Introduction
One of the important factors affecting the fate of societies from prehistory to modern times is major epidemics. The most significant are those of a pandemic nature, covering large areas, which have contributed to unprecedented mortality. Epidemic outbreaks have always been associated with a sense of danger and widespread anxiety and insomnia. On March 11, 2020, the World Health Organization declared a COVID-19 pandemic caused by a new strain of coronavirus (SARS-CoV-2) [1]. Almost every person was forced to reorganize their routine functioning in a very short period of time. The danger of infection with an unknown and dangerous pathogen and the dramatic change in daily life became a source of stress. The fear of losing their own health and lives, as well as those of their loved ones, the vision of potential livelihood and economic problems, and forced isolation, negatively affected the well-being of most people. Particularly vulnerable to stress were people whose professional activities involved potential infection by an unexplored virus. During all outbreaks, medical personnel are the group most vulnerable to their chronic consequences. In addition to the increased risk of contracting the disease, working in health care is associated with psychological ailments, which include chronic stress. During the 2002–2003 SARS outbreak, significant mental deterioration was observed among medical workers, including the emergence of a depressive state leading to post-traumatic stress disorder (PTSD) and sleep disturbances in the form of insomnia. Similar symptoms were found in frontline workers fighting the Ebola virus in 2014–2016 [2]. Emergency medical team personnel are particularly vulnerable to situations of overload. In addition to the stress factors that are present in most workplaces, such as poor technical conditions, job insecurity, and a multitude of duties, employees are additionally burdened by a sense of great responsibility, 24-hour on-call duties, and the awareness of saving health and life, which are inevitably accompanied by suffering and death [3]. In the COVID-19 pandemic, the most commonly reported mental health abnormalities appeared to be anxiety disorders, feelings of loneliness, frustration, mood disorders, somatization disorders and poor sleep quality [4]. The pandemic period did not always allow the internal rhythm of sleep and wakefulness to be reconciled with the time of day and night. The problems, worries and constant stress that emergency workers had to deal with contributed to the development of sleep disorders. In addition to the above, shift work, usually 12-hour shifts, which causes dysfunctions in circadian sleep and wakefulness rhythms, was also significant [5]. An association between insomnia, exhaustion and secondary traumatic stress (STS) has been observed among frontline medical personnel of the COVID-19 pandemic, including paramedics. This problem is widespread, so it seems very important to find factors that influence insomnia among paramedics in the era of the SARS-CoV-2 pandemic [6]. An attempt was made by the authors of the present study to identify factors that may influence the occurrence of sleep disorders among paramedics during the COVID-19 pandemic.
The aim of this study is to identify factors influencing the development of sleep disorders among paramedics working during the COVID-19 pandemic.
Material and methods
An online diagnostic survey method was used to conduct the study, consisting of a proprietary questionnaire and standardized questionnaires: the Athens Insomnia Scale (AIS) and Epworth Sleepiness Scale. The survey was conducted between 10/11/2020 and 14/01/2021. In order to reach the largest possible group of paramedics, the Google questionnaire was published on social networks (Facebook – paramedic professional groups, Instagram) and online forums designed for paramedics. A total of 387 people (280 men (72.35%) and 107 women (27.65%)) working as paramedics in outbound teams during the COVID-19 pandemic participated in the survey. Table I shows the sociodemographic characteristics of the study group.
Table I
Sociodemographic characteristics of the study group
The Athens Insomnia Scale (AIS) is a short, eight-item questionnaire that allows quantitative measurement of insomnia symptoms based on ICD-10 criteria. In the validation studies conducted, high reliability and accuracy of this tool were demonstrated. The Athens Insomnia Scale contains 8 questions on: frequency and severity of sleep disturbances, sleep maintenance, morning awakening, sleep quality, mood and daytime functioning. A total score of 6 or more on the scale was considered a value to infer the presence of insomnia with high probability (sensitivity of the scale – 93%, specificity of the scale – 85%) [7, 8]. The AIS is one of the most widely used scales, both for diagnostic purposes and to determine the effectiveness of insomnia treatment [9, 10].
The Epworth Sleepiness Scale (ESS) is a scale used to assess sleep disorders, including in the diagnosis of sleep apnea syndrome. It is classified as a self-assessment scale and consists of the respondent’s determination (on a scale of 0-3) of the likelihood of falling asleep in 8 everyday situations. Interpretation of Epworth scale scores: 0–10 points – normal score, 11–14 points – mild sleepiness, 15–18 points – moderate sleepiness, more than 18 points – severe sleepiness [5].
The study also used a self-administered survey questionnaire, which included questions about gender, marriage, length of work experience as a paramedic, and family relationships. The impact of the pandemic on the frequency of use of stimulants, such as alcohol and psychoactive substances, which included marijuana, cocaine, amphetamines, heroin and mephedrone, was also assessed. Patients were also asked about the use of sleeping and psychoactive drugs. The question on the use of sleeping aids did not specify specific medicinal substances.
Statistical analysis
The study used the Excel 2021 computer program and the R language in the RStudio environment with the implementation of the pROC package to analyze the data obtained. The results obtained were presented in numerical and percentage form – as the ratio of the number of people indicating a given answer to the total number of people taking part in the survey. Quantitative variables in our data set were reflected as mean ± standard deviation. Ratings of relationships with family members were presented as an 11-point scale, where 5 indicated maintaining family contacts after the pandemic at the same level as before the pandemic. Values of 0–4 indicated a deterioration of relations within the family, and scores of 6–10 indicated an improvement in relations with family members, compared to the situation before the pandemic. The study used Student’s t-test with Forsyth Brown’s test for homogeneity of variance to represent quantitative variables. We also used analysis of variance (ANOVA), with Tukey’s post hoc test for sample size inequality, to compare more than two samples, using a backward stepwise method. In our study, values of p < 0.05 were considered statistically significant.
Ethics
Ethical approval for the study was obtained from the University Bioethics Committee of the Silesian Medical University in Katowice (PCN/CBN/022/KB/233/121). Before taking part in the study, respondents were informed that their participation was fully voluntary and that all information collected would be kept anonymous. Each participant was free to withdraw from further participation in the study at any time, without any consequences.
Results
The total number of paramedics who took part in the survey was 387. All of these individuals declared that they worked in the Emergency Medical Service during the COVID 19 pandemic. The majority of the respondents were men (72.35%). A detailed description of the study group is presented in Table I.
Table II shows the general characteristics of the study group with respect to the AIS and Epworth scales, considering both men and women. The average number of points obtained by the study participants in the AIS scale is 2.73, with a minimum score of 0.00 and a maximum score of 6.00. In the Epworth scale, the respondents obtained an average of 9.61 points, with a minimum score of 0.00 and a maximum score of 23.00.
Table II
General characteristics of the group in relation to the scales analyzed
| Variable | No. of observation | Average | Minimum | Maximum | Standard deviation |
|---|---|---|---|---|---|
| AIS | 387 | 2.73 | 0.00 | 6.00 | 1.54 |
| Epworth | 387 | 9.61 | 0.00 | 23.00 | 5.06 |
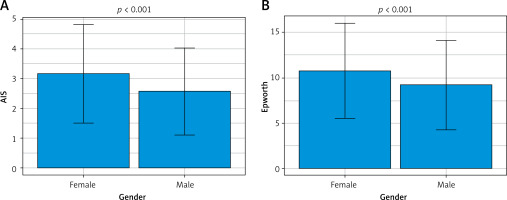
Figure 1 compares scale values by gender. Significantly higher values of the analyzed scales were observed in women, compared to men. In the AIS scale, 3.6% of women scored 6–10 points, which was considered the limit of normal and qualification for mild sleep disorders, as many as 96.4% of women scored within the normal range, i.e. ≤ 5 points. 2.9% of men scored 6–10 points on the AIS scale presenting mild sleep disorders. In the Epworth scale, 29.9% of women scored normal (0–10 points), 16.8% of women scored 11–14 points indicating mild sleepiness, 28.00% of women presented moderate sleepiness scoring 15–18 points, and severe sleepiness requiring medical consultation was presented by 25.2% of women who scored more than 18 points in the questionnaire. In the Epworth questionnaire, 41.1% of men scored normal (0–10 points), 22.1% of men scored 11–14 points indicating mild sleepiness, 22.1% of men presented moderate sleepiness scoring 15–18 points, and symptoms of severe sleepiness requiring medical consultation were presented by 14.6% of male paramedics scoring more than 18 points (Figure 2).
Significantly lower Athens Scale scores were observed in married individuals compared to those who were single, with no significant differences between those in an informal relationship and the other groups. Epworth scale scores differed significantly between married and unmarried individuals (Table III).
Table III
Comparison of values obtained in the studied scales by marital status
| Variable | Married | Unmarried | Casual relationship | P-value | |||
|---|---|---|---|---|---|---|---|
| Average | SD | Average | SD | Average | SD | ||
| AIS | 2.47 | 1.46 | 3.03 | 1.58 | 2.93 | 1.60 | < 0.001 |
| Epworth | 8.95 | 4.73 | 9.23 | 5.34 | 11.25 | 5.07 | < 0.001 |
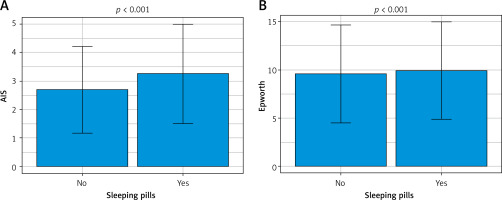
Those using sleep medication during the COVID-19 pandemic scored significantly higher on the AIS and Epworth scales.
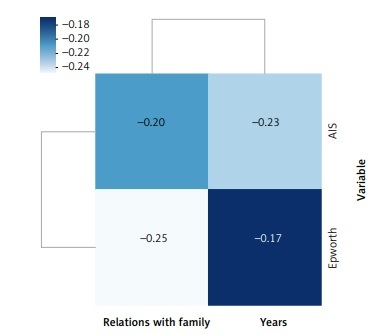
In the study conducted, a significant negative correlation was observed between the scores of the various scales and the assessment of relations with the family (Figure 3). Those scoring higher on the questionnaires showed worse relations with family members.
Figure 3
Correlations between the obtained values of the scales and the assessment of relations with the family
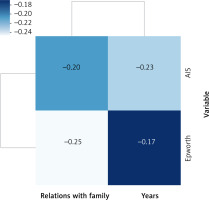
Significant negative correlations were also found between the scores on the AIS and Epworth scales and the subjects’ age and length of service (Table IV). Older subjects and those with more seniority in the paramedic profession obtained significantly lower values of the scales analyzed.
Table IV
Correlations between the obtained values of the scales analyzed and age and length of service
| Variable | Age | Length of service in the emergency medical service |
|---|---|---|
| AIS | −0.21 | −0.23 |
| Epworth | −0.10 | −0.17 |
Logistic regression analysis confirmed the significant effect of female gender, psychoactive substance use and sleep aids on the risk of insomnia based on the AIS scale.
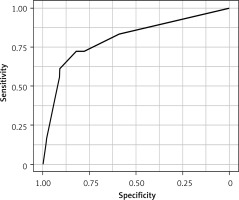
The ROC curve was used to visualize the ratio of true positives (sensitivity) to the percentage of false positives (specificity) at each probability level. The ROC curve demonstrates the value of a given test by illustrating the number of misclassifications for a given cutoff point (Figure 4).
Discussion
The study presented here was designed to identify risk factors for the development of sleep disorders among paramedics working during the COVID-19 pandemic, using a proprietary questionnaire and standardized scales: AIS and Epworth. This cross-sectional study included 387 subjects, and in light of the results obtained, the supposition that there was a deterioration of sleep quality among paramedics during the first period of the COVID-19 pandemic was confirmed. Of the 387 subjects, 4.65% of paramedics were identified to have mild sleep disorders scoring between 6 and 10 points on the AIS scale. In contrast, as many as 62.0% of paramedic members presented symptoms of sleepiness on the Epworth scale. Higher values of the analyzed scales were observed among women compared to men. On the basis of the AIS scale, mild sleep disorders were found in 3.6% of women, while in the Epworth scale, symptoms of increased sleepiness were declared by as many as 70.0% of women. These data are similar to results obtained in a study conducted in China, which found that women reported more severe symptoms of depression, anxiety and insomnia [11]. Similarly, Rossi et al. in their study in Italy obtained results confirming a higher prevalence of psychological problems among young women and workers with direct patient contact [12]. Also, Tuan et al. observed that during the second wave of the pandemic, symptoms of depression and insomnia were most frequently reported by nursing staff. The above data are due to the fact that nurses are mainly women, who are more predisposed to develop anxiety and depressive disorders than their male colleagues [13]. Similar results were obtained by Krupa et al., who observed an increase in sleep disorders among medical workers during the COVID-19 pandemic, with nurses presenting the highest levels of insomnia [14].
In contrast, in a study conducted in Jordan by Oteir et al., no differences were observed between men and women in the frequency of reported anxiety and insomnia symptoms, which may have been due to the lower proportion of women, who made up only one-fifth of the participants in the study group. In addition, it was found that among medical personnel, paramedics presented the highest mean scores on the anxiety, depression and insomnia scales, although no statistically significant differences were observed between other medical professions. The greater responsibility and workload during the pandemic made paramedic workers more prone to fatigue, stress, depression and, consequently, sleep disturbances [15].
There are many studies confirming that this occupational group is at risk of developing sleep disorders associated with the COVID-19 pandemic. Pappa et al., based on a meta-analysis of 13 cross-sectional studies with a total of 33,062 participants, provided evidence that a significant proportion of health care workers experienced mood disorders, anxiety and insomnia during the pandemic. The prevalence of anxiety disorders was estimated at 23.2% in 12 studies, depression at 22.8% in 10 studies, while sleep disorders were assessed in five studies with a total prevalence of 38.9% [16]. Analogous results were obtained by Zhang et al., who found that among 1,563 participants, 36.1% of medical personnel suffered from insomnia during the COVID-19 outbreak [17]. A study by Huang et al. also proved that during the COVID-19 pandemic, the Chinese public struggled with poor sleep quality and a higher incidence of insomnia. They found that there were no gender differences in anxiety, which contradicts the results of our earlier study and those of other authors [18–20].
The likely cause of sleep problems in stressful situations may be due to stimulation of the hypothalamic-pituitary-adrenal axis, leading to an increase in stress markers such as cortisol, which disrupt the natural sleep rhythm. The resulting shortened or disrupted sleep causes a further increase in these markers, thus fueling a vicious cycle of stress and insomnia [17]. Undoubtedly, the primary source of stress for the medical personnel in our study was the COVID-19 pandemic itself, from which other factors affecting functioning, such as deterioration of relationships with the family, may have resulted.
Sleep disorders and the development of psychopathological symptoms have been found in a number of studies around the world assessing the health status of health care workers during the COVID-19 pandemic. Erazo et al. reported that among 1,028 participants in a study in Ecuador, insomnia was found in 16.3% of them. Depressive symptoms were reported by 27.3%, anxiety disorders by 39.2%, and post-traumatic stress disorder (PTSD) symptoms were present in as many as 43.8% of them. Factors associated with the development of the above disorders were female gender, working in the province most affected by the pandemic, being a doctor without a specialty, and lack of adequate protective equipment [21]. A study by Tuan et al. assessed the prevalence of mental disorders among health care workers during the second wave of the pandemic in Vietnam. The following results were obtained: 26.85% of the 611 participants presented symptoms of anxiety, 34.70% presented symptoms of depression, 34.53% reported insomnia, and 46.48% reported general mental problems [13]. Al-Otaibi et al. reported that during the COVID-19 pandemic in Kuwait, insomnia was found in 58.5% of healthcare workers, and 65.1% of respondents developed poorer sleep quality [22]. The above data confirm the increased prevalence of sleep problems among paramedics working during the COVID-19 pandemic.
By evaluating the relationships between age and seniority and scores obtained on the AIS and Epworth scales, the authors of the present study inferred that work experience and older age have a protective effect on the incidence of insomnia among paramedics. Our results agree with those obtained by Huang et al., who observed that the younger age of the population (< 35 years) was associated with a higher risk of psychiatric disorders [18].
Baka took the opposite view, finding that levels of insomnia, anxiety and exhaustion were higher in older workers and those with longer tenure. Fear of contagion and disease development among older medical personnel may have been due to the highest mortality rate in this age group and fear of harm from an unknown pathogen [23]. A study by Patel et al. found that the older a person is, the more likely he or she is to experience mental problems and insomnia [24].
Other significant factors associated with a high risk of sleep disorders in the respondents we studied were not having a partner/daughter and the use of sleep medications. Statistical analysis showed that married paramedics had significantly lower Athens Scale scores compared to those who were single, with no significant differences between those in an informal relationship and the other groups. Epworth scale scores showed a significant difference in scores between married and unmarried individuals. This was confirmed by Erazo et al., who observed a lower likelihood of anxiety disorders among medical personnel who had a partner and were in stable relationships [21].
In our study, those scoring higher on the scales reported worse relationships with family members. Similarly, in China, it was found that paramedics who cared for patients suspected of having SARS-CoV-2 infection reported worsening family contacts. This was due to the fact that family and friends maintained social distance and were unable to provide adequate social support to the paramedics. Worse relationships within the family translated into increased stress levels, depression and a greater predisposition to develop sleep disorders [25]. The majority of paramedics reported a negative impact of the pandemic on interpersonal interactions, due to fear of contracting the disease from another person, especially from those providing medical care to patients with SARS-CoV-2 infection. Fear of transmitting the disease to family, friends and children resulted in avoidance of contact with paramedics. In addition, it was found that as a result of the imposed requirements of social distance and compliance with the Ministry of Health’s recommendations, visits to friends were reduced. The public avoided meeting paramedics, who were perceived to be infected with SARS-CoV-2 because of direct contact with patients who were sick or suspected of being infected [26, 27].
There is no doubt that our study provides important data on the development of sleep disorders among paramedics and other health care workers during epidemics that are predicted in the next decades. The results discussed above point to the need to identify ways to prevent and mitigate mental health risks for health care workers and adapt interventions in pandemic settings. The Ministry of Health and other government bodies should consider establishing multidisciplinary teams to provide mental health support to paramedics working under stressful conditions. Perhaps the interventions put in place would maintain adequate numbers of personnel working during future pandemics, preserve quality and capacity, and prevent the development of serious health disorders among EMTs. It would be valuable to conduct a future study evaluating the effectiveness of the applied methods of coping with stress among a specific population of health care workers such as paramedics.
The questionnaire conducted in an online format carries certain limitations. In order to fully achieve the research objectives, we used a proprietary questionnaire, in addition to the validated mental health assessment scales, which has not been validated. It is impossible to make a full psychiatric diagnosis solely on the basis of the self-assessment questionnaires used; hence we did not make specific nosological diagnoses but focused on assessing the intensity of symptoms suggestive of sleep disorders in the surveyed respondents. On the other hand, data obtained from online questionnaires is a recognized method of obtaining reliable data, thanks to the elimination of the stress of direct contact with the subject.
In conclusion, women working in the Emergency Department scored significantly higher on all analyzed scales assessing sleep disorders. Those in informal relationships and those who were single showed a higher risk of developing sleep disorders compared to those who were married. Paramedics using sleep medications during the COVID pandemic-19 were more likely to present symptoms of sleep disorders. EMTs declaring good relationships with their family members were less likely to present symptoms of sleep disorders. Older people and those with longer tenure obtained lower values in all scales analyzed. Risk factors for insomnia were female gender, not having a formal partner, young age and low work experience.