The lung isolation effect of double-lumen bronchial tubes (DLT) can provide a good surgical field for thoracoscopic surgery, ensure smooth procedure of the operation, ensure effective ventilation of the unaffected lung, and avoid the pollution of the secretion of the affected lung [1]. At present, DLT is still one of the most widely used important means of lung isolation in thoracic anaesthesia. The correct position of DLT directly affects the safety and effectiveness of lung isolation technology. Ensuring the correct position of DLT is a good way to maintain single-lung anaesthesia. On the premise of ventilation and oxygenation, the risk of hypoxaemia, airway damage, and poor lung collapse may occur when the DLT is in the wrong position. Lung auscultation and fibreoptic bronchoscopy (FOB) examination are the most common methods for localizing DLT. The traditional auscultation method has strong subjectivity, high blindness, low accuracy, and poor reliability [2]. The FOB inspection method is the most effective for DLT positioning, but there are certain limitations in the clinical use of FOB in primary hospitals due to its cost. At the same time, in thoracic surgery, the position of the DLT tube end often moves due to the placement position or surgical operation. Because FOB is expensive and cannot be used for continuous monitoring during surgery, it cannot be used to determine DLT displacement early [3].
The level of airway pressure is an important indicator of ventilatory resistance. Therefore, monitoring of airway pressure is often performed during mechanical ventilation. The airway pressure is generally controlled at 15–20 cm H2O during mechanical ventilation, and the airway pressure will increase when the two-lung ventilation (TLV) is changed to one-lung ventilation (OLV). When the TLV was changed to OLV, peak inspiratory pressure (Ppeak) increased by 67% when the DLT position was normal, and it increased by 74% when the DLT position was abnormal [4]. Ppeak is the maximum airway pressure during inhalation, which can reflect the position of the DLT to ensure the correct position of the DLT and the patency of the airway. Ppeak can be maintained at a satisfactory level during OLV. Monitoring Ppeak during OLV can help detect the abnormal position of DLT early, avoid the decrease of oxygen saturation (SPO2) and the occurrence of hypoxaemia, and then adjust the position of DLT, thereby preventing more serious consequences. End-tidal carbon dioxide pressure (PETCO2) refers to the concentration of CO2 in the exhaled breath at the end of the breath [5]. PETCO2 is a non-invasive monitoring method that has become another vital sign monitoring indicator of the human body in addition to blood pressure, ECG, blood oxygen, body temperature, and blood pressure. In recent years, with the rapid development of sensing analysis and other technologies, PETCO2 monitoring has the advantages of being simple, available in real-time, and continuous and having high sensitivity. PETCO2 monitoring has been drawing more and more attention in various types of surgeries, critically ill patient rescue, and intensive care units [6].
At present, there is still a lack of quantitative indicators for judging the increase in airway pressure when the DLT is in the correct or in a misplaced position. This study was carried out to explore the feasibility of accurately locating the position of the DLT tube end through Ppeak combined with PETCO2 monitoring. We assume that Ppeak and PETCO2 can effectively predict the location of DLT, and that Ppeak and PETCO2 in one-lung ventilation are higher than those in two-lung ventilation. The aim is to improve the accuracy of DLT tube end positioning and ensure the continuous and smooth progress of thoracic surgery without the aid of FOB positioning.
Before the operation, the Ethics Committee of our hospital gave consent and the patients and their families agreed and signed an informed consent form for anaesthesia. Sixty patients, aged 18–65 years, who needed thoracotomy under elective general anaesthesia, were randomly selected, with no history of bronchial asthma or airway hyperresponsiveness, and with cardiac function grade I–II. The patients were routinely fasted for 8 h and avoided drinking for 2 h before the operation. After entering the room, the venous access was routinely opened. Anaesthesia induction in patients was the same: midazolam 0.05 mg/kg, sufentanil 0.5 µg/kg, propofol 1.0–2.0 mg/kg, and rocuronium 0.6 mg/kg [7, 8]. After 3 min, an appropriate type of DLT was selected, and the anaesthesia intubation operation was performed by an anaesthesiologist with the same amount of experience. In the experiment, intermittent positive pressure ventilation, tidal volume 8 ml/kg, frequency 12 times/min, inspiratory ratio 1 : 2, maintained PETCO2 35–40 mm Hg, inhaled 1.5–2.0% sevoflurane during the operation, and pumped remifentanil and propofol were used to maintain an anaesthesia depth BIS of between 45 and 60 [9–11].
Monitoring of PETCO2 and Ppeak. After induction, DLT was inserted, and the catheter position was adjusted until the auscultation was satisfactory, and the PETCO2, Ppeak, and SPO2 values of TLV and OLV were recorded. After turning over, the catheter position was adjusted and the auscultation was satisfactory, and the PETCO2, Ppeak, and SPO2 values were recordeds after re-examination with FOB. Displacement of the catheter was defined as movement of the DLT by ≥ 5 mm from the correct position.
DLT positioning criteria. Judgment standard of auscultation: during TLV auscultation, the breath sounds of both lungs were the same as before intubation; during OLV auscultation, the breath sounds of each lobe on the ventilation side were the same as before intubation, but the breath sounds on the non-ventilation side disappeared.
Criteria for FOB judgment: the positioning of the left DLT, the FOB is placed in the left tube, the left bronchus and the bronchial opening of the upper and lower lobes can be seen at the exit end of the tube, and the FOB is placed in the right tube, and the carina, the opening of the right bronchus and the left bronchus can be seen at the mouth of the tube. The inflated blue bladder is below the carina. The right DLT was positioned, and the FOB was inserted into the left tube. The carina, the left bronchial opening, and the inflated balloon in the right bronchus were visible at the tube orifice. The FOB was inserted into the right tube. The bronchial orifice of the right lower lobe, the bronchial opening of the right upper lobe can be seen through the lateral hole of the duct.
PETCO2 criterion: TLV, the PETCO2 curve, and its values were normal. During OLV, the PETCO2 curve and its value on the ventilating side were normal, and the PETCO2 curve on the non-ventilating side was a straight line, and its value was 0. Meeting this standard was considered satisfactory positioning. If there is a PETCO2 curve on the non-ventilation side but there is no expiratory plateau, the PETCO2 value is lower than normal, indicating that some lung isolation is incomplete; if the non-ventilation side CO2 curve shows an expiratory plateau, the PETCO2 value is in the normal range, indicating severe lung isolation.
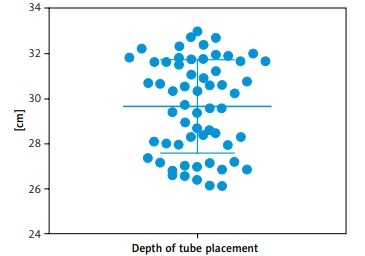
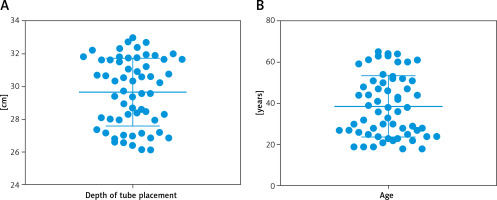
General condition and depth of DLT insertion in patients. There were 60 patients, including 27 patients with left DLT and 33 patients with right DLT. DLT was successfully inserted in all patients at one time, and 8 cases were in place after repeated adjustment under auscultation. The mean intubation depth of the patients was 29.66 ±0.27 cm, and the mean age was 38.62 ±1.90 years (Figure 1). When the lung isolation effect of the supine auscultation method was satisfactory, PETCO2 monitoring showed that the lung isolation was incomplete in 16 cases. After FOB re-examination, 22 cases had improper position, of which 10 cases were inserted too deep, 8 cases were too shallow, and 4 cases had catheter distortion. The position of DLT changed in 9 cases by auscultation after turning over. The position of the catheter was adjusted until the lung isolation was satisfactory, and PETCO2 was monitored. The lung isolation was incomplete in 9 cases, and shifted by FOB in 15 cases, of which 9 cases were too shallow and 6 cases were too deep.
Figure 1
Statistics of mean intubation depth (A) and mean age (B) of patients. A total of 60 patients, aged 18–65 years were involved in this test
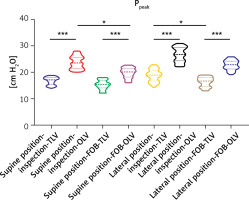
Changes in Ppeak during TLV and OLV. The OLV Ppeak in the supine and lateral positions of the two detection methods was significantly higher than that of the TLV (p < 0.05). The Ppeak detected by the FOB method in the supine and lateral positions was lower than that by the auscultation method, respectively (p < 0.05). During OLV, 21 cases had Ppeak below 25 cmH2O (1 cm H2O = 0.0981 kPa), 32 had Ppeak at 25–30 cm H2O, and 7 had Ppeak at 30–35 cm H2O. After FOB re-examination, there were 5 cases with Ppeak at 25–30 cm H2O, and 55 cases with Ppeak < 25 cm H2O (Figure 2, Table I).
Table I
Ppeak (cm H2O) test results and results statistics of patients
| Ppeak | Supine position | Lateral position | ||||||
|---|---|---|---|---|---|---|---|---|
| Inspection | FOB | Inspection | FOB | |||||
| TLV | OLV | TLV | OLV | TLV | OLV | TLV | OLV | |
| Mean | 16.72 | 23.74 | 15.26 | 19.74 | 18.72 | 26.60 | 16.35 | 22.71 |
| SEM | 0.18 | 0.31 | 0.22 | 0.25 | 0.30 | 0.36 | 0.24 | 0.23 |
Figure 2
The patient’s Ppeak test results. Detect the Ppeak of the above 8 groups (Supine position-inspection-TLV, Supine position-inspection-OLV, Supine position-FOB-TLV, Supine position-FOB-OLV, Lateral position-inspection-TLV, Lateral position-inspection-OLV, Lateral position-FOB-TLV, and Lateral position-FOB-OLV). *P < 0.05, ***P < 0.001
Changes in PETCO2 during TLV and OLV. The PETCO2 numerical monitoring results showed that in each group, the PETCO2 of OLV was higher than that of TLV. During TLV, the change of PETCO2 between auscultation method and FOB was not significant (p < 0.05), while during OLV, the change of PETCO2 in the supine position was not obvious, and PETCO2 in the lateral position was significantly decreased after FOB review (p < 0.05) (Figure 3 A, Table II).
Table II
PETCO2 (mm Hg) and SPO2 test results and results statistics of patients
Figure 3
A – PETCO2 test results of patients. Detect the PETCO2 of the above 8 groups (Supine position-inspection-TLV, Supine position-inspection-OLV, Supine position-FOB-TLV, Supine position-FOB-OLV, Lateral position-inspection-TLV, Lateral position-inspection-OLV, Lateral position-FOB-TLV, and Lateral position-FOB-OLV). B – SPO2 test results of patients. Detect the SPO2 of the above 8 groups. (Supine position-inspection-TLV, Supine position-inspection-OLV, Supine position-FOB-TLV, Supine position-FOB-OLV, Lateral position-inspection-TLV, Lateral position-inspection-OLV, Lateral position-FOB-TLV, and Lateral position-FOB-OLV). *P < 0.05, ***P < 0.001, ns – not significant
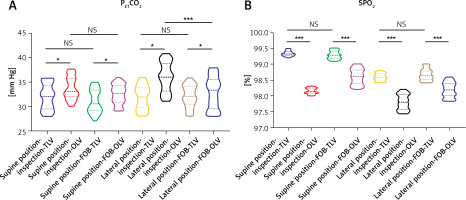
Changes in SPO2 during TLV and OLV. Comparing FOB and auscultation, the content of SPO2 in OLV was significantly lower than that in TLV (p < 0.05). After re-examination of FOB in supine and lateral positions, there was no significant difference in SPO2 between TLV and auscultation, but the SPO2 of OLV was significantly increased (p < 0.05) (Figure 3 B, Table II).
The correct position of the DLT can ensure the effective implementation of the lung isolation technology in thoracic surgery. When the DLT is in the wrong position, there may be risks such as hypoxaemia, airway damage, and poor lung collapse. FOB examination is the most effective method for DLT positioning at present, but the clinical use of FOB in primary hospitals has certain limitations, and FOB examination cannot be used for continuous monitoring during surgery [12, 13]. Therefore, this study analysed the application of Ppeak combined with PETCO2 monitoring in DLT localization.
For the DLT in the best position, the safe margin of movement is 16–19 mm for the left DLT and only 1–9 mm for the right DLT. Some studies believe that monitoring PETCO2 can more accurately judge the position of tracheal intubation and shorten the judgment time. During OLV, if there is air leakage from the ventilated side to the non-ventilated side, the PETCO2 curve and its value on the non-ventilated side can reflect the amount of leaked gas and the number of ventilations, i.e. it can reflect the DLT alignment and incomplete lung isolation [14–16]. In this study, when the lung isolation effect of the supine auscultation method was satisfactory, PETCO2 monitoring showed that the lung isolation was incomplete in 16 cases. The position of DLT was changed in 9 cases by auscultation after turning over, and the position of the catheter was adjusted until the lung isolation was satisfactory, and PETCO2 was monitored, and the lung isolation was incomplete in 9 cases. This study shows that monitoring PETCO2 has significantly greater accuracy than auscultation in detecting incomplete lung isolation. Because the PETCO2 on the non-ventilated side is monitored, regardless of the position of the bronchial balloon (the depth of the DLT catheter), and as long as the side bronchus can be blocked, the PETCO2 cannot be monitored, but when the DLT is in the correct position, if the bronchial balloon fails to completely block the side bronchus, some airflow leaks into the non-ventilated side. The PETCO2 waveform can be measured on the non-ventilated side.
The level of airway pressure is an important indicator to reflect ventilation resistance. The airway pressure is generally 15–20 cm H20 during TLV. When changing from TLV to OLV, the airway pressure will increase by 40% with the reduction of the effective lung ventilation area [17, 18]. The plateau pressure is the airway pressure at the end of inspiration, which overcomes the elastic pressure of the chest and lungs and keeps the lungs in a state of expansion. Ppeak is the highest airway pressure when the lung is inflated. When it remains constant and the airway is unobstructed, the level of Ppeak can accurately reflect the degree of airway obstruction, i.e. the level of Ppeak is closely related to whether the DLV is in place. When the DLT is inserted too deeply and the left/right upper lobe bronchus is blocked, the left/right lung ventilation bronchus is reduced and the airway resistance is increased. The Ppeak of OLV in the supine and lateral positions of the 2 detection methods was significantly higher than that of the TLV. The Ppeak detected by the FOB method in the supine and lateral positions was lower than that by the auscultation method [19, 20]. In each group, the PETCO2 of OLV was higher than that of TLV. During TLV, the change of PETCO2 between auscultation method and FOB was not obvious, but during OLV, the change of PETCO2 in the supine position was not obvious, and the PETCO2 in the lateral position was significantly decreased after FOB review. Compared with the auscultation method, the SPO2 content of FOB in OLV was significantly lower than that in TLV. After the FOB review after the supine and lateral positions, there was no significant difference in SPO2 between TLV and auscultation, but the SPO2 of the OLV increased significantly.
Because the monitoring of Ppeak and PETCO2 is continuous, slight changes in DLT during surgery can be detected in time, and its clinical placement rate is higher than that of auscultation. The use of Ppeak and PETCO2 to evaluate the catheterization site of patients not only reduces the trauma of the clinical procedure, but also enables the clinician to dynamically monitor the changes of the patient’s condition, which is critical for emergency treatment. Therefore, monitoring with Ppeak and PETCO2 is a quick and easy way to improve DLT in place. The improvement of DLT positioning accuracy is conducive to the smooth progress of thoracic surgery, ensuring the safety of patients during surgery and rapid postoperative recovery, reducing the length of hospitalization, and reducing hospitalization costs. In this study, through the relationship between Ppeak and PETCO2 monitoring and DLT tube end position, a simple, easy, accurate, and clinically practical DLT localization method was created. This method can be extended to grass-roots hospitals without FOB or with limited FOB, which is beneficial to the development of relevant departments in grass-roots hospitals. With the promotion of hierarchical diagnosis and treatment, we need to establish more diverse treatment systems and methods, and explore and compare the advantages of different methods to deal with different medical conditions and different patient groups. The limitations of this study are that the sample size is small and the follow-up work cannot be followed up in time. These factors need to be considered in future research.
In conclusion, compared with the auscultation method, the clinical delivery rate of PETCO2 and Ppeak monitoring is higher, and the change of DLT position can be detected in time.