Medical procedures using ionizing radiation are invaluable in modern medicine, but we must not forget that they carry risks related to exposure to ionizing radiation. The number of diagnostic and therapeutic procedures using ionizing radiation, especially computed tomography, has increased significantly in recent decades [1–3]. Computed tomography, alongside interventional radiology, is the largest source of patient exposure to ionizing radiation in medical procedures [4–6].
In the case of examinations of pregnant women using ionizing radiation, individual justification is particularly important, taking into account the risk of using ionizing radiation for the fetus and the risk of delaying the diagnostic examination or interventional procedure for the health and life of the mother. The method of performing the medical procedure requires optimization using all available tools to ensure that the doses resulting from exposure for both the woman and the unborn child are kept at the lowest possible level allowing the required medical information to be obtained [7–9]. The aim of this study was to analyze the doses received by the fetus in the womb during procedures using fluoroscopy and computed tomography.
Methods
In the measurements of exposure of pregnant women, highly sensitive thermoluminescent detectors (TLDs type MCP-N manufactured by Radcard, Poland) were used [10, 11]. Calibration of TL detectors for measurements with an anthropomorphic phantom was performed in the air kerma (Ka) unit using the ISO N-80 reference energy spectrum [12] according to procedures developed at NIOM. An overall 20% measurement uncertainty was estimated, and it is mainly due to the energy dependence of TL detectors.
To simulate the exposure of a pregnant woman to ionizing radiation, an anthropomorphic phantom from CIRS was used. This phantom simulates the structure of an adult woman with a height of 173 cm and weight of 73 kg. The phantom was additionally equipped with female breasts, and a bag filled with water was placed on the pelvis area, simulating a pregnant belly. Due to the size of the fetus in the mother’s womb, TL detectors were placed in three areas of the pregnant abdomen, i.e., upper, middle, and lower.
The measurements were performed on two types of devices. The first was the Axiom Artis Zee Ceiling angiograph by Siemens used for procedures in the field of interventional cardiology. On this device, the radiation beam was directed at the heart area using various projections, allowing the effect of the beam angulation on the dose received by the fetus to be determined. For each position of the lamp, measurements were performed without the pregnant abdomen covered with a protective apron and with the pregnant abdomen covered. Parameters of the beam used for measurements: 74 kV, 200 mAs.
The second type of device used to determine the level of exposure of pregnant women was the Canon Aquilion Prime CT scanner by Canon. This is a 256-row CT scanner. Fetal exposure was determined during scans in three areas: head, chest, and whole body. Similar to measurements on the Axiom Artis Zee Ceiling angiography device, measurements were performed with and without a protective apron (except for whole body scanning, when no apron was used). For the head protocol, the scanning parameters were 120 kV, 320 mA; for the chest protocol, 120 kV, 380 mA; for the whole body protocol, 120 kV, 320 mA. To increase the accuracy of the reading, each measurement was performed using 5 series of helical scans. All obtained results were converted into one series of scans, i.e., one examination. A protective apron with a lead equivalent of 0.5 mmPb was always used to cover the pregnant abdomen. In all measurements, an assessment of the exposure of women’s breasts during individual exposures was also made.
Results
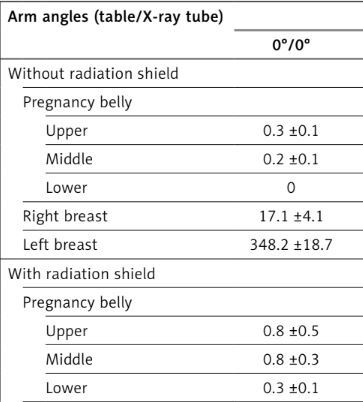
Table I shows the dose levels that the female breasts and fetus receives during interventional cardiology procedures using the Axiom Artis Zee Ceiling angiography system. Due to the relatively low level of exposure, the dose values are expressed in μGy per 100 s.
Table I
Level of exposure to the fetus and breasts of women during interventional cardiology procedures using the Axiom Artis Zee Ceiling angiography system
Table II shows the level of exposure to the fetus and breasts of women undergoing diagnostic procedures using a CT scanner.
Table II
Level of exposure to the fetus and breasts of women undergoing diagnostic procedures using a Canon Aquilion Prime CT scanner
Discussion
As shown in Table I, fetal exposure during interventional cardiology procedures depends on the angle of incidence of the ionizing radiation beam. The closer the radiation beam passes to the fetus, the greater is the exposure. This is very visible when the arm and table are positioned at 0°/CRAN 20°, where the radiation beam passes from the patient’s legs relatively close to the pregnant abdomen. Of course, in none of the analyzed cases of table and arm positioning did the radiation beam pass directly through the fetus; however, in some positions it passed relatively close to the pregnant abdomen.
This work also analyzed the effect of using a radiological shield on the pregnant abdomen. Comparison of the measurement results with and without the use of a protective apron on the pregnant abdomen area showed no statistically significant differences in the dose readingsg (p = 0.001). Looking at the absolute values for the C-arm projections 0°/0° and 0°/CRAN 20°, it can be seen that the exposure of the fetus is greater when the shield is used than when it is not. The fact that there is no statistically significant difference between the readings in these situations confirms the validity of the recommendations of the Canadian Radiological Society [13, 14]. In order to realistically assess the exposure of women during procedures performed using fluoroscopy, an analysis of the exposure time during coronary angiography and coronary angioplasty was performed in patients who underwent these medical procedures in the period of 12 months before the phantom measurements were performed. As a result of the analysis, it was found that during coronary angiography the average radiation exposure time is 190.4 ±273.8 s (min.–max: 48–1342s), and in the case of coronary angioplasty it is 764.0 ±489.5s (min.–max.: 427–2296 s). Especially in the case of coronary angiography, the exposure times differ greatly. The standard deviation exceeds the value of the obtained mean.
In order to estimate the dose to the fetus, it is necessary to take into account the radiation emission times during individual procedures and the measured dose rates presented in Table I. The highest measured value is 4.1 μGy/100 s. This means that taking into account the average duration of coronary angiography, the fetus can receive 7.8 μGy, while during coronary angioplasty it can receive 31.4 μGy. In a worse-case situation and taking into account the longest radiation emission times, we obtain doses of 55.2 µGy and 94.4 µGy for coronary angiography and coronary angioplasty, respectively. Assuming that these procedures are not performed repeatedly in the patients studied (the probability of their repeated performance in a pregnant woman within 9 months is particularly low), the level of exposure of the fetus in the mother’s womb is very low.
Analyzing the exposure of the breasts in pregnant women undergoing interventional cardiology procedures, a significant increase in the radiation dose rate is visible compared to the abdominal area (fetus), especially for the left breast. This is obvious due to the position of the left breast in relation to the heart. The maximum dose rate was measured for the left breast at the X-ray tube position of 0°/CAUD –20°. Taking into account the average times of ionizing radiation emission during coronary angiography and coronary angioplasty, the breast exposure was calculated as 1.22 mGy and 4.88 mGy, for right and left breast, respectively.
The exposure of pregnant women during examinations using a computed tomography scanner is completely different. In this case, the most significant effect on the level of exposure is the range of scanning the patient’s body. When scanning the head area, the fetus in the mother’s womb receives a relatively small dose of ionizing radiation. In this case, the dose recorded is in the range of 1.9 µGy to 6.3 µGy. In the case of using a shield for the pelvic area, the doses were not recorded. However, it should be remembered that, similarly to interventional radiology procedures, no statistically significant difference was found between measurements with and without a shield (p = 0.001). Also, no significant difference was found between the doses received by the breasts in the examined women (p = 0.002). The doses to both breasts were on average 538 µGy and 420 µGy for the examination without a shield and with a shield, respectively. This is on average about 3% of the dose received by the breasts in women during scanning the chest area. Scanning the chest area is the largest ionizing radiation dose burden for the breasts in women. The doses for scanning with and without a pelvic shield are 15.9 mGy and 16.3 mGy, respectively. Similarly, the doses measured in the area of the pregnant abdomen increase in relation to imaging the head area. Here, a 94% increase in the dose is observed in the area of the pregnant abdomen in relation to scanning the head area. As in the previous analyzed cases, there is no statistically significant difference between the dose in the area of the pregnant abdomen with and without a shield (p = 0.011).
The greatest exposure for the fetus in the womb is scanning in the TRAUMA module – whole body scanning. In this case, the area of the pregnant abdomen receives an average of 4.6 mGy, while the breasts receive 6.6 mGy. In this case, the fetus is exposed to the highest dose out of all the cases analyzed in this study. The breasts of the women studied receive 42% of the dose recorded when scanning the chest area. Full-body computed tomography should be given special attention when analyzing the exposure of pregnant women. This type of examination is often performed in emergency cases in women admitted to hospital emergency departments as a result of road accidents or other injuries that threaten the patient’s life and health.
In conclusion, interventional cardiology procedures pose a significant risk to the unborn child. The recorded individual dose rates are not high compared to other medical procedures using ionizing radiation. However, due to the very large discrepancy in the times of ionizing radiation emission in individual procedures, the dose levels that the fetus may receive are already significant from the point of view of later health effects. In the case of computed tomography, the exposure of the fetus is at a very high level, which in the early stages of pregnancy may lead to its termination. The use of shields on the pelvic area or the pregnant abdomen does not affect the decrease in the dose to the fetus.