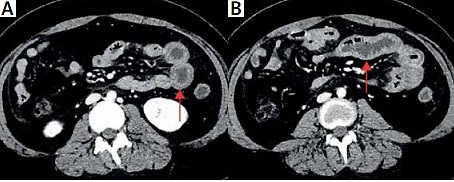
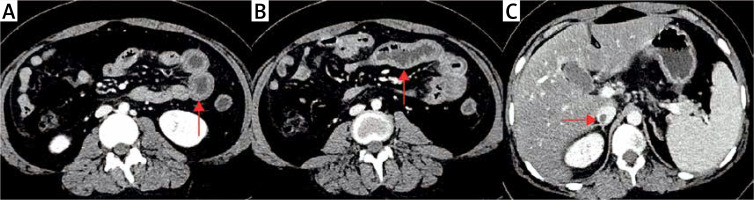
A 14-year-old girl presented to our hospital with acute abdominal pain and vomiting for 2 days. A diagnosis of systemic lupus erythematosus (SLE) as well as secondary Evans syndrome, due to a combination of autoimmune haemolytic anaemia and immune thrombocytopaenia, was made at our hospital 6 months ago – a diagnosis predicated on the simultaneous exclusion of sepsis, paroxysmal nocturnal haemoglobinuria, thrombotic thrombocytopaenic purpura, and Kasabach-Merritt syndrome. Her condition improved after treatment with prednisone (60 mg/day) and mycophenolate mofetil (0.75 g/day). No significant family history was present. Physical examination revealed jaundice and periumbilical tenderness with no rebound pain. Laboratory data showed a white blood cell of 9.78 × 109/l (normal range: 4–10), haemoglobin of 132 g/l (normal range: 110–155), platelets of 131 × 109/l (normal range: 100–300), erythrocyte sedimentation rate of 37 mm/h (normal range: 0–15), C-reactive protein of 4.8 mg/l (normal range: 0–10), PCT of 0.17 μg/ml (normal range: 0–0.5), C3 of 0.78 g/l (normal range: 0.9–1.8), and C4 of 0.03 g/l (normal range: 0.1–0.4). The stool culture was negative. Positive for antinuclear antibodies (ANA), direct and indirect Coombs test. There were elevated titres of anti-cardiolipin and anti-β2-glycoprotein-I (β2-GPI) antibodies of IgM and IgG isotypes, along with the presence of lupus anticoagulants. The systemic lupus erythematosus disease activity index (SLEDAI) score was greater than 10. Enhanced abdominal computed tomography showed diffuse intestinal wall thickening, engorgement of mesenteric vessels (Figures 1 A, B), and inferior vena cava thrombosis (Figure 1 C), with no evidence of intestinal infection or tumour. The final diagnosis of lupus mesenteric vasculitis, secondary antiphospholipid syndrome (APS), and inferior vena cava thrombosis was made. Initially, she was given 1 mg/kg of methylprednisolone as the first choice of treatment, but her symptoms did not resolve. Subsequently, methylprednisolone 500 mg/day was given for 3 days and then gradually reduced to 0.5 mg/kg for maintenance, combined with cyclophosphamide 0.6 g to enhance immunosuppression and enoxaparin 4000 U/day for anticoagulation, along with fasting, anti-infection, parenteral nutrition, and other symptomatic supportive treatment. She recovered well and was discharged 2 weeks later with regular follow-up.
Figure 1
A, B – Enhanced abdominal computed tomography showed diffuse intestinal wall thickening and engorgement of mesenteric vessels. C – Enhanced abdominal computed tomography showed a large thrombus in the inferior vena cava
The serological examination of gastrointestinal tract involvement in SLE lacks specific markers, and its clinical manifestations are not specific, especially requiring differentiation from gastrointestinal tract infection, inflammatory bowel disease, pseudo-intestinal obstruction, adverse drug reactions, and other diseases [1]. Abdominal contrast-enhanced CT is helpful for early diagnosis, and the common imaging findings are target sign (thickening and oedema of the intestinal wall) and engorgement of mesenteric vessels. Buck et al. found that the incidence of mesenteric vasculitis was significantly higher in patients with SLEDAI scores above 8 than in those with scores below 8. Therefore, computed tomography is recommended as a routine for the diagnosis of vasculitis in patients with SLEDAI scores above 8 and subacute abdominal pain [2]. The inflammatory mechanism represented by intestinal vasculitis and the intestinal vascular thrombotic mechanisms induced by antiphospholipid antibodies may activate each other and participate in the development of gastrointestinal involvement and inferior vena cava thrombosis in this case of SLE [3]. Studies have shown that β2-GPI inhibits ADP-induced platelet aggregation and activation of coagulation factors and is thought to control thrombus formation [4]. Vein thrombosis in APS occurs mostly in the veins of the extremities and pulmonary system, while obstruction in the portal, mesenteric, and inferior vena cava is rare. The present case is an uncommon example of combined mesenteric vasculitis and inferior vena cava thrombosis associated with APS. Treatment usually requires long-term anticoagulant therapy. In conclusion, lupus mesenteric vasculitis is the most common cause of acute abdominal pain in childhood-onset SLE, and it usually occurs during the active phase of the disease, with the possibility of combined inferior vena cava thrombosis requiring vigilance.