Introduction
Total hip arthroplasty (THA) is one of the most frequently performed surgical procedures in orthopedics [1, 2]. Recently, with a continual lengthening of the mean lifespan an increase has been noted in the number of patients with degenerative disease. This increase has been accompanied by greater numbers of endoprosthesis procedures. Over 200 000 THA procedures were performed in the USA in 2005, and this number is predicted to rise to over 570 000 by 2030 [3]. The projected increase in annual THA performed in the US for 2040 is 284% compared to 2014 data [3]. Similarly, costs associated with THA in the USA, currently estimated at over $13.7 billion in 2009, are expected to rise by 175% by the year 2030 [4, 5].
Although a range of THA techniques can be performed, the most commonly employed approaches are the posterolateral approach (PLA) and lateral approach [6, 7]. However, the last twenty years have seen a growth in interest in the use of minimally invasive techniques. One form of minimally invasive procedure employs the direct anterior approach (DAA, MIS DAA).
It has been proposed that MIS DAA may be associated with minimal tissue damage, a shorter surgery procedure, less exposure of the wound, reduced use of analgesic substances, post-operative pain killers and better function of the operated joint compared to PLA [7–13]. In addition, MIS DAA demonstrates a very low frequency of complications [14–17]. Previous works suggest that DAA offers shorter hospitalization time, i.e. length of stay (LOS), than PLA [15, 16, 18–20].
LOS is thought to have the greatest influence on inter alia the number of postoperative complications, the risk of hospital infection, the overall cost of therapy and the ultimate postoperative outcome [15, 17, 21–30].
The choice of surgical approach, which potentially allows faster and more effective patient mobilization and rehabilitation, and thus a shorter hospitalization time, can bring a number of benefits for both the patient and the treatment center.
The aim of the study was to compare two approaches, DAA and PLA, in terms of LOS, economic outcomes, quality of life, hip joint function and hip joint awareness.
Material and methods
The study was performed as a retrospective analysis of 52 cementless total hip arthroplasty procedures performed by MIS DAA and 56 cementless THA performed by classic standard PLA (the characteristics of the groups are presented in Tables I and II) in the period 2017–2018 in orthopedic centers in two cities in Poland.
Table I
Descriptive statistics of continuous biodemographic variables – summary
Table II
Percentage distributions of qualitative demographic variables
The exclusion criteria comprised:
post-traumatic arthrosis,
post-infectious arthrosis,
hip joints which had been operated on previously,
hip joint dysplasia – Crowe type > II,
ASA (American Society of Anesthesiologists Scale) score below 2.
All patients qualified for the study, i.e. both the DAA and PLA groups, were operated on under spinal anesthesia.
Patients qualified for surgery were admitted to the hospital 24 h before the planned procedure. The LOS was calculated from the time of admission to the time of discharge. All the procedures took place within the planned time, i.e. within 24 h following admission to the hospital. All patients qualified for THA received a diagnostic survey using the HHS (Harris Hip Score), FJS-12 (Forgotten Joint Score 12) and WHOQOL (World Health Organization Quality of Life scale). This procedure was repeated after 3 months, and again after 6 months. In addition, the level of pain in the operated joint was assessed each day during hospitalization on the VAS (Visual Analog Scale).
The PLA and DAA procedures were performed in the period 2017–2018 by a two single surgeons who perform a minimum of 80 PLA and 80 DAA hip replacement operations each year. They had at least 8 years’ experience of performing THA surgery.
The PLA procedure was performed according to the standard method. MIS DAA was performed through the intramuscular space between the tensor fasciae late muscle and the sartorius muscle [11, 19, 31, 32]. No incisions were performed with the aim of dissecting the muscles. During the preparation of the proximal part of the femur, the operating table was hyperextended at 15° to the hip. The standard ‘4’ position was replaced by a 20-degree bend in the knee joint and an external rotation of 90°. This method allowed the tissue trauma to be minimized without worsening the operating conditions and femur exposure during implantation of the hip stem. After completion of only the fascia, subcutaneous tissue and skin were sutured. This method allowed the tissue trauma to be minimized without worsening the operating conditions and femur exposure during implantation of the hip stem.
At the beginning of the procedure, each patient received 1 g of intravenous tranexamic acid [31]. No automatic retractors, traction tables or fluoroscopy were used during the procedures. No drain was used in the PLA and MIS DAA groups. Compression dressings and drainage were not used. Implants available in the clinics which took part in the study were used for the procedure.
Both groups had postoperative X-rays of the hip joints within 24 h of the end of the procedure, received prophylactic antibiotic therapy (cefazolin), low molecular weight heparins as antithrombotic prophylaxis during hospitalization and analgesic treatment in accordance with the analgesic ladder. Other internal medicine was administered according to the individual needs of the patient.
On the first day after the procedure, all patients were mobilized with the assistance of a physiotherapist and began learning to walk using crutches or a walking frame. Postoperative rehabilitation followed the same pattern in both examined groups. The patients were discharged from the department on the day they met the discharge criteria:
independent movement using one or two crutches or a walking frame,
independent movement on the stairs,
sufficient functional range of motion in the operated joint (0–90°),
understanding further discharge recommendations,
hemoglobin level above 9 mg/dl,
VAS score below 3.
Postoperative follow-up visits were carried out by operators after 3 and 6 months after the operation. Data regarding the cost of MIS DAA were obtained from the hospital which performed the procedure.
Statistical analysis
All statistical analyses were performed using Statistica 9.0 software. The Kolmogorov λ-test was used to determine whether the results were normally distributed. As the distribution was normal, Student’s t-test for independent events was then used to compare the length of stay for each patient following the operation.
Descriptive statistics were calculated for the following indicators: hip function according to the HHS questionnaire, the level of joint awareness measured by the FJS-12 questionnaire and the quality of life measured by the WHOQOL-Brief questionnaire.
Each parameter was measured three times for each patient, i.e. before the operation (P1), 3 months after the operation (P2) and 6 months after the operation (P3), giving three measurements per value (Stanisz, 2007). As the measurements were all quantitative, the entire spectrum of descriptive statistics was applied: range (min–max.), measures of central tendency (mean) and distribution (standard deviation), and measures of location (skewness, kurtosis).
Results
To determine the homogeneity of the groups identified in the study, they were compared in terms of demographic variables. All were found to be homogeneous according to age, body mass index (BMI), sex distribution, and ASA qualification by an anesthesiologist.
Neither group demonstrated any significant postoperative complications that would affect the time of hospitalization, such as DVT/PE, dislocation or loosening of the endoprosthesis components, or early signs of infection. All patients demonstrated a hemoglobin level above 9 mg/dl; none of the patients required blood transfusion.
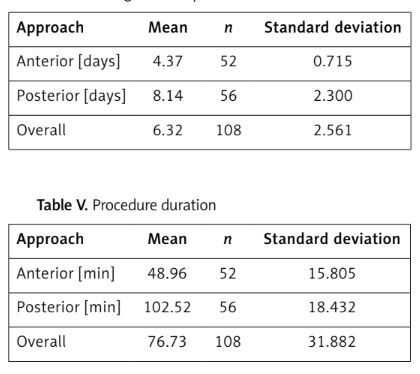
The length of stay in the hospital, and the duration of the procedure according to operative approach, are included in Table III.
Table III
The mean length of hospitalization values were compared between approach types (DAA and PLA)
| Parameter | n | Minimum | Maximum | Mean | Standard deviation |
|---|---|---|---|---|---|
| Procedure duration [days] | 108 | 30 | 165 | 76.73 | 31.882 |
| Length of hospitalization [days] | 108 | 3 | 19 | 6.32 | 2.561 |
Table IV
Length of hospitalizations
| Approach | Mean | n | Standard deviation |
|---|---|---|---|
| Anterior [days] | 4.37 | 52 | 0.715 |
| Posterior [days] | 8.14 | 56 | 2.300 |
| Overall | 6.32 | 108 | 2.561 |
Table V
Procedure duration
| Approach | Mean | n | Standard deviation |
|---|---|---|---|
| Anterior [min] | 48.96 | 52 | 15.805 |
| Posterior [min] | 102.52 | 56 | 18.432 |
| Overall | 76.73 | 108 | 31.882 |
Table VI
Consecutive measurements of the functional capability of the hips of patients undergoing posterior approach surgery and interaction of these two factors: descriptive statistics, effect size and post-hoc tests
Table VII
Quality of life of patients undergoing surgery by the anterior and posterior approaches and the interaction between two factors: descriptive statistics, effect size and post-hoc tests
The two approach types did not display homogeneity of variance with regard to the mean duration of the procedure (Levene’s test: F = 17.89; p < 0.005). The choice of approach significantly influenced the mean LOS (Student’s t-test: t (66) = –11.70; p < 0.005): it was found to be significantly shorter for the anterior approach (DAA) (4.37 days) than the posterior approach (8.14 days) (Student’s t-test for independent variables: p < 0.005).
The mean duration of the anterior approach procedure (48.96 min) was found to be around half that of the posterior approach (102.52 min). Variations in mean duration within the groups were found to be homogeneous (Levene’s test: F = 2.37; p > 0.005). The mean durations of the two types of approaches were found to be significantly different (Student’s t test: t (106) = –16.15; p < 0.005).
A VAS score level below 3 was acquired in the DAA group at 1.47 days post-operatively and 1.94 days in the PLA group. The difference showed statistical significance.
The financial costs of the stay in the ward were analyzed. It was assumed that the fixed costs (food, nursing, energy, cost of hospital administration) only constituted a small share of the total cost of stay. In addition, as both types of approaches had similar fixed costs, it is reasonable to omit these charges in further calculations. The cost of the procedure was found to be the same in both hospitals: the mean cost of the stay was PLN 377, and the costs resulting from the operation were PLN 4531/h of work in the operation room. Hence, it can be concluded that the shorter mean duration of stay and shorter procedure duration associated with the anterior approach result in mean savings of PLN 5465.96 per procedure.
Hip joint fitness assessment
Identical hip function measured as the Harris Hip Score was found in the individual anterior and posterior groups, and in both groups combined. In each case, all three consecutive measurements, i.e. postoperative, after 3 months and after 6 months, significantly differed from each other (each < 0.001): Improved hip function was observed immediately after the operation, and this improvement was even greater after 6 months.
The measurements taken immediately after the operation demonstrated a significant difference with regard to interaction effect (p = 0.019). Both groups reported equally low performance before the operation and higher performance 6 months later; however, 3 months after the operation, the anterior group reported significantly worse performance (approximately 7%) than the posterolateral group.
Evaluation of quality of life
The patients reported higher quality of life measured according to the WHOQOL-BREF following the operation. Statistical analysis confirmed that the quality of life had significantly improved immediately after the operation, and continued to improve over the following 6 months (all p < 0.001). No significant difference was observed between the two approaches.
Evaluation of hip joint awareness
Significant differences were observed between successive measurements of the hip joint measured on the FJS12 scale – hip joint feeling was approximately 25% higher before the operation than afterwards; this value had fallen by 17% after the following 6 months (p < 0.001). In addition, patients treated by the posterior approach were significantly more likely to experience higher hip joint awareness than those treated by the anterior approach (p < 0.001).
All data discussed above are presented in Tables III–VIII.
Table VIII
Joint awareness at successive observations of patients undergoing surgery by the anterior and posterior approaches, and the interaction between two factors: descriptive statistics, effect size and post-hoc tests
Discussion
The growing demand for THA should motivate clinicians to improve the course of treatment and rehabilitation while maintaining an appropriate level of safety for the patient [3–5]. The LOS of a patient following THA has a significant influence on the final outcome of treatment [25], and there is a great interest in reducing the LOS for both medical and economic reasons [24].
Our findings demonstrate that the DAA enables a significant shortening of the LOS while also maintaining patient safety and ensuring adequate rehabilitation. Better VAS scores, indicating less pain, were obtained for the DAA group during the first few days after the operation. Similarly, Wang reported both better VAS scores immediately after the operation and better Harris hip score results in the second and fourth week following the procedure. No other differences were found between the DAA and PLA groups [33]. The use of the DAA is also associated with a lower chance of iatrogenic damage of muscle structures, shorter procedure, less intraoperative blood loss and less postoperative pain, resulting in faster mobilization following the operation [13–17].
As indicated by our present findings, the DAA approach is associated with not only a shorter procedure but also a significantly shorter stay in the ward. In our opinion, the significant difference in LOS observed in the present study between approaches stems from the differences in tissue trauma during the operation. The greater tissue trauma in the case of PLA results in greater pain and limitation of independent functioning during the first postoperative days, and thus lower fulfillment of the discharge criteria.
The literature provides no standardized criteria that the patient must fulfill on the day of discharge following THA: each researcher devises a specific criterion believed to be the most appropriate for a given population [34]. In Poland, the mean time to rehabilitation is 109 days; therefore, in our case, the most important criteria were the period of time before independent functioning, and a VAS score below 3 successfully treated with the help of the first and second levels of the analgesic ladder. Our criteria were based on the works of Larsen and of Lazie [26, 34].
Selected works demonstrate that shorter hospitalization after THA may yield a range of benefits for patients. A correlation was observed between shorter LOS and better long-term postoperative results, as well as with greater satisfaction with the treatment, as reported by Husted et al. and Larsen et al. [25, 26], among others. In addition, Yannick et al. note that the introduction of a 24-hour fast-track procedure after THA allows for effective postoperative rehabilitation and better education among patients, despite the LOS being significantly shortened [20].
Complications associated with longer hospitalization time are not only a medical problem but also generate additional economic problems. The economic aspect of LOS is an important one. Shorter LOS and the introduction of a fast-track procedure after THA may be associated with a reduced risk of thromboembolic events and deep periprosthetic infections [22, 27]. In the US, the annual costs associated with revision hip replacement after septic loosening increased from 320 million to 566 million dollars during the period 2001 to 2009 [28, 29]. A study in Finland found that periprosthetic infection increased treatment costs threefold compared to uncomplicated primary THA [30].
In Poland, the THA procedure is paid by the public insurance (NFZ) as a flat rate, and as the LOS in the hospital has no effect on the cost of reimbursement to hospital. The total cost of treatment is reduced by a shorter stay in hospital and by a shorter duration of the procedure [31–35]. In the present study, we achieved a saving of PLN 5465.96 per procedure. Shorter LOS can also have a positive impact on the efficiency of the ward and operating theatre, and shorten waiting times for surgery. A UK House of Commons report of 2003/2004 indicated that shortening LOS by 1 day in a 40-bed ward allows 146 additional THA treatments to be performed per year [36]. In the present study, the use of the MIS DAA approach resulted in hospitalization time being shortened by 3.8 days. The costs associated with the treatment of postoperative complications can also be lowered indirectly by reducing the risk of infection, the need for transfusion of blood products during MIS DAA, and the risk of thromboembolic events [22, 28–30, 37].
The present study does have some limitations. Patients were operated on by two different specialists. Surgeons who routinely perform THA, both in Poland and elsewhere, typically choose one preferred approach in which they train and specialize. It is important to emphasize that in this case, both surgeons had similar experience and had performed a similar numbers of procedures. In addition, due to the number of procedures performed, they were not subject to the learning curve effect.
Another limitation is that the patients from the DAA and PLA groups were treated in two different centers. However, although the rehabilitation and perioperative care protocols are standardized between the two departments, and hence any such differences should be minimized, this fact does bear consideration when interpreting the results.
Our findings, however, clearly indicate that the MIS DAA approach has a significant influence on shortening hospitalization and procedure duration, which is associated with a number of benefits for both the patient and the hospital. However, further randomized prospective studies are needed to more precisely evaluate this relationship.
In conclusion, the MIS DAA procedure is a safe and less traumatizing surgical approach for hip arthroplasty which allows faster primary mobilization post-operatively, shorter procedure time and sooner discharge from hospital than standard PLA; however, similar improvements in function and quality of life were observed in both groups of patients, i.e. both the DAA and PLA groups. It appears that MIS DAA is the optimal surgical approach to THA both for patients wishing to quickly return to mobility and for the operating center which intends to significantly reduce its costs of hospitalization.