Miscarriage is the most commonly occurring failure of procreation [1]. In Polish hospitals, 40,000 to 45,000 miscarriages occur annually [2]. They occur with the highest frequency in the first trimester of pregnancy [1].
In Poland, the criteria defining miscarriage refer to both the duration of pregnancy and the weight of the fetus [1]. The time indicator defines a miscarriage as an obstetric failure occurring before the completion of the 22nd week of pregnancy (from the 23rd week onwards, it is referred to as a preterm birth and/or stillbirth). The weight criterion defines a miscarriage as the expulsion of the fetus below 500 g of body weight [1, 2].
After a miscarriage, women may experience depressive and anxiety disorders [3]. Data from worldwide literature show that rates of depression in women after experiencing miscarriage reach up to 55%, anxiety and stress range from 28% to 45% [4], and prevalence of post-traumatic stress disorder (PTSD) is up to 39% from 1 to 3 months [5].
Positive feelings, e.g. a sense of hope, are less obvious after miscarriage. It has been reported that a higher level of hope is associated with a lower level of anxiety and depression and a higher quality of life in patients with cancer [6]. Hope is therefore defined as a fundamentally positive phenomenon necessary for constructive coping with the trauma, and its main purpose is to avoid despair, with a secondary function allowing an individual to survive unpleasant or stressful situations.
The aim of the study was to determine the sense of basic hope, as well as the severity level of anxiety and depression symptoms in women after experiencing a miscarriage during hospitalization and 3 months after its conclusion.
Methods. The Bioethics Committee of the Jan Kochanowski University approved the study (25/2020). The study was of two-stage structure. The first stage of the study took place on day 2 or 3 of hospitalization (the surveys were administered by pen and paper), and the second 3 months after its completion. The questionnaires were sent to the same patients from the first stage of the study electronically or by letter. The analysis of the returned questionnaires in the second stage of the study was carried out in accordance with the standards proposed by the American Association for Public Opinion Research (AAPOR) [7]. The research was conducted at the Department of Obstetrics and Gynaecology of the Provincial Combined Hospital in Kielce among in-patients due to miscarriage in the period from September 2019 to August 2021. According to the national procedure every woman referred to the gynaecology department with a diagnosis of missed abortion is hospitalized. After induction of miscarriage, if the endometrial thickness is < 15 mm visible on ultrasound, hospitalization is completed.
The inclusion of the subjects included the following inclusion and exclusion criteria: Inclusion criteria included: patients hospitalized due to miscarriage, the absence of traumatic events within 1 month before hospitalization as a result of miscarriage, returning completed questionnaires 3 months after the end of hospitalization, age over 18 years, consent to participate in the study. Exclusion criteria included patients hospitalized for reasons other than miscarriage, experiencing a traumatic event within 1 month before hospitalization as a result of miscarriage, failure to fill in questionnaires again 3 months after the end of hospitalization, a psychological dysfunction that prevents a history of examination or diagnosis of a mental illness (e.g., depression, anxiety disorder, abnormality of content and manner of thinking), intellectual disability, being under 18 years of age, lack of consent for participation in the study.
An original survey was used to collect sociometric data. The questionnaire contained 13 questions, for example about age, marital status, number of previous miscarriages, having children or week of lost pregnancy.
The Hospital Anxiety and Depression Scale (HADS) by R.P. Snaith and A.S. Zigmond [8] – in the Polish adaptation prepared by M. Majkowicz, K. de Walden-Gałuszko and G. Chojnacka-Szawłowska [9] – was used to assess the level of anxiety and depressive symptoms. Two independent subscales, each containing seven statements, refer separately to anxiety and depression, and for each of the statements the respondent may score from 0 to 3 points. According to the authors of the scale, the following standards of the analysis were adopted: 0–7 points – no symptoms of anxiety or depression; 8–10 points – borderline states; above 10 points – high severity of anxiety and depression symptoms. The maximum score for anxiety and depression separately is 21 points. The higher the score, the greater the incidence of anxiety and depressive symptoms.
The BHI-12 Questionnaire by Trzebiński and Zięba was used to assess the sense of basic hope [10]. According to the authors, hope is understood as a belief of an individual about the order and meaningfulness of the world and its favourable attitude to people. The maximum score on the scale is 45 points. The higher it is, the greater is basic hope.
Statistical analysis. Quantitative variables were analysed by calculating the mean, standard deviation, median and quartiles. The analysis of the qualitative variables was conducted by calculating the number and percentage share of the occurrences of each value. A comparison of the values of quantitative variables in two repeated surveys was made using the Wilcoxon matched-pairs test. The correlations between quantitative variables were analysed using the Spearman rank correlation coefficient. A comparison of the values of quantitative variables in two groups was made using the Mann-Whitney test. A comparison of the values of quantitative variables in three or more groups was made using the Kruskal-Wallis test. Once statistically significant differences had been detected, a post-hoc Dunn’s test analysis was conducted in order to identify groups that differ statistically significantly. A multifactorial analysis of the impact of many variables on the quantitative variable was performed using the linear regression method. The results were presented as regression model parameter values with a 95 percent confidence interval.
The analysis was performed in R program, version 4.1.2 [11].
Results. Finally, 161 patients hospitalized due to miscarriage were included in the study. The return rate on sent questionnaire was 77.8%.
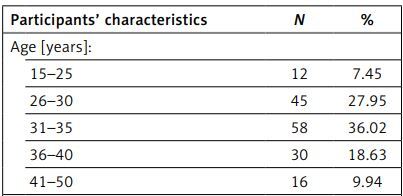
Table I shows the characteristics of the surveyed group. Most of them were women aged 31 to 35, married, and reported pregnancy planning. The length of procreative efforts for the last lost pregnancy (if it was planned) was on average 14.62 months (SD = 25.02) and ranged from 1 month to 15 years (180 months). The week of pregnancy loss ranged from 6 to 21.
Table I
Participants’ characteristics
Table II shows the severity of anxiety and depression symptoms during hospitalization and 3 months after its completion. The severity of anxiety and depression symptoms significantly decreased after 3 months compared to the level during the stay in hospital (p < 0.001).
Table II
Symptoms of anxiety and depression during hospitalization and 3 months after hospitalization
It was found that during hospitalization, most women presented a low sense of hope. After its completion, the largest part of the group declared a high level of a sense of hope. The level of hope significantly increased after 3 months compared to the level during hospitalization (Table III).
Table III
Basic hope during hospitalization and 3 months after hospitalization – significance of changes
| BHI-12 [points] | During hospitalization | After 3 months | P-value |
|---|---|---|---|
| Mean ± SD | 27.79 ±7 | 29.17 ±6.37 | < 0.001 |
| Median | 28 | 29 | |
| Quartiles | 23–33 | 25–35 |
The level of hope during the stay (p = 0.024) and after 3 months (p = 0.028) was significantly lower for married women than for women in informal relationships and unmarried ones. The level was higher for women with primary, technical or vocational education than for those with secondary or higher education (p = 0.01). After 3 months, it was significantly greater in women with primary, technical, vocational, or higher education than in women with secondary education (p = 0.011). A greater sense of hope during the hospital stay (p = 0.023) and after its completion (p = 0.008) was also experienced by professionally active women. The level of hope during the hospital stay (p = 0.03) and after 3 months (p = 0.013) was significantly higher in women who had lost an unplanned pregnancy and had not received treatment at the Procreative Health Clinic (p < 0.001). The number of previous pregnancies lost correlated significantly and negatively with BHI-12 during hospitalization (r = –0.306; p < 0.001) and after 3 months (r = –0.376; p < 0.001). There was also a significant and positive relationship with regard to having children. The more children the respondents had, the higher was their level of the basic sense of hope during their hospital stay (r = 0.212; p = 0.007) and after 3 months (r = 0.214; p = 0.006). The longer the reproductive efforts to become pregnant were, the lower was the level of basic hope both during the stay (r = –0.25; p = 0.001) and after 3 months (r = –0.312; p < 0.001).
There was no correlation between age, place of residence, manner of residence, the week of pregnancy loss, or duration of the current relationship and the level of hope.
The BHI-12 correlated significantly and negatively with the level of anxiety (r = –0.438, p < 0.001) and depression symptoms (r = –0.456, p < 0.001) during and after hospitalization (anxiety r = –0.649, p < 0.001; depression r = –0.643, p < 0.001).
Regression analysis demonstrated that during hospitalization, the independent predictors of the level of the sense of basic hope were: secondary and higher education, lack of professional activity and the number of children. In contrast, secondary education and lack of professional activity were independent predictors of the level of hope after hospitalization. It was hypothesized that an increase in the level of the sense of basic hope may impact an increase in the symptoms of anxiety and depression after hospitalization. In order to evaluate the above relationships, correlations were assessed between the changes detected through the BHI-12 questionnaire and the changes detected through HADS. It was noted that an increase in the level of basic hope (BHI-12) correlated significantly (p < 0.05) and positively (r < 0) with a decrease in the level of anxiety and depression symptoms (Table IV).
Table IV
Basic hope and symptoms of anxiety and depression and sociometric data – linear regression
Discussion. It was found that the level of hope significantly increased after 3 months compared to this level during hospitalization. Hope was associated with lower levels of anxiety and depression symptoms.
An explanation of these results can be found in the concept of post-traumatic growth, according to which a difficult, traumatic experience may significantly affect the perception of the world, its predictability, and the source of new opportunities [10, 12]. A sense of hope was found to be lower in married women than in women who were not in a relationship and/or who were in an informal relationship. From a psychological point of view, it seems that marriage can, or at least should, be a potentially protective factor. However, there exist two possible explanations for this result. First of all, women who are in a formal relationship, but after unsuccessful procreation, lose hope of expanding their family and giving birth to a child with a vital partner. Secondly, the causes of adverse reactions in women after a miscarriage may be associated not only with psychological but also cultural causes.
Therefore, it is not surprising that in this study, low levels of hope were found in childless women. It was noted that the more children the surveyed women had, the higher was their level of hope during and after their hospital stay. Factors such as the number of previous pregnancies lost (the more miscarriages in the past, the lower the level of hope immediately after this event and 3 months after it) and treatment at the Procreative Health Centre also appeared to be important.
Infertility, which is constantly increasing, negatively affects couples’ lives and may cause a crisis [13]. Depression, anxiety [14, 15], and lack of hope [16] were observed to be common among women receiving infertility treatment. Symptoms of depression in women treated for infertility were also associated with lower rates of conception. Conversely, the lower the symptoms of depression and anxiety were, the greater was the increase in successful attempts at procreation [17]. It was also noted that most women treated for infertility had a low level of hope of having children in the future [14, 18]. This is consistent with the results obtained in this study. The regression analysis demonstrated that having each consecutive child is a factor raising the level of hope. Therefore, the lack of children may generate a risk of increasing symptoms of depression and anxiety.
An important aspect of this issue seems to be the relationship of depression and anxiety with the level of the sense of basic hope. It was reported that basic hope was negatively associated with depression [10]. These results are also confirmed by the present data. It was noted that the higher the level of hope was, the lower was the severity of anxiety and depression symptoms both during hospitalization and 3 months after its completion. And conversely, as the level of hope rose, the symptoms of anxiety and depression diminished.
A significant relation was also found between a sense of hope and pregnancy planning and the duration of efforts made for a lost pregnancy. This is consistent with other authors’ findings. The lowest score for feeling hopeful was found in women who had been treated for infertility for up to 4 years and had waited between 7 and 9 years to have a child [18]. Along with the prolongation of procreation time, anxiety and depressive symptoms also increased [14].
A relationship between education and employment and the level of basic hope was also noted. The level of hope after 3 months was significantly higher for women with primary, technical, vocational or higher education than for women with secondary school qualifications and the professionally active group. The regression analysis also demonstrated that the sense of basic hope decreased along with the lack of professional activity. Working women have greater financial freedom, which allows them to access health care services and respond to pregnancy failures more effectively, pay for medical costs or even seek additional support, such as psychological help. Some authors even assume that women who are traditional housewives are more likely to be subject to the traditional expectations of having a child by the family and social environment than other women [19]. For this reason, they have a lower ability to cope with pregnancy loss and social pressure and present higher rates of hopelessness and anxiety as well as depression symptoms [14, 16].
A miscarriage may also play a role in experiencing the next pregnancy. The anxiety and fears related to the progress of their pregnancy, a vision of another loss and receiving (potential) bad news, an ambivalent attitude to a new pregnancy, as well as a negative impact on the child resulting from the mother’s emotional instability and establishing a bond with her consecutive child are the reactions most commonly reported by women [19]. It is also supported by the findings of this study, which indicate that the more early miscarriages occur, the lower is the level of hope.
In the studies related to the assessment of the severity of anxiety and depression symptoms after miscarriage, the personal significance attached to pregnancy was also found to be crucial [20]. It is also supported by the findings of this study. There was no confirmation of an association between the level of adequate protection and the week of pregnancy loss. Thus, regardless of when the pregnancy terminated, at an earlier or later stage, this situation constitutes a kind of specific crisis; it is a unique and individual experience. Parents lost their hopes, dreams and expectations related to the future changes in the family structure. Only a few studies on gestational age and bereavement after miscarriage have demonstrated that the intensity of bereavement increases with the gestational age [21]. Consequently, it is worth noting that although in the medical sense it is a relatively natural process, in the subjective sense it is always personal and may occur at any time, regardless of the physiological course of the pregnancy and the time when it was lost.
People who have experienced a miscarriage are, therefore, a group that requires special attention. Jacobs and Harvey [21] presented a support programme for women who have lost their pregnancies due to miscarriage. An equally effective type of support is a therapy aimed at inspiring hope [22]. Hope-oriented therapy provides a variety of coping options and leads to psychological comfort by enhancing achievements, self-esteem, and effectiveness. It was demonstrated that reviving the feeling of basic hope helps women cope with loss and enhances the willingness to regain confidence in both the help offered and in themselves when facing new challenges (creating a new order in life and giving it meaning) [19].
Although the number of analyses of the psychological consequences of miscarriage has increased worldwide, there is no reference therein to the level of hope and its relationship with the severity of anxiety and depression symptoms. The literature on Polish women does not offer much in this area either. This work is the first to develop this direction of research in Poland.
The present study has several limitations. First of all, the sample of the surveyed women was selected in only one clinical unit. In addition, the obtained data were not analysed in a broader temporal perspective. Not taking into account the issue of the sense of coherence in coping with a crisis situation may also be a crucial factor.
The strength of this study undoubtedly lies in its objective. In the currently available literature, there are no studies analysing the level of basic hope among women who have experienced miscarriage. Understanding how women function in this situation should become a valuable guide in therapeutic proceedings. Despite its extensiveness, the conducted research, however, does not fully exhaust the issue of the psychological aspects of women after experiencing miscarriage. Therefore, conducting further verification in this area is justified.