Hemiplegic migraine is a rare type of migraine with aura, and the only one that has a proven monogenetic background for its familial form [1]. The two main types are: familial (FHM), when the disease is present in more than one family member, and sporadic (SHM), which may cause more diagnostic issues and requires neuroimaging and other tests to exclude other causes [2]. According to the International Classification of Headache Disorders, 3rd edition (ICHD-3), to diagnoses a hemiplegic migraine, aura must occur, with both motor weakness and visual sensory and/or speech/language symptoms, which are all fully reversible [2]. Different types of FHM depend on the type of gene mutation responsible for the disease development. Thus, three main types: 1, 2, and 3, are described, and the genes with causal mutations for them are CACNA1A (calcium voltage-gated channel subunit alpha1 A), ATP1A2 (ATPase Na+/K+ transporting subunit alpha 2), and SCN1A (sodium channel protein type 1 subunit alpha), respectively [1, 2]. Those genes are responsible for approximately 75% of cases of FHM [3]. Hence, genes other than those can also result in FHM development, and the type of FHM with other gene loci mutations has been included in the classification [2]. Two genes have been recently described, PPRT2 (proline-rich transmembrane protein 2) and SLC1A3 (solute carrier family 1 member 3) [4].
Importantly, genes known to cause FHM are responsible for multiple functions in the human organism and thus are related to a variety of other impairments. Among them, different kinds of epileptic disorders can be found. The most common conditions related to the three main genes associated with FHM have been summarized in Table I [5–7].
Table I
The most common gene mutations responsible for FHM development, along with related conditions
| Gene | Related conditions | Source |
|---|---|---|
| CACNA1A | FHM1, intellectual disability, episodic ataxia type 2, epilepsy, autism spectrum disorder, paroxysmal tonic upward gaze | [5] |
| ATP1A2 | FHM2, epilepsy, reversible epileptic encephalopathy | [6] |
| SCN1A | FHM3, genetic epilepsy with febrile seizures plus, developmental and epileptic encephalopathies, autism spectrum disorder | [7] |
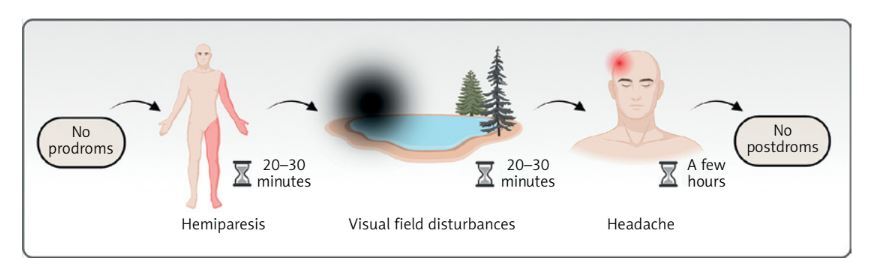
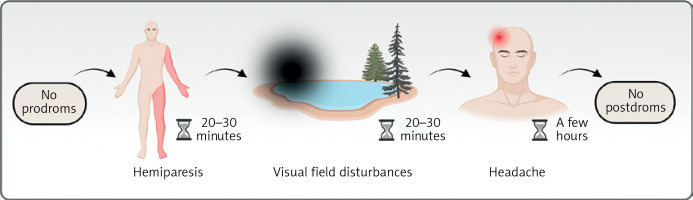
Herein, we present the case of a 70-year-old male patient who was admitted to the Department of Neurology due to the worsening of hemiplegic migraine attacks. The man has had a diagnosis of FHM for approximately 20 years and has remained under the care of an outpatient clinic with the same neurologist. During this time, he has experienced recurrent aura episodes, consisting of hemiplegia affecting either the right or left side of his body, sometimes followed by visual disturbances. Each symptom lasted for about 20 to 30 min. After the aura, a headache developed, usually bilateral in location, which was not a pulsating headache. The graphical presentation of consecutive symptoms is presented in Figure 1. The patient rated the intensity of the pain as reaching 10 out of 10 on the numeric rating scale (NRS), and it was accompanied by photophobia, nausea, and sometimes emesis. Given the clear clinical presentation complying with the ICHD-3 criteria, hemiplegic migraine was diagnosed.
Figure 1
A graphical presentation of consecutive symptoms of a complete migraine attack with all putative phases typical for the described family with hemiplegic migraine
The patient has kept a thorough headache diary, documenting each attack from the beginning of his disease; as a result, we can assume that from 2006 to March 2025, he experienced at least 64 episodes. The detailed description of each episode recorded by the patient is presented in Table II, translated carefully from his personal notes.
Table II
The information about the dates of the patient’s attacks, with additional notes based on the translated patient’s diary
In the laboratory tests performed during the hospitalization, the patient’s lipid parameters were above the upper reference level. All other tests were normal, including the complete blood count, electrolytes, coagulation parameters, hepatic parameters, renal parameters, creatine kinase (CK), thyroid-stimulating hormone (TSH), vitamin B12, and folic acid. In the magnetic resonance imaging (MRI), no signs of acute abnormalities were found, and brain atrophy of the frontal and temporal lobes was described.
While taking medical history from the patient, he informed that his son and granddaughter (the son’s daughter) were also affected by similar attacks. Both aforementioned family members, a 42-year-old man and a 14-year-old girl, suffered from recurrent episodes of transient focal neurological symptoms with headaches that were very comparable to those experienced by our patient. More precisely, episodes were comprised of a headache preceded by first visual disturbances, and subsequent unilateral motor weakness. The son reported that visual abnormalities were usually in the form of a scotoma in the field of view, similar to his daughter, who presented/had problems with entering through the door, hitting the doorframe. Regarding the ICHD-3 criteria for FHM, it is mandatory to identify at least one first- or second-degree relative who also meets criteria for FHM [2]. Thus, this thorough medical interview allowed for the diagnosis of FHM. Moreover, the girl underwent genetic tests, which revealed the pathogenic variant of the ATP1A2 gene, confirming the diagnosis of FHM type 2.
Another aspect concerns the history of suspected epilepsy diagnoses in all three family members. The described patient had previously been diagnosed with temporal epilepsy due to recurrent absence seizures. In the medical records from 2013, he was discharged from the hospital with the diagnosis of status epilepticus. However, he currently denies this diagnosis. The son had a history of seizure attacks with loss of consciousness during his adolescence, with one additional attack occurring in his early twenties. Subsequently, for about 20 years, no attacks have occurred. Finally, the granddaughter experienced febrile seizures as a child, but there were no further episodes, supporting the diagnosis of epilepsy.
The EEG examination conducted during the latest hospitalization revealed unilateral abnormalities characterized by slow-wave activity in the left hemisphere, with a tendency to involve the frontal areas of the right hemisphere, similar to the one performed in 2020 both while taking valproic acid, and the recent one also during gabapentin therapy. Additionally, the son’s EEG examinations, the latest of which was performed in November 2024, were abnormal, showing multiple delta waves localized in the left hemisphere, mainly in the left frontotemporal region. Finally, due to febrile seizures, the granddaughter underwent an EEG when she was just 20 months old, which indicated epileptiform activity. However, the EEG performed in 2022, when she was 12, revealed only slow wave activity localized in the right temporo-occipital area. She has not been taking any medications.
The final section of this case report addresses the suspicion of intracranial hypertension in the patient, which occurred in October 2022. In the MRI conducted at that time, features such as distension of the perioptic subarachnoid space, flattening of the posterior aspect of the globe, and an empty sella sign were described. The radiological presentation suggested intracranial hypertension. Given that the patient experienced recurrent headaches, this diagnosis could explain, in addition to migraine, those symptoms. However, no such characteristics were observed in the MRI conducted a month later, in November 2022. Therefore, the patient continued to be monitored. The MRI performed during the last hospitalization indicated only slight distension of the perioptic subarachnoid space, with no apparent signs of intracranial hypertension. Consequently, the suspicion has not been confirmed. No such information was reported for either the son or the granddaughter. During hospitalization, the patient gave written consent for the publication of his medical history in the form of a case report.
This case report highlights that, in addition to headaches, FHM may be associated with other symptoms linked to specific gene mutations. Consequently, FHM frequently co-occurs with various conditions, such as epilepsy. A holistic approach should be taken for these patients to identify any abnormalities that may affect the entire family.