is one of the more significant prognostic markers in ALS patients; a recent study has underscored the need for adequate physical rehabilitation for musculature strengthening. The research studies suggest that this program of respiratory physical rehabilitation is well tolerated and leads to improvement of respiratory and bulbar functions [16].
During routine pulmonary function testing of ALS patients, it has been noted that some of them have elevated R20 and R5. Our study, however, did not find any correlation between the values of impulse oscillometry and time of survival of ALS patients (p = 0.488 for R20Hz and p = 0.181 for R5Hz), in spite of our high expectations that the patients with higher values of extrathoracic and intrathoracic airways resistance would have shorter time of survival. It is particularly true if we inspect the results suggesting that the time of survival in patients with bulbar disease is significantly shorter than in patients with the spinal form of the condition. Anyway, these results call for additional research in future as well as an analysis of the potential prognostic significance of airway resistance.
Presently recommended Medicare criteria (a federal government website managed and paid for by the U.S. Centers for Medicare & Medicaid Services) for NIMV application in ALS patients include any of the following: FVC < 50% of the expected, SAT O2 < 88% during at least 5 min, and PaCO2 44 mm Hg. Upon updating the American Academy of Neurology Database, two additional criteria were added, sniff nasal inspiratory pressure (SNIP) < 40 cm H2O and orthopnea, which may justify the introduction of noninvasive ventilation. In our country, the criteria of providing home care NIMV are FVC < 50% of the expected, and global respiratory insufficiency with HCO3 > 28 mmol/l obtained from arterial blood gas analysis. The study by Vitaca et al. revealed that the NIMV, in the Italian pulmonological units, was introduced in patients with neuromuscular conditions in case of diurnal hypercapnia, nocturnal desaturation and FVC < 50% of expected. Nevertheless, a large number of centers take the position that mere presence of symptoms such as dyspnea or orthopnea are adequate criteria for starting the ventilation [24].
The above result is immensely significant given that, in our country, the indication for NIMV application is FVC below 50%. But, our results demonstrate that FVC is a powerful predictive factor.
Our study has several limitations. First of all, measurement of maximal SNIP was not performed in our patients due to lack of equipment. SNIP has been shown to be strongly correlated with maximal sniff oesophageal pressure [25], is well established as a non-invasive method for assessing inspiratory muscle strength [26], and its values better correlate with onset of respiratory failure than FVC [27]. Next, SVC measurement was also not performed in our patients, despite the fact that change in SVC predicts respiratory failure or death in patients with ALS [28]. Similarly, nocturnal hypoventilation, known to be associated with poor prognosis, has not been studied in this analysis, in spite of the fact that an increasing number of experts nowadays believe that nocturnal hyperventilation is an indication of NIMV [18]. Finally, other prognostic factors in ALS, such as delay from symptom onset to diagnosis [29], progression rate of revised ALS Functional Rating Scale (ALSFRS-R) score [30], psychological distress [31], and frontotemporal lobar dementia [32], were not taken into account. All these factors, and several more, strongly affect quality of life and have an influence on survival of patients with ALS. A couple of prognostic scores based on mentioned and other parameters were developed for patients with ALS [33, 34]. Excluding these factors from our analysis could potentially have an influence on the results of this study, despite the fact that decline in lung function, measured primarily by FVC [35–37], is a strong independent prognostic factor in ALS.
The increasing number of clinicians and the authors of scientific and research papers agree on the fact that the sequential diagnostic procedures, especially if used in combination with sophisticated techniques as described by Carreiro et al., could offer an alternative predictive strategy [17].
In conclusion, our study points to the significance of timely application and early start of NIMV in patients with ALS as an important approach to defer functional impairment, which would mean that the criteria, in our country, for application of these devices must be changed, not only regarding the value of current functional diagnostic tests used in everyday practice in patients with ALS but also in regard to the introduction of new diagnostic tests, such as SNIP and/or polysomnographic testing.