Chin augmentation is a major facial aesthetic surgery [1–3], which generally concerns 2 different kinds of incisions; namely, the intraoral approach and the extraoral approach. The extraoral approach is relatively less employed in China due to its detriment of leaving scars on submental skins [4]. The intraoral approach consists of horizontal incision, vertical incision, U-shaped incision, V-shaped incision, etc. [5–9]. Vertical incision (single and bilateral) is currently the most commonly used incision, whereas intraoral horizontal incision, especially horizontal middle incision, is not recommended considering its various disadvantages [5, 6]. On the basis of referring to correlated theses [10] and observation of clinical practices, we have improved the intraoral horizontal incision. Since 2014, we have applied intraoral horizontal middle incision on all mild to moderate micrognathia patients with basically normal occlusion. Satisfactory results have been attained on a total of 122 patients. The process of this technique is presented as follows.
From August 2014 to December 2021 improved chin augmentation with intraoral horizontal middle incision with prosthesis implanting was applied to treat a total of 122 patients, among whom 31 were males and 91 were females, aged 18-50, averaging 26.8 years. Of the 122 patients, 102 involved simple chin augmentations, 4 were combined with rhytidectomy, 7 were combined with face and neck liposuction, and 9 were combined with rhinoplasty. The study was approved by the medical Ethics Committee of the hospital (HWHK20140609). All patients gave written informed consent, especially for the publication of photographs.
Detailed examination and history were recorded. Patients with oral inflammation and obvious malocclusion were excluded, and patients with basically normal occlusal system and simple micrognathia were included. Meanwhile, it is necessary to understand in detail the aesthetic goal of the patients, and whether or not the patient had undergone any previous facial surgery or orthodontic treatment. Routine facial imaging inspection and analysis should be conducted with patients undergoing a secondary surgery.
Malformation classification: The problems of chin dysplasia lie commonly in 2 aspects: lacking prognathism in the horizontal position, and lacking length in the vertical position. Thus, the insufficiency in aesthetics manifests into 3 situations: deficient warp (mandibular retrusion), deficient length (short jaw), or deficiency of both (micrognathia).
Evaluation standard: In accordance with the aesthetic standard of the facial and mental region, if the aesthetic positions of nasion and nasal spine are standardized, the connecting line of the two ought to run through the submental point in a lateral view, hence forming an ideal mental topology [11]. The submental point being posterior to the connecting line will appear as chin retrusion. By this standard, chin retrusion can be classified into 3 categories by its severity: I. Mild, within 1 cm of the ideal position; II. Moderate, approximately 1–2 cm of the ideal position; III. Severe, approximately 2–3 cm of the ideal position, incorporated with significantly reduced frontal area [12]. Additionally, on the principle of the 3 divisions of the face, a harmonious face is divided equally into three parts by 4 lines running respectively through the hairline, supraorbital notch, nasal base, and chin point. While the lower 1/3 of the face can be further divided into the upper 1/3 and lower 2/3, and a shorter length of the lower 1/3 of the whole face than the middle 1/3 will form a short jaw.
Basic principles: Choose the chin prosthesis with a proper thickness in response to the extent of the chin’s retrusion that is assessed in the preoperative evaluation, so that the lengthened chin agrees with the aesthetic standard.
Choose the chin prosthesis with the correct size according to the face type and chin situation of the patient: choose larger ones for patients with sharper and smaller chins. Contrarily, choose relatively small ones for patients with round chins.
Choose the chin prosthesis with an appropriate radian according to the intrinsic radian of the internal side of the prosthesis and the radian of the bone surface on which the prosthesis is to land. Based on the malformation of the chin, there are 2 candidate bone surfaces: the bone surface of the chin that is parallel to the Frankfort horizontal plane, or the most anterior lower bone surface of the chin. The radian of the internal surface of the chosen prosthesis must fit the topology of the selected bone surface.
Make adjustments to the principle in reference to the patient’s own requirements, occupation, personality, and his/her perception of aesthetics.
Preparation of prostheses: The median mark of the prosthesis must be apparent. The margins on both sides must be rendered thin. The transition from the sides to the middle must be natural and streamlined. The main body in the middle can be made sharper and more spherical for female patients and blunter and squarer for male patients. At the same time, it should be noted that the radian of the prosthesis is consistent with the surface morphology of the chin bone.
First, mark the position of the chin midline, the inferior marginal line of the mandible, and the mental foramen; the marked area to be peeled depends on the deficiency of warp and length.
The patient takes a supine position. Sanitize and drape routinely. Conduct local anaesthesia or bilateral mental nerve blockage anaesthesia with 1.0% lidocaine and adrenaline mixture (1/100,000). Mildly massage the injection area. The anaesthetic solution must not be excessive so as not to impede intraoperative observation.
Take the frenulum labii inferioris as the midline, and make a horizontal incision 0.5 cm away from the inferior gingival sulcus. The incision should be about 1.5 cm long, cutting to the submucosa. Then, in the middle of the incision, cut longitudinally to the periosteum with a #11 scalpel, splitting the muscle fibres in accordance with their direction, rendering a double-layer incision, where the external layer is a transverse incision of the mucosa, and the internal layer is an improved transverse incision with muscle longitudinally split (Figure 1). Then peel beneath the periosteum using a pointing-head periosteum elevator. According to the marked area, peel the left side first and then the right side. Afterwards, peel the corresponding mandibular margin (if needed), with the peeled area slightly larger than the prosthesis to be implanted. Meanwhile, avoid injuring the mental nerve, and check if there is active bleeding. If not, prepare to implant the prosthesis. Clip the middle and rear part of the prosthesis with curved pliers. Push the left part of the prosthesis along its prolate axis into the peeled-out cavity on the left. Then fold the right end of the other half of the prosthesis and push it gently in until the prosthesis enters completely. Check carefully whether the prosthesis clings to the bone surface, whether the middle point matches the midline of the marked skin area, and whether folding or twisting has occurred. Afterwards, make a further inspection of whether or not the prosthesis is in its designated position and properly fixed. Having made sure there is nothing unexpected, mildly squeeze the cavity to expel any possible liquid. Suture the longitudinally cut muscle with 3.0 silk thread, and then the transverse mucosa incision (Figure 2).
Postoperative treatment: The external dressing on the chin should be pressed and fixed with wide adhesive tape for 3–5 days (or not), oral antibiotics should be taken to prevent infection, a liquid diet taken for 3–5 days, chlorhexidine gargle used for gargling 3 times a day, and the suture removed 1 week later.
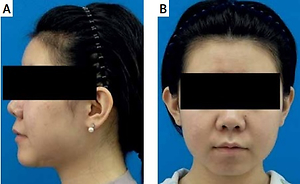
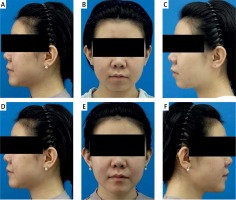
In all 122 patients, the local swelling was mild after operation, which subsided within 2 weeks. There were no complications such as postoperative infection, delayed wound healing, obvious deviation of prosthesis, and numbness of the lower lip. Forty cases were followed up for a long time. The longest follow-up time was 3 years and the shortest was 3 months. No displacement and exposure of prosthesis were found, and the effect was satisfactory (Figure 3).
Figure 3
Surgical results following chin augmentation in a 24-year-old woman. A–C – frontal view and lateral view before operation, D–F – frontal view and lateral view 6 months after operation
The correct proportions of the chin are vital to the harmoniousness of the face. As facial topology gains more and more attention from modern people, the distinctive facial shape and personality characteristics of the chin make it particularly prominent. Therefore, chin surgery is receiving more and more attention.
Chin augmentation is a relatively common aesthetic surgery, which in itself is not a complicated surgery, but if not properly operated or with flawed operation design, there can be complications [4] such as postoperative prosthesis drifting, labial suture disappearance, varus of the lower lip, infection, scar formation, etc. Additionally, a majority of scholars [5–7] believe that the occurrence of complications has a certain causal relation with the choice of the incision. Thus, as far as chin augmentation is concerned, optimization of the incision is decisive, and hence to which we shall give due consideration.
We believe that an ideal chin augmentation surgery must possess the following features: 1. The incision must be as small as possible, with as little damage as possible. And when it comes to important anatomical structures, especially important muscles such as the musculus mentalis, care should be taken to avoid damage. 2. It is convenient to observe the position that the prosthesis is implanted and to operate in the surgery; 3. Not only can it help maintain normal configuration of the chin, avoiding swirl malformation and mandible prolapse, etc., but it also prevents scar formation and other situations that hamper the functionality of the lower lip. In short, the determination of the incision must be reasonable, which must comply with standard anatomy and physiology, as well as the basic principles of plastic surgery.
In standard anatomy and physiology of the chin and lower lip, there are 3 pairs of muscles that concern chin augmentation surgery with an intraoral approach: the musculus depressor anguli oris, the musculus quadratus labii inferioris, and the musculus mentalis, of which the musculus mentalis holds specific significance. The musculus mentalis comprises 2 paired muscles located at the interior surface of the musculus quadratus labii inferioris. The musculus mentalis originates from the incisor alveolar sockets on both sides of the midline of the mandibula. Their muscle fibres run longitudinally; the upper parts approach and merge with fibres from the other side when nearing the midline, and the lower parts run obliquely down and ends at the skin of the lower lip. The musculus depressor labii inferioris is sometimes referred to as the asmusculus quadratus labii inferioris. It originates from the oblique line of the mandible and ends with the skin of the lower lip, the fibres of which are interwoven with those of the musculus orbicularis oris. The musculus depressor anguli oris, also named the deltoid muscle of the lower lip, originates from the same oblique line. It is located inferior to the musculus depressor labii inferioris and ends with the skin of the corners of the mouth. All 3 muscles bear the same function, i.e. lowering the lower lip and lifting the chin’s skin [10].
Traditional chin augmentation with an intraoral horizontal middle incision enjoys the advantages of clear exposure of the surgical area and easy input of the prosthesis [13, 14]. However, it requires complete severance of the musculus depressor anguli oris, the musculus quadratus labii inferioris, and the musculus mentalis, so as to make the direction of the stress that the incision bears the same as that of the implanted prosthesis. In addition, the incision is in the most low-lying position of the vestibulum oris, where oral secretions and food residues tend to cumulate, which will undoubtedly soak and contaminate the incision, thus making it difficult for the incision to heal firmly and tightly. All the above lead to complications such as the upward drifting of the prosthesis, incision dehiscence, infection, scar formation, etc.
In response to the disadvantages of the traditional incision, improved chin augmentation with intraoral horizontal middle incision bears the following characteristics: 1. Complying with standard anatomy and physiology – the improved incision fully respects the physiological structure and the functionality of the important structures of the chin and the lower lip, with minimal damage to the musculus mentalis and the middle tissues of the lower lip, ensuring effective wrapping around the prosthesis and preventing the prosthesis from drifting. The 2 layers being designed vertical to each other effectively avoids the tensions that the implanted prosthesis might cause to the incision, as well as the possible entrance of food and other oral contents, which not only makes for faster healing of the incision but also prevents infection. 2. Respecting the principles of minimally invasive and non-invasive surgery. The horizontal incision only concerns the mucosa and submucosa, while the vertical incision splits the muscles according to its original fibre direction, causing no transverse-cut damage of the muscle, which is to say, no unnecessary tissue damages. Moreover, the design of the incision ensures that all the peeling procedure is undertaken bluntly in the sub-periosteum cavity, reducing possible damage to the interior of the muscle tissues, which further decreases the occurrence of complications [15] such as postoperative haematoma, chin skin wrinkling, lower lip deformation, etc., which stands in line with basic principles of plastic surgery. 3. The operation is more convenient and effective. The improved horizontal middle incision inherits the merits of traditional horizontal incisions, at the same time surmounted the disadvantage of insufficient sight of vertical incisions, acquiring minimized operation distance, optimized sight, and making it very convenient to check on the position of the prosthesis, hence guaranteeing the symmetry of the implantation. Based on the above advantages, we assume that the improved horizontal middle incision can avoid the complications in previous operations and improve the surgical effect, and this is also confirmed through our clinical practice.
In conclusion, improved chin augmentation with horizontal middle incision can effectively reduce and prevent the occurrence of complications. It was well validated in our clinical practice, and satisfactory clinical results were obtained.