Atrial fibrillation (AF) is the most common clinical cardiovascular disease, and one of the most important arrhythmia diseases; AF can increase the morbidity of stroke, arterial embolism and heart failure [1]. AF can result in the loss of effective atrial contraction and diastole, and lead to deterioration or loss of cardiac pumping function accompanied by irregular ventricular rhythm [2]. At present, the incidence of AF in adults is about 0.4–1%, and the incidence of AF in patients over 60 years old is 2–4%. In addition, even without cerebral infarction, AF can cause cognitive impairment in patients, atrophy of the hippocampus, and increase the prevalence of Alzheimer’s disease [3]. AF is the main cardiovascular disease that causes increased mortality and increased health care spending. In the United States, about 2.3 million people suffer from AF disease, and this number is expected to increase to 5.6 million by 2050 [4, 5]. At present, the main treatment methods of AF are internal, surgical radiofrequency ablation and drug conversion therapy, however, due to the high recurrence rate of atrial fibrillation, there is no effective and safe treatment method. This is attributed to the complicated pathogenesis of AF that has not been completely clarified.
Inflammatory pathogenesis is one of the important mechanisms of atrial fibrillation. More and more evidence supports the role of inflammation in the pathophysiology of AF, which indicates that the inflammatory pathways is a potential therapeutic target, inflammation and related immune reactions are involved in the occurrence and maintenance of AF [6, 7]. Inflammatory pathways can lead to atrial electrical and structural remodeling and thrombogenesis in patients with AF. Many inflammatory factors can cause fibrosis changes in the myocardium, which produces a substrate for the onset of AF. For instance, tumor necrosis factor (TNF) can activate transforming growth factor β (TGF-β) signaling pathway and myocardial fibroblasts, increase secretion of matrix metalloproteinases-2 (MMP-2) and MMP-9, which mediate atrial remodeling [8]. In the SD (Sprague Dawley) rat model of aseptic pericarditis, interleukin-17A (IL-17A) can aggravate myocardial fibrosis and promote the occurrence of AF. Inhibition of IL-17A expression can reduce myocardial fibrosis, which shows a therapeutic effect in AF [9]. Many studies have found that IL–17A can stimulate the release of pro-inflammatory cytokines (IL-1β, IL-6 and TGF-β1), which participate in the pathogenesis of myocardial fibrosis, thereby promoting the occurrence of atrial fibrillation [10, 11].
In the study of AF-related drugs (Colchicine and Curcumin) by transcriptome [12] (Figure 1 A, each group had three rats), we found that the IL-17 pathway is highly expressed in the AF rat model (The rat model of AF was induced by Ach (66 μg/ml) – CaCl2 (50 mg/ml) with a dose of 0.1 ml/100 g via the tail vein injection for 28 days, Atrial fibrillation model standards: the electrocardiogram showed that the P wave disappeared and the f-wave appeared as the typical atrial fibrillation ECG). The Colchicine treatment group and Curcumin treatment group were given colchicine by gavage once a day for 24 days at a therapeutic dosage of 0.8 mg/kg and 4 ml/kg/d (concentration: 50 mg/ml), and the expression of IL-17 pathway was significantly down-regulated after drug intervention (Figure 1 D) [12]. The emerging role of IL-17 as a hallmark proinflammatory cytokine of the adaptive immune system produced by a new T helper cell subset termed “Th17” has received considerable attention. IL-17 is an important pro-inflammatory cytokine that plays an important role in the innate and acquired immune systems of the body. The IL-17 family can promote the body to resist infection of various pathogens, and is closely related to the occurrence and development of autoimmune diseases, tumors and other diseases [13]. The family consists of six members: IL-17A, IL-17B, IL-17C, IL-17D, IL-17E (also known as IL-25) and IL-17F. Among them, IL-17A and IL-17F play an important role in Th17 (T helper cell 17) cellular immunity. IL-17A and IL-17F are 50% homologous and can form either homologous dimers or heterodimers that bind to IL-17RA/IL-17RC, which can activate downstream nuclear factor кB (NF-кB) and mitogen-activated protein kinase (MAPK) signaling pathways by acting on signaling complex IL-17R-ACT1-TRAF6 [14]. The IL-17 pathway participates in the body’s anti-infection immunity, pathological inflammatory response related to autoimmune diseases, and the occurrence and progression of tumors.
Figure 1
A – Transcriptome experimental workflow. B – Heatmap of hierarchical clustering of DEGs among the blank group, AF group and Drugs treatment group (X axis represents each comparing sample. Y axis represents DEGs. Colouring indicates the log2 transformed fold change. High: red, Low: blue). C – The GO classification results among the blank group, AF group and Drugs treatment group (X axis represents number of DEG. Y axis represents GO term). D – Pathway classification of DEGs among the blank group, AF group and Drugs treatment group (X axis represents enrichment factor. Y axis represents the pathway name. The color indicates the q-value (high: white, low: blue), the lower q-value indicates the more significant enrichment. Point size indicates DEG number (The bigger dots refer to larger amounts). Rich Factor refers to the value of the enrichment factor, which is the quotient of foreground value (the number of DEGs) and background value (total Gene amount). The larger the value, the more significant enrichment

Comprehensive genome-wide screening of the transcriptome has shown the mechanism of disease differentiation and possible diagnostic and treatment value. Analysis of the expression profiles among the Blank group, AF group and Drugs treatment group and the profound analysis of Differentially Expressed Genes (DEGs) changes may contribute to the comprehensive understanding of the pathology of AF and potential therapeutic mechanisms. Hierarchical clustering analysis revealed that the genomic expression of three groups of tissues had differences in transcriptomics profiles (Figure 1 B). Genes, such as IL17a, IL17b, Mapk13, Mapk15, Lcn2, Cxcl10, Rsph10b, Ccl11, Irx3 and Ccl20 are included in the IL-17 pathway (Table I). Moreover, these genes were highly expressed in the AF group and significantly down-regulated after drug intervention, indicating that these genes can be used as potential therapeutic targets in IL-17 pathway. In addition, we perform the Gene Ontology (GO) classification and functional enrichment with DEGs. GO has three ontologies: molecular biological function, cellular component and biological process, most of them participated in the cell process, cell part, binding, etc (Figure 1 C).
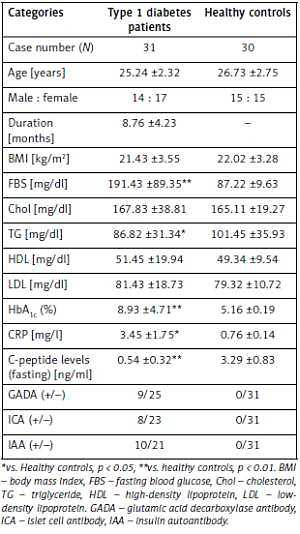
Table I
Details of key genes in the combination of DEGs in the IL-17 pathway
In conclusion, we provide an integrative analysis of transcriptomics for studying the pathogenesis of AF. We first discovered that the IL-17 signaling pathway plays an important role in the pathogenesis of AF and that some genes can be used as potential therapeutic targets for AF. Due to the importance of the IL-17 pathway in the pathology in this study, targeting differential genes in the IL-17 pathway may become new diagnostic and therapeutic methods in the future.