Introduction
While vitamin D has conventionally been linked to bone health due to its vital involvement in bone and mineral metabolism, it is now being recognized for various non-skeletal functions [1]. Recently, a more extensive role has been suggested for this essential vitamin, attributed to the presence of its receptor in diverse tissues, including cardiovascular organs. Atherosclerosis, a prominent feature of cardiovascular disorders, is a complex process that can evolve over decades before becoming clinically evident [2]. Inflammatory alterations, osteogenesis, angiogenesis, and endothelial dysfunction are among the crucial factors associated with the pathogenesis of atherosclerosis, all of which are either directly or indirectly influenced by vitamin D [3].
Numerous studies have investigated the correlation between vitamin D status and various aspects of cardiovascular disorders, such as metabolic syndrome, hypertension, or fatal events associated with coronary artery disease (CAD) [4, 5]. In light of these findings, there is a growing call for heightened attention to the potential role of vitamin D deficiency as a risk factor for CAD. Nevertheless, the existing evidence remains inconclusive due to conflicting reports in the literature, with some supporting and others opposing this concept [6, 7]. Importantly, the genetic polymorphism of the vitamin D receptor may alter its role, and variations in ethnicity, lifestyle, and geographic conditions could potentially influence its effects [8].
The objective of this study was to assess the correlation between vitamin D levels and the findings of coronary artery computed tomography (CT) angiography in a Slovakian population.
Material and methods
In this cross-sectional study, we extended invitations to patients referred for coronary artery CT angiography (CTA) by a cardiologist. Exclusions encompassed individuals with recent coronary heart disease, such as prior myocardial infarction, coronary stent or bypass grafting, or recent invasive coronary angiography confirming coronary vessel stenosis. Additionally, those with vitamin D intake, chronic diseases (including known hepatic, renal, endocrine, or metabolic conditions), a documented presence of supraventricular tachyarrhythmia with numerous extrasystoles in the resting electrocardiogram (ECG), and individuals allergic to contrast agents were excluded. Informed consent was obtained from all participants following a thorough explanation and clarification of the study procedures.
The sample comprised 205 patients (20 were excluded). Initially, the age and sex of each patient were recorded, as well as any family history of CAD and cigarette smoking. Patients were introduced to a constant laboratory environment at our hospital on the same day as CTA. Blood samples were taken and analyzed, and serum levels of 25-hydroxyvitamin D (25(OH)D) were measured using high-performance liquid chromatography. Based on the levels of vitamin D measured, patients were categorized into two groups as follows: vitamin D deficiency (< 20 ng/ml) and non-insufficient level of vitamin D (> 20 ng/ml) [9].
All participants underwent a two-phase imaging protocol, beginning with a noncontrast scan followed by contrast-enhanced coronary CT angiography (CTA), utilizing a 64-slice scanner system (SOMATOM Force; Siemens AG, Berlin, Germany). The Agatston scoring method (Aquarius iNtuition software, TeraRecon, Inc., San Mateo, CA, USA) was employed to determine the coronary artery calcium score (CACS), which was recorded for each patient. Patients were then categorized into five groups based on their scores according to Rumberger’s guidelines: normal (CACS = 0), minimal (CACS = 1–10), mild (CACS = 11–100), moderate (CACS = 101–400), and severe (CACS > 400) [10]. A retrospective electrocardiogram-gated technique was employed, and the scan delay was calculated using the test bolus technique. Intravenously, a bolus of 70 ml of iodinated contrast (Visipaque, GE Healthcare) was injected, followed by saline, at a flow rate of 4.5 ml/s. The scan parameters included collimation of 64 × 0.625 mm, tube current of 400–600 mA, tube voltage of 120 kV, and gantry rotation time of 350 ms.
Initially, source images were reconstructed at 75% of the R-R interval to serve as default images; however, alternative phase locations were also available and reviewed as needed. Thin slice maximum intensity projections and curved multiplanar reconstructions were employed. The evaluation included the assessment of coronary artery stenosis, with the severity estimated as the ratio of the luminal diameter in the most stenotic area to that of the unaffected distal portion. A stenosis was deemed significant if it reached 50% or more. An independent review of all scans was conducted by both a cardiologist and a radiologist with expertise in coronary CTA. Subsequently, patients were classified into two groups: normal and nonsignificant disease (absence of plaque or presence of plaque with less than 50% stenosis), and significant disease (plaque with more than 50% stenosis in one, two, or three major coronary arteries).
Statistical analysis
Quantitative variables, such as continuous measurements, and qualitative variables, representing categorical data, were detailed by presenting their mean values along with their respective standard deviations. Additionally, proportions were expressed as percentages to provide a comprehensive understanding of the data distribution. For statistical inference, a robust suite of tests and analyses was employed, including the Kolmogorov-Smirnov test and the Shapiro-Wilk test, to assess the normality of the data distribution. The Spearman correlation coefficient was utilized to explore potential relationships between variables, particularly examining associations between serum vitamin D levels and other pertinent factors. Furthermore, the study conducted multivariable regression analysis, which incorporated a comprehensive set of covariates such as age, gender, smoking status, arterial hypertension, and/or hyperlipidemia. This analytical approach allowed for a thorough investigation into the collective impact of these factors on serum vitamin D levels. To ascertain statistical significance, a two-sided α level of 0.05 was applied. The analysis was performed using the R Statistics software, version 3.5, an open-source project known for its robustness and versatility, which facilitated comprehensive data exploration and interpretation across all participant data sets.
Results
Clinical characteristics of patients
Out of 225 patients initially considered for the study, 205 met the inclusion criteria. The average age of participants was 61.4 ±10.8 years, ranging from 30 to 85 years. The age distribution was as follows: 14.1% (n = 29) were under 50 years old, 28.3% (n = 58) were between 50 and 59 years, 36.1% (n = 74) were between 60 and 69 years, and 21.5% (n = 44) were 70 years or older. Approximately 43% (n = 88) were male, and 16.6% (n = 34) were smokers. In terms of the presence of other selected risk factors (arterial hypertension, type 2 diabetes mellitus, elevated LDL-C), their prevalence was as follows. Out of the total of 205 patients, 168 patients were treated for hypertension (80.5%), and 18 (8.8%) patients had documented type 2 diabetes mellitus either on diet, oral antidiabetic therapy, or insulin therapy. The average level of LDL-C was 3.1 mmol/l, with the highest at 5.6 mmol/l and the lowest at 1.34 mmol/l. The average serum vitamin D level was 19.6 ±10.3 ng/dl, ranging from 4.7 to 39.7 ng/dl. According to the results, 52.1% of all participants (n = 107) had vitamin D deficiency, while 47.2% (n = 98) did not have vitamin D deficiency, and they were divided into these two groups (Table I).
Table I
Summarized characteristics of participants
Coronary artery disease
The CT angiographic findings among participants were as follows: 77% (n = 158) had normal or nonsignificant CTA; 23% (n = 45) had at least one significant coronary artery stenosis.
Calcium score
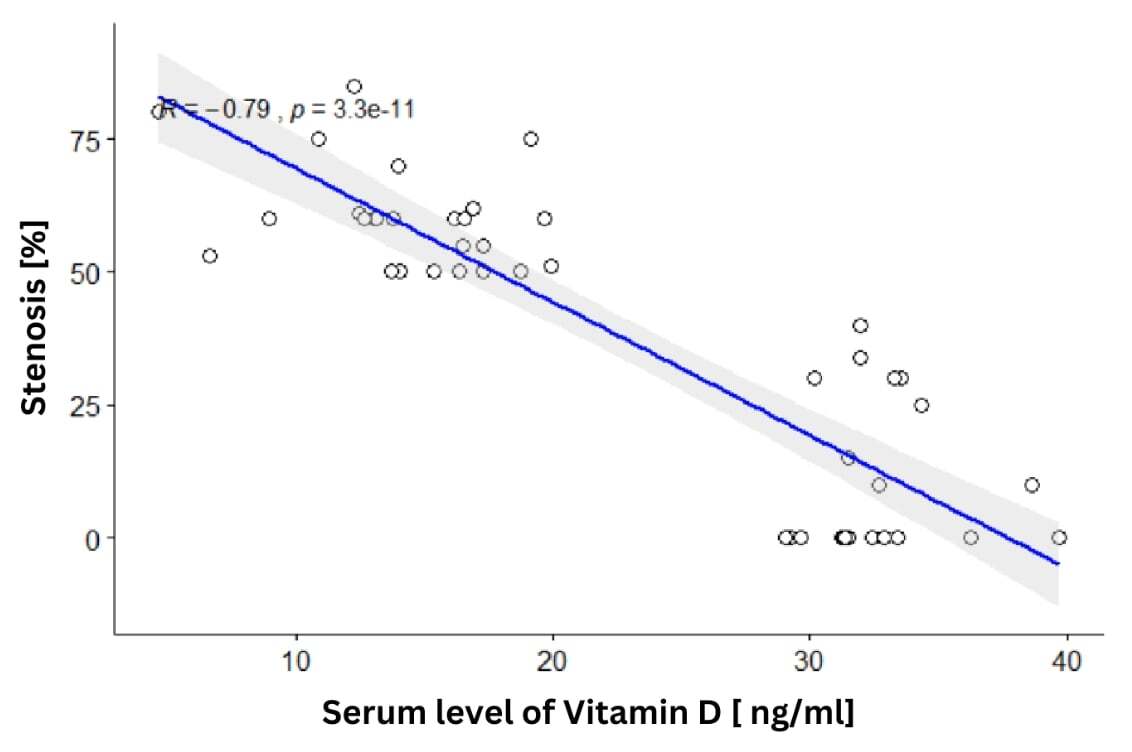
Among the participants, 37.5% (n = 77), 10.2% (n = 21), 17.5% (n = 36), 18.5% (n = 38), and 17.5% (n = 36) had normal, minimal, mild, moderate, and severe calcium scores, respectively. As anticipated, the mean calcium score was notably higher in patients with severe CAD (p < 0.0001). The Spearman test revealed a significant negative correlation coefficient (–0.48) between serum vitamin D levels and (CACS) (p < 0.0001) (Figure 1). Conversely, the mean CACS in the vitamin D deficient group was significantly higher than in the vitamin D insufficient and non-insufficient groups (p < 0.0001).
Vitamin D
There was a significant decline (p < 0.0001) in the mean serum vitamin D level with increasing severity of CAD (Figure 2). In the logistic regression analysis, among the determinants including age, gender, smoking habits, arterial hypertension, hyperlipidemia, and serum vitamin D level, the latter emerged as a significant determinant of CAD (Table II). This implies that individuals with adequate vitamin D levels have a lower cardiovascular risk and are less likely to exhibit hemodynamically significant stenosis. Conversely, those with a vitamin D deficiency fall into a higher cardiovascular risk category, and a greater likelihood of coronary artery disease has been observed in this group. Finally, among the determinants mentioned above, only hyperlipidemia was a significant factor affecting serum vitamin D levels. Patients without hyperlipidemia and with lower CACS exhibited significantly higher levels of vitamin D compared to those with hyperlipidemia and with higher CACS (p < 0.01) (Table III).
Table II
Results of the logistic regression analysis considering age, gender, smoking habits, arterial hypertension, hyperlipidemia, and serum vitamin D level as determinants of CAD
Table III
Results of the multiple regression analysis considering age, gender, smoking habits, arterial hypertension, hyperlipidemia, and coronary artery calcium score as determinants of vitamin D level
Discussion
Vitamin D deficiency poses a significant health challenge on a global scale, especially in developing nations [11]. In the current study, 52.1% of all patients exhibited vitamin D deficiency (below 20 ng/ml). This figure aligns with the global prevalence [12].
The assessment of vitamin D deficiency in various disorders, including CAD, has yielded conflicting results. Nevertheless, the presence of genetic polymorphisms in the vitamin D receptor suggests that differences related to ethnicity may influence the occurrence of vitamin D deficiency [13]. Our study revealed a relationship between serum vitamin D levels and the severity of CAD. These findings diverge from those reported by Ho et al. [14]. However, such discrepancies could be attributed to variations in geographical location, ethnicity, a lower CAD prevalence in their study, and the absence of female participants. Additionally, the relatively small sample size in our study may have contributed to these differences.
While previous global studies have consistently identified a connection between disorders related to coronary arteries and vitamin D deficiency, they have not directly analyzed detailed angiographic data [15–21]. However, our current study revealed a noteworthy correlation between elevated CACS and the severity of vitamin D abnormalities (deficiency or insufficiency). Given the established role of CACS in predicting the plaque burden of coronary arteries, its significant association with low vitamin D levels in this study suggests a meaningful relationship between the severity of CAD and abnormal vitamin D levels.
In the evidence recently published by Fang et al., genetically lowered 25(OH)D levels did not show an elevated risk of CAD [22]. This implies that the potential connection between vitamin D levels and CAD might be influenced by confounding factors or reverse causation. Vitamin D deficiency is linked to several conditions, including obesity, insulin resistance, diabetes, metabolic syndrome, hypertension, and hyperlipidemia [23–25]. Additionally, significant associations are observed between abnormalities associated with vitamin D and major cardiovascular events, such as heart failure, myocardial infarction, sudden cardiac death, stroke, atrial fibrillation, and peripheral vascular disease [26, 27].
The precise understanding of the pathophysiology underlying the connection between vitamin D deficiency and atherosclerosis is essential for grasping the underlying mechanisms and potential treatment implications. Numerous observational studies consistently reveal a reciprocal relationship between vitamin D deficiency and risk factors for atherosclerosis. Insufficient levels of vitamin D are linked to conditions such as hypertension, dyslipidemia, insulin resistance, and obesity, all of which fuel the development and progression of atherosclerosis [28]. Moreover, vitamin D deficiency correlates with indicators of hidden atherosclerosis, such as increased carotid intima-media thickness and coronary artery calcification, underscoring its significant role in atherosclerosis progression. While the precise mechanisms linking vitamin D deficiency to atherosclerosis are still under investigation, one proposed mechanism depends on the anti-inflammatory properties of vitamin D. It inhibits the production of pro-inflammatory cytokines and curtails the activation of immune cells involved in atherosclerotic processes. By modulating the inflammatory response, vitamin D may alleviate the inflammatory burden within arterial walls, consequently impeding atherosclerosis development and progression. Additionally, vitamin D might impact endothelial function, oxidative stress, and vascular smooth muscle cell proliferation – critical processes in atherosclerosis. By enhancing nitric oxide (NO) production, reducing oxidative stress, and dampening inflammation, vitamin D could ameliorate endothelial function. Furthermore, it may regulate the proliferation and migration of vascular smooth muscle cells, thereby contributing to plaque stability [29, 30].
In conclusion, our findings, along with those of the majority of existing literature, suggest a correlation between vitamin D levels and the severity of CAD to some extent. Clearly, conducting additional well-designed studies with a larger cohort of Slovak patients is imperative to validate the role of vitamin D in both primary and secondary prevention of CAD.
Limitations: While we established a significant association between vitamin D deficiency and CAD, certain limitations should be acknowledged. CAD is a chronic process typically initiated in childhood, yet we relied on a single laboratory report of vitamin D levels, which may not be indicative of past or lifelong vitamin D status. The fluctuation of vitamin D levels with seasons, though not assessed in our study, was mitigated by our sampling strategy, which covered all four seasons fairly evenly. Memory bias, inherent in relying on patient recollection regarding supplement avoidance during sampling, could not be entirely eliminated.
The experiment was conducted with a particular set of participants. Our study cohort consisted solely of patients residing in urban areas within the central region of Slovakia. The majority of these patients were undergoing treatment with statins. The study did not consider the dosage or duration of statin treatment, which is recognized to influence vitamin D levels [30]. Therefore, the findings cannot be generalized to other populations. Additionally, the study was observational and cross-sectional in nature, meaning it cannot establish causation but can only highlight statistical correlations. Finally, lack of a control group is one of the biggest limitations of the study which needs to be mentioned.
The known link between hypertension and vitamin D deficiency, coupled with the relationship between hypertension and CAD, introduces the possibility of confounding variables. Additionally, while CTA is a non-invasive imaging method with high sensitivity and specificity for identifying coronary plaques, the functional significance of these plaques remains elusive without diagnostic invasive selective coronary angiography. Nonetheless, ongoing advancements in CT devices with each new model are noteworthy. To clarify this hypothesis, further studies with larger samples, free from these limitations, are imperative.
In conclusions, a correlation was observed between vitamin D levels and both CACS and the severity of luminal stenosis caused by atherosclerotic plaques. Despite scientific societies’ recommendations not endorsing vitamin D supplementation for preventing or slowing the progression of CAD, given the relatively high prevalence of cardiovascular disease in the study population, further research in this area is warranted. Such investigations could help evaluate the potential beneficial effects of such treatment in patients with these conditions.