Introduction
Nonalcoholic fatty liver disease (NAFLD) is a condition characterized by fatty liver without significant alcohol consumption [1, 2]. Although the prevalence of this condition may differ among societies, it is increasingly becoming a global issue, impacting approximately one out of every 3–4 individuals worldwide and showing a steady rise [3–5]. Its prevalence is approximately 70% in the diabetic population and 38% in the general population [6, 7]. Additionally, the current population-based prevalence of NAFLD is approximately 30–40% in males and 15–20% in females [8]. NAFLD can often be asymptomatic, but it can also be a progressive disease process that can lead to serious liver diseases such as steatohepatitis, fibrosis, cirrhosis, and hepatocellular carcinoma [9, 10]. The development of NAFLD involves various mechanisms, including insulin resistance, oxidative stress, disruption of lipid metabolism, and inflammation [11]. In recent years, increasing evidence has shown that fatty liver disease is a multisystem disease that not only increases liver-related morbidity and mortality but also has adverse effects on extrahepatic organs [4]. Metabolic syndrome (MS) is closely related to obesity, dyslipidemia, hypertension (HT), and type 2 diabetes mellitus (DM) [4, 12]. Also the risk of atherosclerotic cardiovascular disease, which is the main cause of death, is increased in these patients [13].
NAFLD can have profound effects on metabolic health. For this reason, a new term, “metabolic dysfunction-associated steatotic liver disease (MAFLD)”, rather than NAFLD, was first proposed by a multisociety consensus in 2020 to refer to fatty liver disease that occurs due to metabolic disorders [14]. For the diagnosis of MAFLD, the presence of at least one of five cardiometabolic risk factors is required in patients with liver steatosis who do not exceed the daily alcohol intake limit (> 20–30 g/day for females and males, respectively).
The diagnostic criteria for MAFLD in adults [14, 15] are as follows:
Boddy mass index (BMI) ≥ 25 kg/m2 or waist circumference (WC) > 94 cm (male), 80 cm (female), or ethnicity-adjusted equivalent;
Fasting plasma glucose (FPG) ≥ 100 mg/dl, glycosylated hemoglobin (HbA1c) ≥ 5.7% or type 2 DM;
Blood pressure ≥ 130/85 mm Hg or specific antihypertensive drug treatment;
Plasma triglyceride (TG) ≥ 150 mg/dl or lipid-lowering treatment;
Plasma high-density lipoprotein (HDL)-cholesterol ≤ 40 mg/dl (male), ≤ 50 mg/dl or lipid-lowering treatment.
MAFLD is a more comprehensive variant of NAFLD and is linked to metabolic dysfunction. This revised definition may enhance the ability to evaluate and handle patients by offering a more comprehensive outlook on clinical practice. When diagnosing and treating MAFLD, it is crucial to consider metabolic risk factors. This technique enables a more precise evaluation and control of patients’ cardiometabolic risks.
The triglyceride-glucose index (TyG index) has become increasingly accepted as an indicator of insulin resistance in the healthy nondiabetic population. The TyG index is calculated from triglyceride and fasting glucose levels. It offers a more convenient and cost-effective alternative to other methods used in insulin resistance assessments. A high TyG index plays a predictive role for diseases such as diabetes mellitus [16], coronary artery disease [17, 18], and atherosclerosis [19]. It is a strong determinant of cardiovascular mortality in diabetic and prediabetic patients [20]. Since dyslipidemia is a significant risk factor for both hepatosteatosis and cardiovascular diseases, we need cost-effective alternatives in clinical practice to effectively predict diseases such as hepatosteatosis that pose metabolic risks, especially cardiovascular events. The plasma atherogenic index (PAI), a new quantitative index used to evaluate lipid levels, is a strong marker of dyslipidemia [21]. The cardiometabolic index (CMI) is a recently developed index based on TG/HDL-C and waist-height ratio (WHtR) values that can be easily obtained during health checks. Multiple key metabolic indicators that comprise the CMI also contribute to the development of fatty liver disease [22]. For this reason, the relationships between the TyG index and MAFLD, along with the PAI and CMI, which are other indicators of cardiovascular mortality, have emerged as essential research topics. Therefore, investigating whether the TyG index is associated with the severity of hepatosteatosis is critical for developing new approaches for the management of these patients. Although previous studies have investigated the effects of insulin resistance and related biomarkers on diabetic fatty liver, studies explicitly investigating the TyG index are limited in nondiabetic patients.
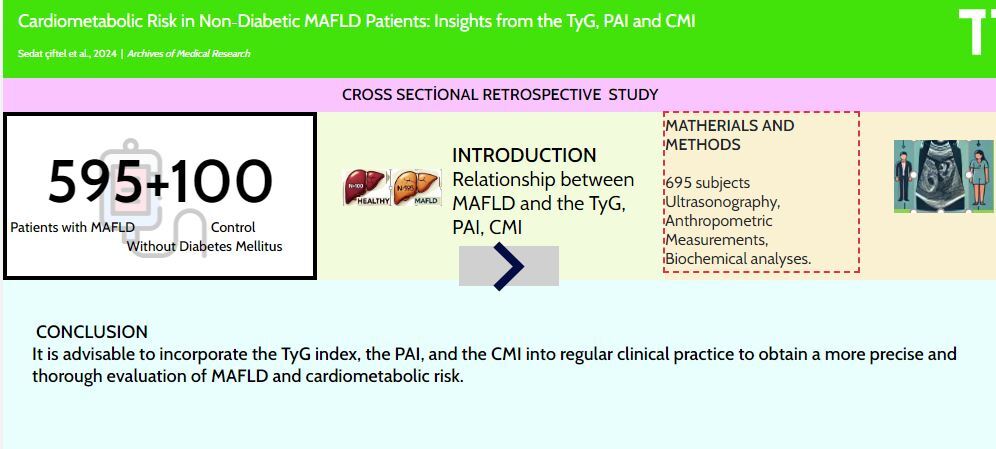
The objective of this study was to analyze the TyG index, PAI, and CMI in nondiabetic patients with MAFLD and to estimate the significance of these indices in diagnosing MAFLD and evaluating cardiometabolic risk. The objective in this context is to incorporate these indices into regular clinical practice to enable early detection of MAFLD and enhance the management of cardiometabolic risks.
Materials and methods
Participants and study design
Six hundred ninety-five nondiabetic individuals aged ≥ 18 years participated in this single-center retrospective study. Our study population consisted of 595 patients with MAFLD (359 females, 236 males). Of these, 271 patients had grade 1 hepatosteatosis (HS), 214 had grade 2 HS, and 110 had grade 3 HS. The control group included 100 subjects of the same age (38.47 ±12) without HS. All the volunteers had undergone transabdominal ultrasonography (US) scanning, in which the liver’s echogenicity was increased compared to that of the renal cortex [23]. US was performed by a single experienced radiologist. The degree of hepatosteatosis was classified into three grades based on echogenicity and the visibility of intrahepatic structures. The patients were categorized into three groups according to their HS grade. The diagnosis of MAFLD was established using the 2020 International Consensus criteria [14]. The study excluded individuals with a known history of DM, cardiovascular disease, other chronic liver diseases, those who consumed more than 20–30 g of alcohol per day, pregnant and breastfeeding women, and patients under 18 years of age and over 65 years of age. DM was defined as an FPG > 125 mg/dl, an HbA1c > 6.5%, a previous diagnosis of diabetes, or the use of any antidiabetic medication. No separate oral glucose tolerance test (OGTT) was conducted to diagnose DM.
Peripheral venous blood samples were taken after 8 h of overnight fasting to assess the serum levels of glucose, TG, HDL, low-density lipoprotein (LDL) cholesterol, alanine aminotransferase (ALT), aspartate aminotransferase (AST), and γ-glutamyl transferase (GGT). BMI was defined as weight (kg)/height (m2) [24]. WC was measured from the midpoint between the lowest rib and the anterior-superior iliac crests with a nonelastic flexible tape measure by the same trained health personnel.
The following formulas were used for calculating lipid-related indices: The TyG index was calculated using TyG = Ln (TG (mg/dl) × FPG (mg/dl)/2 [20, 25]. The PAI was calculated as follows: PAI = log(TG/HDL-C) [25]. The CMI was calculated as follows: CMI = TG/HDL-C × WHtR (WHtR = waist circumference/height) [26].
Statistical analysis
Statistical analysis was performed using the IBM Statistics (SPSS) software, version 22 (IBM Corp., Armonk, NY). The distribution of the variables was assessed using the Kolmogorov-Smirnov test. The independent t test and one-way ANOVA were used to compare normally distributed data. The Mann-Whitney U and Kruskal-Wallis tests were used to compare groups with nonnormally distributed parameters. The Dunn-Bonferroni post hoc correction was used for pairwise comparisons. The normally distributed data between groups are presented as the mean ± standard deviation. The nonnormally distributed data are presented as medians and quartiles. Comparisons between categorical variables were made using the χ2 test. Correlation analysis and logistic regression analysis were performed to evaluate the relationships between categorical and continuous independent variables and dependent variables. Receiver operating characteristic (ROC) curve analysis was performed to determine whether continuous variables can be used in diagnosis and to determine cutoff values. A binary logistic regression analysis was conducted to investigate the effects of common variables in a mixed model for patients with and without hepatosteatosis. The level of statistical significance was set at p < 0.05.
Results
Table I shows the initial characteristics and laboratory measurements of the subjects. The BMI and WC of the patient group with HS were greater than those of the group without HS. There was no statistically significant difference in the BMIs of individuals with grade 1, 2, or 3 hepatosteatosis. The TyG index, PAI, and CMI of the group without HS were significantly lower than those of the group with HS (p < 0.001). In addition, as the HS grade increased, the values of these three parameters increased significantly. The ALT/AST ratio and triglyceride level were found to be significantly lower in the non-HS group (p < 0.001).
Table I
Baseline characteristics and laboratory parameters of participants
[i] HS – hepatosteatosis, BMI – body mass index, WC – waist circumference, WHtR – waist-height ratio, ALT – alanine aminotransferase, AST – aspartate aminotransferase, GGT – γ-glutamyl transferase, HDL-C – high-density lipoprotein cholesterol, LDL-C – low-density lipoprotein cholesterol, TyG – triglyceride-glucose index, AIP – atherogenic index of plasma, CMI – cardiometabolic index.
Table II presents the results of the ROC analysis conducted to investigate the contributions of the TyG, PAI, and CMI indices in differentiating hepatosteatosis and to establish the threshold values. The analytical results indicated that TyG (AUC ± SE; 95% CI: 0.729 ±0.028; 0.674–0.785), PAI (AUC ± SE; 95% CI: 0.748 ±0.027; 0.694–0.801), and CMI (AUC ± SE; 95% CI: 0.779 ±0.027; 0.726–0.831) have the potential to be utilized for the identification of hepatosteatosis. The TyG index, using a cutoff point of 8.47, effectively ruled out the presence of severe simple steatosis, with a sensitivity of 65.3% and a specificity of 66.0%. The PAI, with a cutoff point of 0.39, effectively ruled out the presence of severe simple steatosis, with a sensitivity of 66.6% and a specificity of 67.0%. CMI, with a threshold of 1.40, effectively ruled out cases of significant steatosis, with a sensitivity of 70.1% and specificity of 70.1%.
Table II
Analysis of ROC curve results of TyG, AIP, and CMI for MAFLD
In Table III, a binary logistic regression analysis was performed to examine the impact of common factors in a mixed model, which included TyG index, the ALT/AST ratio, and WC. The analysis yielded a specificity of 40.4 and a sensitivity of 96.7. The analytical results indicate that in the TyG index model (B ± SE; 1.186 ±0.271, OR = 3.273, p < 0.001), age (B ± SE; –0.007 ±0.012, OR = 0.993, p = 0.575), the ALT/AST ratio (B ± SE; 1.798 ±0.314, OR = 6.037, p < 0.001), and the WHtR (B ± SE; 0.319 ±2.45, OR = 1.375, p = 0.897) are significant factors. The sex distribution was analyzed using logistic regression. The estimated coefficient (B) was –0.967, with a standard error (SE) of 0.328. The odds ratio (OR) was calculated to be 0.380. The body mass index (BMI) was calculated as B ± SE; 0.149 ±0.012, with an odds ratio (OR) of 1.160 and a p-value < 0.001.
Table III
Logistic regression analysis of participants in terms of hepatosteatosis presence in a mixed model
Spearman correlation analyses were performed to compare TyG with other metabolic markers. Table IV shows that there was a moderate association between the TyG index and other parameters that were not included in the calculation.
Discussion
In this study, we investigated the impact of the presence and degree of hepatosteatosis on the TyG index, PAI, and CMI in individuals without diabetes. The findings showed that patients with hepatosteatosis had significantly greater TyG index, PAI, and CMI values than those without hepatosteatosis. Furthermore, in patients with MAFLD, these index levels progressively increased as the degree of hepatosteatosis increased, even though the BMI remained the same. These findings clearly demonstrate the relationship between hepatosteatosis and cardiometabolic risk factors in the absence of diabetes mellitus. The impact of hepatosteatosis on cardiometabolic risk factors can be explained through a series of biological mechanisms. First, hepatosteatosis can lead to insulin resistance, adversely affecting triglyceride and glucose metabolism. This condition results in an elevated TyG index. The literature has previously reported a strong association between the TyG index and cardiometabolic risk factors, such as insulin resistance and metabolic syndrome [19]. A previous cohort study, comparable to our own, revealed that the TyG index could serve as an independent predictor of cardiovascular disease (CVD) in nondiabetic patients [27].
Our study revealed that this relationship is also valid in nondiabetic individuals and that hepatosteatosis can be an essential indicator of cardiometabolic risk. Second, fat accumulation in the liver and the resulting inflammation can lead to changes in the atherogenic lipoprotein profile, contributing to an elevated PAI. Given the effects of hepatosteatosis on metabolic dysfunction and lipid metabolism, the PAI is expected to be elevated in these patients [28]. A recent study was undertaken to assess new indices for predicting MAFLD. This study revealed that the AIP can be used as a predictive marker for MAFLD in nondiabetic patients, which is consistent with our own findings [29]. Our study confirms this expectation, showing that the PAI is significantly greater in patients with MAFLD. Third, the progression of hepatosteatosis, with increased oxidative stress and inflammation [30], can adversely affect overall cardiometabolic health, leading to an elevated CMI, a valuable new index for assessing visceral obesity [22, 25, 26]. A recently published study revealed a link between systemic immune-inflammatory indices (SIIs) and the presence and severity of NAFLD [31]. Another study demonstrated a positive association between the pan-immune-inflammation value (PIV) rather than the systemic immune-inflammation index and NAFLD or hepatic fibrosis [32]. These three metabolic indices are essential markers that should be evaluated together to reflect metabolic health. Abdominal obesity, increased BMI, and the presence of DM are known to be the most important triggers of MAFLD [25]. In our patients with hepatosteatosis, risk factors other than diabetes were present, but there was no difference in BMI among the different grades of hepatosteatosis. The presence of MAFLD patients with a normal BMI and normal WC, TG, HDL, LDL, ALT, and AST levels indicates that these factors alone are insufficient for diagnosing MAFLD. Therefore, measuring the TyG index, PAI, and CMI, which encompass multiple factors, is a more accurate and practical approach.
Our study revealed that grade 3 hepatosteatosis was more prevalent among males. One possible explanation for this finding is that women are more resistant to NAFLD than males are during the premenopausal phase. Estrogen signaling in the female liver enhances metabolic flexibility, preventing hepatic, metabolic, and inflammatory alterations even in situations of imbalanced nutrition [33]. The liver-protective action of estrogens may be attributed to a decrease in sex hormone-binding globulin (SHBG) levels, which limits the progression of NAFLD to hepatocytes in men, women with polycystic ovary syndrome, and postmenopausal women [34]. Following menopause, the occurrence of NAFLD becomes similar across males and females. The menopausal status of the female participants in our study was not known. Nevertheless, our study included persons aged 18–65, with a high likelihood that the majority of female participants were in their reproductive years.
Fatty liver diseases, such as MAFLD, discussed in this study, currently present significant challenges in terms of both diagnosis and treatment [31, 35–37]. This condition, frequently overlooked in clinical practice, has emerged as a growing health concern. The identification of MAFLD enables the implementation of more focused treatment strategies that are tailored to individuals’ metabolic risk profiles. Aside from invasive procedures such as biopsies, the absence of sensitive noninvasive diagnostics hinders the early detection and treatment of the disease, hence complicating the diagnosis and treatment process [6, 10, 38]. The contemporary literature concurs that the existing screening approaches based on liver enzymes have certain shortcomings, which can result in overlooked diagnoses and delays in treatment [39]. Scientific evidence supports our work by demonstrating that the likelihood of developing MAFLD is elevated even when ALT levels fall within the normal range. Hence, there is an urgent need for cost-effective and easily deployable new diagnostic approaches to enhance the precision of MAFLD diagnosis and facilitate early intervention. Currently, there are limited diagnostic tools and treatment alternatives available for this particular condition. Ongoing efforts are being made to discover a straightforward and easily applicable diagnostic procedure as well as an effective pharmacotherapeutic drug. Hence, incorporating this subject into our investigation is crucial for broadening the scope of our research and emphasizing the existing difficulties in the management of MAFLD.
Although this study revealed the relationship between hepatosteatosis and cardiometabolic risk indices in nondiabetic patients, it has several limitations. The ultrasound method used to detect hepatosteatosis is known to be less reliable when the fat content is less than 20% [40]. Despite concerns about underestimating the prevalence of MAFLD, the low cost, patient comfort, ease of use, and accessibility of ultrasound, along with the sampling errors and postprocedural complications associated with the gold standard liver biopsy [41], were the main reasons for preferring ultrasound. The imbalance in the number of patients and controls and the sex distribution is another limiting factor of our study. Due to the limited sample size and the retrospective cross-sectional nature of the study, a causal relationship cannot be established. Future studies can examine these relationships more profoundly using larger sample groups and longitudinal designs. Additionally, similar studies in different patient populations can enhance the generalizability of the findings.
In conclusion, the use of the PAI, CMI, and TyG indices in routine clinical evaluations can aid in the early detection of patients with hepatosteatosis and the more effective management of cardiometabolic risks. Considering that the levels of these indices increase with the degree of hepatosteatosis, periodic evaluation of these indices can be recommended to monitor the progression of hepatosteatosis. Particularly in nondiabetic individuals, using these indices can enhance the sensitivity of cardiometabolic risk assessment and expand the opportunities for early intervention.