A 24-year-old female presented to our hospital in July 2024 with a 10-year history of recurrent cough, expectoration, and diarrhea, which had worsened over the past 2 months. She also reported intermittent low-grade fever, bone pain, and 10 kg weight loss during this period. The patient has received the hepatitis B vaccination and denied other significant conditions as well as relevant family history. On admission, her body mass index was 14.5 kg/m2.
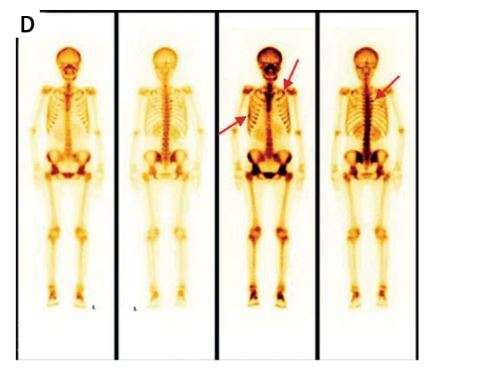
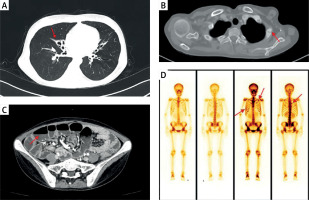
Routine stool tests and repeated stool cultures showed no significant abnormalities. Laboratory tests revealed: albumin 36.5 g/l (reference: 40–55), globulin 3.2 g/l (reference: 20–40), potassium 3.37 mmol/l (reference: 3.5–5.3), calcium 1.72 mmol/l (reference: 2.11–2.52), serum phosphate 0.27 mmol/l (reference: 0.85–1.51). 24-hour urine phosphorus 0.11 mmol/day (reference: 12.93–18.43), 24-hour urine calcium 0.01 mmol/day (reference: 2.5–7.5). Vitamin D level was 3.39 ng/ml (reference: 20–100); IgG 1.390 g/l (reference: 8.6–17.4), IgA 0.143 g/l (reference: 1.0–4.2), IgM 0.195 g/l (reference: 0.3–2.2); Alkaline phosphatase 143 U/l (reference: 35–135); Parathyroid hormone was significantly elevated at 314.5 pg/ml (reference: 15–68); C-reactive protein and erythrocyte sedimentation rate were within normal limits and so were T-cell, B-cell, and NK cell counts. Additionally, tests for anti-HBs, HIV antibodies, antinuclear antibodies, and serum immunofixation electrophoresis were all negative. Chest CT revealed bronchiectasis (Figure 1 A), pulmonary bullae, atelectasis in the right middle lobe, and fracture lines in the left second rib (Figure 1 B) and the right sixth posterior rib. No thymic and parathyroid abnormalities were observed. Abdominal enhanced computed tomography (CT) identified partial intestinal distention with gas and fluid, along with multiple enlarged mesenteric lymph nodes (Figure 1 C). Whole-body technetium-99 bone scan revealed metabolic activity in the left second rib and the right sixth posterior rib (suggesting fractures) (Figure 1 D). Whole exome sequencing, colonoscopy, and gastroscopy revealed no significant abnormalities. The terminal ileum biopsy showed mild chronic active inflammation and erosion. The biopsy of the duodenal bulb mucosa indicated chronic inflammation and gastric mucosal ectopia.
Figure 1
A, B – Lung CT showed bronchiectasis, atelectasis in the right middle lobe, and fracture lines in the left second rib. C – Abdominal enhanced CT identified partial intestinal distention with gas and fluid. D – Whole body scan revealed metabolic activity in the left second rib, the right sixth posterior rib, and slight activity in the axillary segment of the right seventh rib and left sacroiliac joint
Initial therapies, including montmorillonite powder, probiotics, levofloxacin, metronidazole, rifaximin, and sulfasalazine, were ineffective. Following the diagnosis of common variable immunodeficiency (CVID), the patient was treated with 20 g of intravenous immunoglobulin (IVIG). Despite this, diarrhea persisted. A subsequent 5-day course of methylprednisolone (30 mg/day) and a gluten-free diet also failed to alleviate symptoms. The patient then began monthly IVIG infusions (20 g). Although her cough improved after 2 months, her diarrhea did not show any improvement until 6 months later.
CVID is a primary immunodeficiency disease characterized by significantly reduced IgG levels accompanied by decreased IgM or IgA. The main clinical manifestations include recurrent infections, impaired vaccine responses, chronic lung disease, and gastrointestinal disorders [1]. A multicenter study revealed that 23% of CVID patients present with bronchiectasis [2]. Additionally, chronic diarrhea is frequently observed in CVID patients, with a prevalence ranging from 20% to 60% [3]. IVIG is the primary treatment for CVID but is generally less effective for intestinal symptoms. In contrast, glucocorticoids, immunosuppressants, and biologic therapies have demonstrated efficacy in some individuals [4, 5]. In this patient, diarrhea persisted despite treatment with antibiotics, glucocorticoids, and immunosuppressants, showing only slight improvement after 6 months of supplemental immunoglobulin therapy. Refractory diarrhea related to CVID significantly impacts patients’ quality of life and overall health. It is crucial to develop more effective treatments for this condition.
Bone pain was another major issue for the patient. Despite the absence of trauma and evidence of malignancy, CT scans revealed rib fractures. To our knowledge, there are no reports of fractures in patients with CVID. This patient presented with hyperparathyroidism, marked hypophosphatemia, hypocalcemia, and vitamin D deficiency. The deficiency of vitamin D further exacerbated the malabsorption of calcium and phosphorus. A decrease in serum calcium levels may stimulate the secretion of parathyroid hormone, resulting in increased bone turnover, bone loss, mineralization defects, and an elevated risk of fractures [6]. Hyperparathyroidism can further aggravate hypophosphatemia. Hypophosphatemia and vitamin D deficiency can both lead to osteomalacia [7, 8], which commonly manifests with fatigue, bone pain, and fractures. This patient’s bone pain and fractures were most likely caused by osteomalacia, secondary to vitamin D deficiency and hypophosphatemia, which were attributed to refractory diarrhea. Following supplementation with vitamin D, calcium and phosphorus, the patient’s bone pain improved, and levels of parathyroid hormone returned to normal.
In conclusion, it is crucial to conduct immunoglobulin testing to screen for CVID in patients with unexplained chronic diarrhea. In patients with refractory diarrhea, it is important to maintain calcium and phosphate balance and ensure adequate vitamin D supplementation to prevent the development of osteomalacia. Early diagnosis and intervention may significantly improve patient outcomes and overall prognosis.