Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
METABOLIC SYNDROME / CLINICAL RESEARCH
Association between metabolic syndrome and inflammatory bowel disease: a bidirectional two-sample Mendelian randomized study
1
Guangdong Provincial Key Laboratory of Gastroenterology, Department of Gastroenterology, Institute of Gastroenterology of Guangdong Province, Nanfang Hospital, Southern Medical University, Guangzhou, China
2
Yuebei People’s Hospital of Shantou University Medical College, Shaoguan, China
3
Department of Cell Biology, School of Basic Medical Sciences, Southern Medical University, Guangzhou, China
4
Department of Microbiology, Guangdong Provincial Key Laboratory of Tropical Disease Research, School of Public Health, Southern Medical University, Guangzhou, China
These authors had equal contribution to this work
Submission date: 2025-01-25
Final revision date: 2025-07-19
Acceptance date: 2025-08-03
Online publication date: 2025-10-05
Corresponding author
Xiaowei Sun
Guangdong Provincial Key Laboratory of Gastroenterology Department of Gastroenterology Institute of Gastroenterology of Guangdong Province Nanfang Hospital Southern Medical University Guangzhou, China
Guangdong Provincial Key Laboratory of Gastroenterology Department of Gastroenterology Institute of Gastroenterology of Guangdong Province Nanfang Hospital Southern Medical University Guangzhou, China
KEYWORDS
TOPICS
ABSTRACT
Introduction:
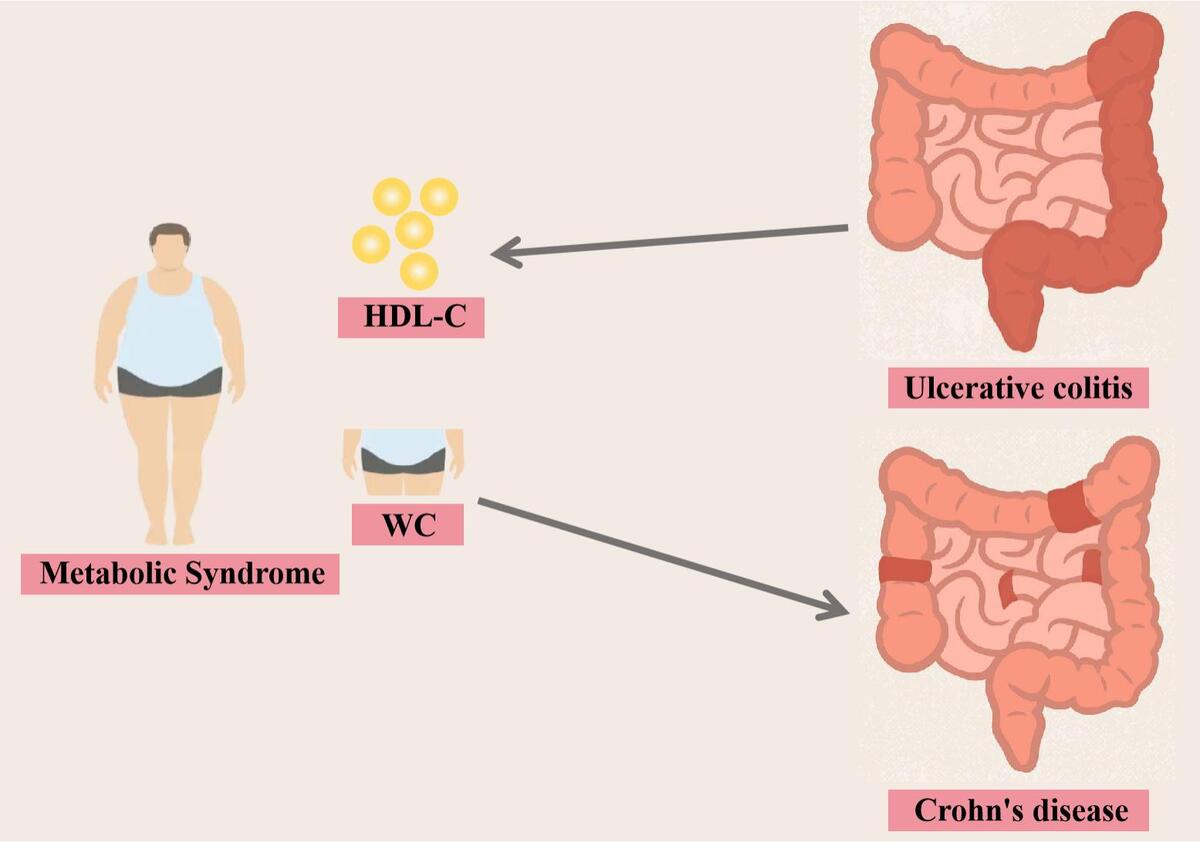
Epidemiological studies have revealed parallel increases in the incidences of metabolic syndrome (MetS) and inflammatory bowel disease (IBD). Clinical observational studies have shown an association between MetS and a poor prognosis of IBD. However, the causal relationship between MetS and IBD remains unclear. This study used bidirectional two-sample Mendelian randomization to investigate potential causal links between MetS and IBD, including ulcerative colitis (UC) and Crohn’s disease (CD).
Material and methods:
Genetic associations of MetS and its components with IBD were sourced from public databases of European populations. Inverse variance weighting was conducted, with weighted median, Mendelian randomization–Egger (MR-Egger), and Mendelian randomization Pleiotropy RESidual Sum and Outlier (MR-PRESSO) methods used as sensitivity analyses. This process was repeated in the opposite direction.
Results:
The inverse variance weighted (IVW) method showed that genetic prediction of MetS may be a potential risk factor for CD (OR = 1.34, 95% CI: 1.009–1.779; p = 0.043). In further estimating the different components of MetS, it was found that waist circumference may increase the risk of CD (OR = 1.33, 95% CI: 1.05–1.684; p = 0.018) and hypertension may increase the risk of UC (OR = 1.61, 95% CI: 1.084–2.39; p = 0.018). Reverse analysis showed that IBD may increase triglyceride levels (OR = 1.019, 95% CI: 1.000–1.038; p = 0.049).
Conclusions:
This MR analysis showed a causal relationship between genetically predicted MetS and CD, and genetically predicted hypertension and UC. Therefore, these patients need to be closely monitored clinically for the risk of CD/UC comorbidities. In patients with IBD, close monitoring of MetS-associated cardiovascular risk is required.
Epidemiological studies have revealed parallel increases in the incidences of metabolic syndrome (MetS) and inflammatory bowel disease (IBD). Clinical observational studies have shown an association between MetS and a poor prognosis of IBD. However, the causal relationship between MetS and IBD remains unclear. This study used bidirectional two-sample Mendelian randomization to investigate potential causal links between MetS and IBD, including ulcerative colitis (UC) and Crohn’s disease (CD).
Material and methods:
Genetic associations of MetS and its components with IBD were sourced from public databases of European populations. Inverse variance weighting was conducted, with weighted median, Mendelian randomization–Egger (MR-Egger), and Mendelian randomization Pleiotropy RESidual Sum and Outlier (MR-PRESSO) methods used as sensitivity analyses. This process was repeated in the opposite direction.
Results:
The inverse variance weighted (IVW) method showed that genetic prediction of MetS may be a potential risk factor for CD (OR = 1.34, 95% CI: 1.009–1.779; p = 0.043). In further estimating the different components of MetS, it was found that waist circumference may increase the risk of CD (OR = 1.33, 95% CI: 1.05–1.684; p = 0.018) and hypertension may increase the risk of UC (OR = 1.61, 95% CI: 1.084–2.39; p = 0.018). Reverse analysis showed that IBD may increase triglyceride levels (OR = 1.019, 95% CI: 1.000–1.038; p = 0.049).
Conclusions:
This MR analysis showed a causal relationship between genetically predicted MetS and CD, and genetically predicted hypertension and UC. Therefore, these patients need to be closely monitored clinically for the risk of CD/UC comorbidities. In patients with IBD, close monitoring of MetS-associated cardiovascular risk is required.
REFERENCES (56)
1.
Buie MJ, Quan J, Windsor JW, et al. Global hospitalization trends for crohn’s disease and ulcerative colitis in the 21st century: a systematic review with temporal analyses. Clin Gastroenterol Hepatol 2023; 21: 2211-21.
2.
Noubiap JJ, Nansseu JR, Lontchi-Yimagou E, et al. Geographic distribution of metabolic syndrome and its components in the general adult population: a meta-analysis of global data from 28 million individuals. Diabetes Res Clin Pract 2022; 188: 109924.
3.
Dobrowolski P, Prejbisz A, Kuryłowicz A, et al. Metabolic syndrome – a new definition and management guidelines: a joint position paper by the Polish Society of Hypertension, Polish Society for the Treatment of Obesity, Polish Lipid Association, Polish Association for Study of Liver, Polish Society of Family Medicine, Polish Society of Lifestyle Medicine, Division of Prevention and Epidemiology Polish Cardiac Society, “Club 30” Polish Cardiac Society, and Division of Metabolic and Bariatric Surgery Society of Polish Surgeons. Arch Med Sci 2022; 18: 1133-56.
4.
Huang PL. A comprehensive definition for metabolic syndrome. Dis Model Mech 2009; 2: 231-7.
5.
Tune JD, Goodwill AG, Sassoon DJ, Mather KJ. Cardiovascular consequences of metabolic syndrome. Transl Res 2017; 183: 57-70.
6.
Cheng K, Faye AS. Venous thromboembolism in inflammatory bowel disease. World J Gastroenterol 2020; 26: 1231-41.
7.
Principi M, Iannone A, Losurdo G, et al. Nonalcoholic fatty liver disease in inflammatory bowel disease: prevalence and risk factors. Inflamm Bowel Dis 2018; 24: 1589-96.
8.
Yki-Järvinen H. Non-alcoholic fatty liver disease as a cause and a consequence of metabolic syndrome. Lancet Diabetes Endocrinol 2014; 2: 901-10.
9.
Chan SSM, Chen Y, Casey K, et al. Obesity is associated with increased risk of crohn’s disease, but not ulcerative colitis: a pooled analysis of five prospective cohort studies. Clin Gastroenterol Hepatol 2022; 20: 1048-58.
10.
Bacha RA, Bouhnik Y, Serrero M, et al. Obesity in adult patients with inflammatory bowel disease: clinical features and impact on disability. A cross-sectional survey from the GETAID. Dig Liver Dis 2023; 55: 1632-9.
11.
Michalak A, Mosińska P, Fichna J. Common links between metabolic syndrome and inflammatory bowel disease: current overview and future perspectives. Pharmacol Rep 2016; 68: 837-46.
12.
Khakoo NS, Ioannou S, Khakoo NS, Vedantam S, Pearlman M. Impact of obesity on inflammatory bowel disease. Curr Gastroenterol Rep 2022; 24: 26-36.
13.
Argollo M, Gilardi D, Peyrin-Biroulet C, Chabot JF, Peyrin-Biroulet L, Danese S. Comorbidities in inflammatory bowel disease: a call for action. Lancet Gastroenterol Hepatol 2019; 4: 643-54.
14.
Adolph TE, Meyer M, Jukic A, Tilg H. Heavy arch: from inflammatory bowel diseases to metabolic disorders. Gut 2024; 73: 1376-87.
15.
Doyle SL, Donohoe CL, Lysaght J, Reynolds JV. Visceral obesity, metabolic syndrome, insulin resistance and cancer. Proc Nutr Soc 2012; 71: 181-9.
16.
Burgess S, Davey Smith G, Davies NM, et al. Guidelines for performing Mendelian randomization investigations: update for summer 2023. Wellcome Open Res 2023; 4: 186.
17.
Skrivankova VW, Richmond RC, Woolf BAR, et al. Strengthening the reporting of observational studies in epidemiology using mendelian randomisation (STROBE-MR): explanation and elaboration. BMJ 2021; 375: n2233.
18.
van Walree ES, Jansen IE, Bell NY, et al. Disentangling genetic risks for metabolic syndrome. Diabetes 2022; 71: 2447-57.
19.
Kurki MI, Karjalainen J, Palta P, et al. FinnGen provides genetic insights from a well-phenotyped isolated population. Nature 2023; 613: 508-18.
20.
Hemani G, Tilling K, Davey Smith G. Orienting the causal relationship between imprecisely measured traits using GWAS summary data. PLoS Genet 2017; 13: e1007081.
21.
Davies NM, Holmes MV, Davey Smith G. Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians. BMJ 2018; 362: k601.
22.
Bowden J, Davey Smith G, Haycock PC, Burgess S. Consistent estimation in mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol 2016; 40: 304-14.
23.
Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol 2015; 44: 512-25.
24.
Verbanck M, Chen CY, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet 2018; 50: 693-8.
25.
Shen Z, Zhang M, Liu Y, et al. Prevalence of metabolic syndrome in patients with inflammatory bowel disease: a systematic review and meta-analysis. BMJ Open 2024; 14: e074659.
26.
Méndez-Sánchez N, Bugianesi E, Gish RG, et al. Global multi-stakeholder endorsement of the MAFLD definition. Lancet Gastroenterol Hepatol 2022; 7: 388-90.
27.
Jiang K, Chen B, Lou D, et al. Systematic review and meta-analysis: association between obesity/overweight and surgical complications in IBD. Int J Colorectal Dis 2022; 37: 1485-96.
28.
Sehgal P, Su S, Zech J, et al. Visceral adiposity independently predicts time to flare in inflammatory bowel disease but body mass index does not. Inflamm Bowel Dis 2024; 30: 594-601.
29.
Yarur AJ, Bruss A, Moosreiner A, et al. Higher intra-abdominal visceral adipose tissue mass is associated with lower rates of clinical and endoscopic remission in patients with inflammatory bowel diseases initiating biologic therapy: results of the constellation study. Gastroenterology 2023; 165: 963-75.e5.
30.
Wunderlich CM, Ackermann PJ, Ostermann AL, et al. Obesity exacerbates colitis-associated cancer via IL-6-regulated macrophage polarisation and CCL-20/CCR-6-mediated lymphocyte recruitment. Nat Commun 2018; 9: 1646.
31.
Nagahori M, Hyun SB, Totsuka T, et al. Prevalence of metabolic syndrome is comparable between inflammatory bowel disease patients and the general population. J Gastroenterol 2010; 45: 1008-13.
32.
Jovanovic M, Simovic Markovic B, Gajovic N, et al. Metabolic syndrome attenuates ulcerative colitis: correlation with interleukin-10 and galectin-3 expression. World J Gastroenterol 2019; 25: 6465-82.
33.
Milajerdi A, Abbasi F, Esmaillzadeh A. A systematic review and meta-analysis of prospective studies on obesity and risk of inflammatory bowel disease. Nutr Rev 2022; 80: 479-87.
34.
Je Y, Han K, Chun J, et al. Association of waist circumference with the risk of inflammatory bowel disease: a nationwide cohort study of 10 million individuals in Korea. J Crohns Colitis 2023; 17: 681-92.
35.
Harpsøe MC, Basit S, Andersson M, et al. Body mass index and risk of autoimmune diseases: a study within the Danish National Birth Cohort. Int J Epidemiol 2014; 43: 843-55.
36.
Rahmani J, Kord-Varkaneh H, Hekmatdoost A, et al. Body mass index and risk of inflammatory bowel disease: a systematic review and dose-response meta-analysis of cohort studies of over a million participants. Obes Rev 2019; 20: 1312-20.
37.
Chan SS, Luben R, Olsen A, et al. Body mass index and the risk for Crohn’s disease and ulcerative colitis: data from a European Prospective Cohort Study (The IBD in EPIC Study). Am J Gastroenterol 2013; 108: 575-82.
38.
Jensen CB, Ängquist LH, Mendall MA, Sørensen TIA, Baker JL, Jess T. Childhood body mass index and risk of inflammatory bowel disease in adulthood: a population-based cohort study. Am J Gastroenterol 2018; 113: 694-701.
39.
Khalili H, Ananthakrishnan AN, Konijeti GG, et al. Measures of obesity and risk of Crohn’s disease and ulcerative colitis. Inflamm Bowel Dis 2015; 21: 361-8.
40.
He Z, Fu T, Lu S, et al. Adiposity as a risk factor for inflammatory bowel disease and the mediating effect of metabolic and inflammatory status: a population-based cohort study. United European Gastroenterol J 2023; 11: 973-84.
41.
Zafar U, Khaliq S, Ahmad HU, Manzoor S, Lone KP. Metabolic syndrome: an update on diagnostic criteria, pathogenesis, and genetic links. Hormones 2018; 17: 299-313.
42.
Choe SS, Huh JY, Hwang IJ, Kim JI, Kim JB. Adipose tissue remodeling: its role in energy metabolism and metabolic disorders. Front Endocrinol 2016; 7: 30.
44.
Kahn CR, Wang G, Lee KY. Altered adipose tissue and adipocyte function in the pathogenesis of metabolic syndrome. J Clin Invest 2019; 129: 3990-4000.
45.
Chung S, Cuffe H, Marshall SM, et al. Dietary cholesterol promotes adipocyte hypertrophy and adipose tissue inflammation in visceral, but not in subcutaneous, fat in monkeys. Arterioscler Thromb Vasc Biol 2014; 34: 1880-7.
46.
Tchernof A, Després JP. Pathophysiology of human visceral obesity: an update. Physiol Rev 2013; 93: 359-404.
47.
Hamdy O, Porramatikul S, Al-Ozairi E. Metabolic obesity: the paradox between visceral and subcutaneous fat. Curr Diabetes Rev 2006; 2: 367-73.
48.
Gonçalves P, Magro F, Martel F. Metabolic inflammation in inflammatory bowel disease: crosstalk between adipose tissue and bowel. Inflamm Bowel Dis 2015; 21: 453-67.
49.
Xiong Z, Wu P, Zhang Y, et al. Radiological biomarkers reflecting visceral fat distribution help distinguish inflammatory bowel disease subtypes: a multicenter cross-sectional study. Insights Imaging 2024; 15: 70.
50.
Zulian A, Cancello R, Ruocco C, et al. Differences in visceral fat and fat bacterial colonization between ulcerative colitis and Crohn’s disease. An in vivo and in vitro study. PLoS One 2013; 8: e78495.
51.
Sinha T, Zain Z, Bokhari SFH, et al. Navigating the gut-cardiac axis: understanding cardiovascular complications in inflammatory bowel disease. Cureus 2024; 16: e55268.
52.
He J, Zhang S, Qiu Y, et al. Ulcerative colitis increases risk of hypertension in a UK biobank cohort study. United European Gastroenterol J 2023; 11: 19-30.
53.
Jaiswal V, Batra N, Dagar M, et al. Inflammatory bowel disease and associated cardiovascular disease outcomes: a systematic review. Medicine 2023; 102: e32775.
54.
Koutroumpakis E, Ramos-Rivers C, Regueiro M, et al. Association between long-term lipid profiles and disease severity in a large cohort of patients with inflammatory bowel disease. Dig Dis Sci 2016; 61: 865-71.
55.
Chen H, Li W, Hu J, et al. Association of serum lipids with inflammatory bowel disease: a systematic review and meta-analysis. Front Med 2023; 10: 1198988.
56.
Toth PP. Triglycerides and cardiovascular risk: getting to the heart of the matter. J Am Coll Cardiol 2024; 84: 1007-9.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.