Approximately 85 million red blood cell (RBC) units are transfused globally every year, with 12–16 million transfused in the United States alone [1]. The utilization of RBC is expected to grow due to the increasing number of surgical procedures performed and the aging population. At the same time, the shortage of blood donors is becoming a growing global problem.
Transfusion of RBC is not devoid of risks. Typical risks include: alloimmunization, hemolytic reactions, iron overload, transfusion-associated lung injury, transfusion-associated circulatory overload, prolonged mechanical ventilation, increased risk of infections, acute kidney injury, thromboembolic complications, prolonged hospitalization, and increased mortality [2]. At the same time anemia increases the risk of myocardial ischemia, stroke, acute kidney injury, and infection [3]. Therefore the decision regarding RBC transfusion requires careful assessment of the risk-benefit balance between anemia and RBC transfusion. This difficult decision constitutes a daily challenge to ordering physicians.
In clinical practice RBC transfusion should be the treatment of last resort, reserved for massively bleeding patients. Rather than relying on symptomatic treatment through RBC transfusion, clinicians should investigate the etiology of anemia and provide causal treatment. Causal treatment of anemia is one of the pillars of a strategy called Patient Blood Management (PBM). This strategy involves optimizing the body’s endogenous RBC mass by stimulating erythropoiesis and addressing treatable underlying conditions; minimizing blood loss during procedures (diagnostic, interventional, surgical); and ensuring patient-specific tolerance to anemia by strictly following physiological transfusion thresholds [4].
Reaching a decision regarding RBC transfusion is frequently complicated; therefore implementation of a hospital program facilitating RBC transfusion decision making is advisable.
The aim of the study was to assess the usefulness of an in-house program designed to improve the appropriateness of RBC transfusions in anemic patients hospitalized in our academic medical center.
Methods. We performed a retrospective analysis of all RBC transfusions in adult non-bleeding patients hospitalized in our academic medical center. A dedicated transfusion committee oversees the use of blood components in our center and is responsible for standard operating procedures (SOPs) on issues regarding transfusion medicine. Our SOP was based on the most recent clinical practice guidelines published by the Association for the Advancement of Blood and Biotherapies (AABB) [5]. The appropriateness of RBC transfusions was decided based on Hb concentration and signs and/or symptoms of anemia before transfusion. Anemia symptoms had to be present before transfusion despite attempts to improve the patient’s tolerance to anemia through increased oxygenation and hemodynamic optimization [6, 7]. Increased oxygenation involved oxygen therapy aimed at peripheral oxygen saturation (SpO2) of 100% and/or arterial oxygen saturation (paO2) of 200 mm Hg. Hemodynamic optimization involved assuring satisfactory cardiac output (CO) through manipulation of preload, contractility and afterload. Appropriate RBC transfusion clinical scenarios are summarized in Table I.
Table I
Clinical scenarios in which red blood cell transfusion was classified as appropriate
Our institution adheres to the single-unit transfusion policy [8]. In the case of multiple unit transfusions the appropriateness was assessed for each unit separately, so if there was no re-evaluation of anemia symptoms after the first unit the next one was deemed inappropriate.
We analyzed time periods before and after implementation of the program: January–June 2022 and January–June 2023. The time period July–December 2022 was the implementation phase and encompassed: new SOP informative meetings (approximately 0.5 h each) for physicians in departments where RBC are frequently ordered, obligatory e-learning training for all clinical and laboratory personnel, modification of the existing RBC computerized provider order entry (CPOE) – the general indication “anemia” was replaced with a detailed drop-down menu of appropriate indications for RBC transfusion (Table I) plus additional options: “anemia with Hb < 70 g/l without assessing anemia signs/symptoms (not recommended)”, “anemia with Hb < 70 g/l without anemia signs/symptoms (not recommended)”, and “anemia – other – please state the indication in the additional field”. Red blood cells transfused during bleeding (n = 495) were excluded because in these situations the pre-transfusion Hb concentration is frequently unavailable and the single unit transfusion policy is commonly abandoned. We also excluded RBCs transfused pre- and intraoperatively in non-elective surgery (n = 201) because various Hb concentrations are required by different operators before non-elective procedures and RBC transfusions in the intraoperative period are not elective.
The retrieved data included: age and gender of RBC recipients, signs and symptoms of anemia before transfusion, laboratory markers of anerobic metabolism (central venous oxygen saturation, mixed venous oxygen saturation, blood lactate) before transfusion, Hb concentration up to 24 h before and up to 24 h after RBC transfusion. We also calculated basic transfusion metrics. Transfusion rate was the percentage of patients who received at least 1 RBC. Transfusion incidence was the number of transfused RBCs per 1000 patient-days.
This study was approved by the Ethics Committee of the Medical University of Silesia in Katowice (approval number/protocol number PCN/CBN/0022/KB/292/21). The research was conducted ethically, with all study procedures being performed in accordance with the requirements of the World Medical Association’s Declaration of Helsinki.
Statistical analysis. Licensed software was used for statistical analysis (Statistica 13.3., Cracow, Poland, TIBCO). Continuous variables were presented as median and interquartile ranges (IQR), whereas categorical variables were presented as numbers and frequencies. The distribution of variables was verified with the Shapiro-Wilk test. Variable distributions in both study periods were compared using appropriate tests: the χ2 test for categorical variables, and the Mann-Whitney U test for continuous variables. A p < 0.05 was considered significant. The study was approved by the Ethics Committee of Medical University of Silesia in Katowice (PCN/CBN/0022/KB/292/21).
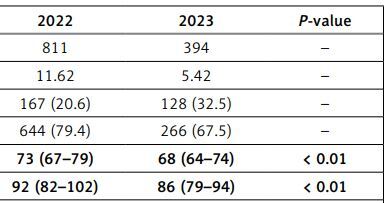
Results. The age of RBC recipients was not different (p = 0.20) before and after program implementation, 65 (IQR: 47–73) and 66 (IQR: 48–74) years, respectively. Before program implementation 415 out of 23492 (1.8%) patients received at least 1 RBC, whereas after implementation 162 out of 25062 (0.6%) patients did so. Transfusion incidence decreased from 11.62 to 5.42 RBC transfusions per 1000 patient-days following implementation of the program. The percentage of appropriate RBC transfusions increased from 23.6 to 37.1%. The percentage of multiple unit RBC transfusions decreased following implementation of the program, but still constituted 67.4%. There was a significant drop in Hb concentration before and after single unit RBC transfusions as well as before multiple unit RBC transfusions after introduction of the program. The characteristics of RBC transfusions in both time periods are presented in Table II.
Table II
Characteristics of red blood cell transfusions before and after program implementation
There was significant year-to-year drop in Hb concentration before inappropriate RBC transfusions, 76 (IQR: 71–82) and 73 (IQR: 68–78) g/l (p < 0.01), respectively. There was also a significant drop in Hb concentration following RBC transfusions in appropriate and inappropriate RBC transfusion categories after implementation of the program, 79 (IQR: 73–90) to 75 (IQR: 67–82) g/l (p < 0.01) and 97 (IQR: 88–104) to 89 (IQR: 84–96) g/l (p < 0.01), respectively (data not shown).
Discussion. In our study we assessed the effectiveness of a simple program designed to improve the appropriateness of RBC use in non-bleeding anemic patients hospitalized at our institution. In our study the transfusion rate was reduced significantly after implementation of the program, from 1.8% to 0.6%, which corresponded to 253 fewer RBC-transfused patients following implementation of the program. These percentages are much lower than those reported in similar studies. Borkent-Raven et al. reported in 2013 that 13.0% of all hospital patients required RBC transfusion [9]. A decreased RBC transfusion rate among hospital patients was observed in the USA following implementation of a national program, where the transfusion rate was reduced from 6.8% in 2011 to 5.7% in 2014 (adjusted relative risk of 0.83) [10].
The utilization of CPOE with clinical decision support (CDS) systems enhances the appropriate use of RBCs in alignment with hospital guidelines [11]. Goodnough et al. demonstrated that the use of the CDS system led to a decrease in RBC transfusions, with pre-transfusion Hb concentrations > 80 g/l dropping from 60% to 30% [12]. Other methods to reduce the number of inappropriate RBC transfusions include education of medical personnel and prospective screening of RBC transfusion orders [13]. After implementation of a transfusion bundle, the number of inappropriate RBC transfusions decreased from 25% to 15% in a medical-surgical ICU [14]. In our institution since December 2022 the CPOE/CDS system has helped clinicians with appropriate ordering of RBCs.
Yerrabothala et al. observed an increase in single-unit transfusions and a decrease in multiple-unit transfusions following implementation of their improvement program [15]. Although the number of multiple transfusions in our study was significantly reduced following implementation of the program, the percentage of multiple-unit transfusions remained high (67.5%). We realized that the previous strategy of transfusing 2 RBC units in a single transfusion episode was difficult to eradicate.
Our study is not devoid of limitations. Because it was conducted retrospectively, we lacked access to some clinical data that may not have been recorded in the patients’ medical records. Even though we extensively reviewed all daily entries, it is possible that symptoms of anemia were not adequately documented by the ordering physicians, potentially leading to incorrect assessments of the appropriateness of some RBC transfusions. This study is also limited by being conducted in a single institution, which restricts the generalizability of its results to other institutions.
In conclusion, a simple strategy of introducing a standard operating procedure adjusted to the local hospital population, backed by in-person and e-learning educational activities, and a minimal change in a CPOE, may lead to a nearly 3-fold decrease in transfusion rate, more than 2-fold decrease in transfusion incidence, and significant increase in the percentage of appropriate RBC transfusions in non-bleeding hospital patients with anemia. Nevertheless, multiple-unit RBC transfusions may still be a problem and warrant further education of ordering physicians.