According to the classification of the International Headache Society [1], cervicogenic headache (CGH) belongs to the group of secondary disorders and is attributed to dysfunctions of the soft tissues and nerve tissue of the cervical spine. CGH constitutes a major diagnostic and therapeutic challenge. It may be caused by overload lesions, often as a consequence of injuries but without traumatic spinal lesions. The headache is mainly of medium intensity, non-pulsating, of variable duration, or constant. It is usually located on the forehead, temples, or in the occipital area and is accompanied by nausea and dizziness. Head movements, forced position, and the compression of characteristic areas may aggravate the pain. Limited mobility of the cervical vertebrae is commonly observed. Suitable treatment should include an accurate diagnosis of dysfunctions in the area of cervical structures and establishing their association with headaches. Differential diagnosis should be carried out to exclude life-threatening conditions. In addition to pharmacological treatment, it seems justified to include physiotherapy in the therapeutic process. It requires a great deal of experience from the physiotherapist cooperating with a neurologist, both in determining the dysfunctions of the entire head-neck-shoulder complex, and in the selection of effective rehabilitation techniques [2–4].
A 19-year-old woman presented to the Emergency Department (ED) due to increasing headache, persistent nausea without vomiting, dizziness, and periodic nasal discharge. The symptoms were preceded by a whiplash injury. The patient remembered taking part in the collision and what happened next. The ED physician found no meningeal or focal symptoms. Laryngological and surgical consultation and imaging tests were ordered. Physical examination revealed slight epistaxis and swelling of the nasal conchae. The X-ray of the cervical spine showed the loss of lordosis without other lesions with no traumatic changes in the craniocervical joint. At discharge from the ED, the patient was recommended to use Sulfarinol intranasally, Aescin and ibuprofen orally.
Due to the lack of improvement, i.e., the headache and dizziness lasted, the patient was consulted by a neurosurgeon 3 days following the event and underwent an outpatient MRI of the brain in the FRAIL, SWI, DWI, FRWSE sequences in the frontal, sagittal and transverse planes with no significant changes. On the following days, an MRI examination of the cervical spine was also performed in the FRFSE and MERGE sequences. It showed: a slight kyphotic position of the C5-C6 level and a small medial hernia of the intervertebral disc, lateralizing to the left and compressing the meningeal sac. A zone of the increased signal was visible in the posterior part of the disc, indicating a fibrous ring rupture. In addition, a small left-sided distal disc protrusion, compressing the meningeal sac and discreetly narrowing the intervertebral foramen, was present at the C6-C7 level. The visible changes were not recent. They do not cause complaints reported by the woman. The spinal cord image was normal without significant focal lesions. In addition, a CT scan of the head was performed, in which no significant abnormalities were found.
Having the results of the imaging examinations, the patient with severe head and neck pain at the time consulted another neurosurgeon. The physician found a slight limitation of the mobility of the cervical spine and compressive tenderness of the spinal processes of the neck. The patient was recommended to use Nimesil orally. After 5 days, the patient presented for another, independent neurosurgical consultation. Comprehensive rehabilitation of the cervical spine was proposed, with the continuation of home-based rehabilitation, immobilization in a soft Schantz-type orthopedic collar, and symptomatic treatment for 3 weeks was suggested.
The patient was examined by a physiotherapist. The diagnosis was made for complaints resulting from dysfunctions of the soft tissues and nerve tissue of the cervical vertebrae. The history and functional examination showed: the limitation of active and passive mobility and compressive tenderness of the spinous processes (Figure 1) of the cervical spine, loss of the cervical lordosis, weakening of the cervical spine muscles, pain during active movement in the shoulder and neck joints (observations based on provocative tests) as well as the presence of active trigger points in the area of the quadrilateral, suboccipital and sternocleidomastoid muscles. Due to persistent, paroxysmal dizziness, a the Dix-Hallpike maneuver [5] was made for benign paroxysmal positional vertigo (BPPV). Horizontal-torsional left-beating nystagmus was observed, which confirmed otolithic disturbances in the posterior semicircular canal of the right labyrinth. The Epley repositioning maneuver [6] was performed, leading to an improvement in terms of dizziness. Moreover, the patient experienced kinesiophobia manifesting as the fear of removing the orthopedic collar and active head movements. As regards history, the patient paid special attention to persistent headaches excluding her from everyday duties (6/10 on the VAS). After consultation with a neurologist specializing in the treatment of headaches, the patient was subjected to comprehensive physiotherapy, which was conducted in 1-hour therapeutic sessions, every day for the first 4 days followed by a once-weekly regimen for the next 2 months. Trigger point therapy was performed within tense muscles (the upper part of the quadriceps muscle, levator scapulae muscle, suboccipital muscles, as well as pectoral muscles). The patient was lying supine with the spinal curvatures comfortably supported, which ensured comfort during therapy. Moreover, the patient underwent neuromobilization of the dura mater while lying supine and in the seat with the lower limbs supported, mobilization according to the Mulligan concept [3], which included exercises conducted by a therapist, as well as an element of self-therapy based on the Sustained Natural Apophyseal Glides (SNAG) technique recommended in the case of limited rotation in the cervical spine, stretching, exercises strengthening the weakened muscles (neck flexors, lower and middle part of the quadriceps muscle, serratus anterior muscles) and increasing the range of motion within the cervical segment and rehabilitation of the vestibular system with the use of habituation and balance exercises. Instructions for exercises to perform at home (mainly autotherapy of SNAG techniques, autoneuromobilization, corrective exercises of the cervico-shoulder complex, automassage of suboccipital muscles) and recommendations related to preventive measures after the applied repositioning maneuver were provided, i.e., the patient was recommended not to take a critical position for 48 h or lie on the affected side for 7 days after the maneuvers. It was suggested to limit the use of the orthopedic collar to situations in which the patient could be exposed to uncontrolled head movements, e.g., public transport. By the patient’s wishes, the occipital nerve block was abandoned. Physiotherapy was performed concurrently with the pharmacotherapy implemented by a neurologist – from 5 to 20 mg (dose determined depending on the severity of pain) of citalopram taken in the morning.
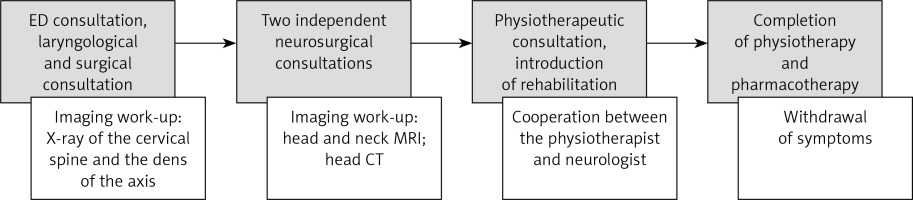
After 4 weeks of treatment, the pain gradually withdrew to the level of 2–3 on the VAS scale, which resulted in reduced drug intake, and restoration of the range of passive and active motion of the cervical spine. The patient stopped reporting the fear of movement, even in situations requiring greater physical involvement. Office-based rehabilitation was continued for another month and was then limited to telephone consultations. Three months after the accident, the patient returned to normal activities, and reported no complaints. The order of visits to individual specialists is shown in Figure 2.
In the opinion of the authors, the described physiotherapeutic methods are the key ways of proceeding. They can be modified or enriched using techniques of other concepts of manual therapy, relaxation training, and psychotherapy. It should always be in accordance with clinical conclusions and the needs of a particular patient.
The present case shows the important role of a physiotherapist in the diagnosis and treatment of cervicogenic headaches and dizziness due to whiplash injury. Despite several consultations with physicians of various specialties, the cooperation of a physiotherapist and a neurologist seemed to be the most effective form of treatment for the described patient. The treatment included comprehensive rehabilitation and pharmacotherapy. Effective systemic mechanisms should be sought to incorporate rehabilitation for patients with headaches and dizziness early in the treatment process.