The presence of a foreign body in the upper gastrointestinal tract is a common emergency among digestive system diseases. Most foreign bodies can be spontaneously expelled via the digestive tract, but some will require endoscopic removal; for a small number, surgery will be required [1]. Most foreign bodies in the upper gastrointestinal tract are fish bones, and it is very rare for surgical clips to enter the gastrointestinal tract through the intestinal wall [2]. Laparoscopic cholecystectomy (LC) is the preferred surgical procedure for benign gallbladder diseases, which has the advantages of less trauma and faster postoperative recovery compared with traditional open surgery, but there are some complications, such as incision infection, bile duct injury, stone residue, and surgical clip displacement [3, 4]. We usually use absorbable bioclips to deal with the gallbladder duct and gallbladder artery during LC implementation. Since Hem-o-lok clips are made of a non-absorbable polymer that cannot be absorbed by the body, there is a possibility of clip migration after surgery.
In clinical practice, Hem-o-lok® clip displacement is common in the biliary system, the displacement can lead to bile leakage, bile duct stones, obstructive jaundice, and even acute pancreatitis [5]. Hem-o-lok® clip displacement to the duodenum and cause duodenal foreign body or ulcers is very rare [6–8]. Clinical symptoms of Hem-o-lok® clip displacement to the duodenum are atypical, which are mainly manifested as abdominal pain, digestive bleeding, nausea, vomiting, etc. The diagnosis mainly depends on digestive endoscopy.
A case in which a Hem-o-lok® clip had entered the duodenal bulb wall, which was subsequently endoscopically removed following laparoscopic cholecystectomy, was presented in this report.
A 64-year-old male patient underwent laparoscopic cholecystectomy in hospital in November 2012 due to “cholecystolithiasis with cholecystitis”, which led to an indwelled Hem-o-lok® clip. In November 2020, the patient underwent fiberoptic gastroduodenoscopy in hospital due to “repeated/persistent upper abdominal pain for one week”. The results indicated a duodenal bulb ulcer and a foreign body (a fish bone) embedded in the duodenal bulb (Figure 1 A). Following the discovery of the duodenal ulcer, endoscopic biopsy for HP testing was not conducted. Later, a 13C breath test was conducted to confirm the absence of HP infection. The foreign body was removed under fiberoptic gastroduodenoscopy, and the surgery was successful without postoperative hemorrhage or perforation (Figure 1 B).
Figure 1
A – Foreign body in the duodenum – food residues. B – The foreign body – food residues. C – The location of the Hem-o-Lok® clip by abdominal CT. D – Embedding of the Hem-o-Lok® clip in the duodenum. E – Removal of the ligation clip. F – Review of the duodenal bulb
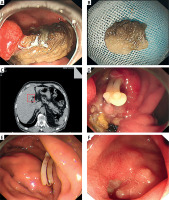
A postoperative abdominal computed tomography (CT) scan showed post-cholecystectomy and a visible Hem-o-lok® clip (Figure 1 C). On June 15, 2022, the patient was admitted to the gastroenterology department of the hospital due to “persistent abdominal pain for 1 month”. Liver function tests performed by the patient at the time showed no abnormalities. Fiberoptic gastroduodenoscopy showed food residues embedded in the duodenal bulb, which were removed using grasping forceps. The large sizes of the food residues initially made them difficult to remove; accordingly, they were crushed using a lithotripter and removed in batches using mesh baskets (The Olympus single use retrieval basket (FG-V422PR)). After repeatedly washing the wound inside the duodenal bulb, an embedded white surgical ligation (Hem-o-lok®) clip was observed (Figure 1 D). The clip was removed using grasping forceps, and no obvious postoperative hemorrhage was observed on the wound surface. Thus, the procedure was considered to have been successful.
Postoperatively, symptomatic treatment, such as fasting (water and food), as well as rehydration, was delivered (Figure 1 E). The abdominal CT scan 6 h after surgery showed no signs of perforation and confirmed that the Hem-o-lok® clip had been successfully removed. The patient was discharged 4 days after surgery. The patient reported neither abdominal pain nor melena at the follow-up 1 month after discharge. A fiber gastroduodenoscopy confirmed that the duodenal ulcer had healed (Figure 1 F).
Foreign bodies in the upper gastrointestinal tract are typically ingested orally, both accidentally and intentionally; however, instances of foreign bodies entering the upper gastrointestinal tract from the abdominal cavity are extremely rare [8]. Foreign bodies in the upper gastrointestinal tract are mainly found in the esophagus, which may be linked to four physiological structures of the esophagus, i.e., the upper esophageal sphincter, the middle of the esophagus, the intersection of the aorta with the left main bronchus, and the lower esophageal sphincter. The insertion of foreign bodies is also associated with esophageal lesions, such as esophageal tumors and hiatal hernia, which may increase the incidence of foreign bodies in the upper gastrointestinal tract [9]. The presence of a foreign body in the upper gastrointestinal tract may lead to mucosal hemorrhage, erosion, ulceration, obstruction, and even perforation, and diabetes mellitus (DM) may increase the risk of these complications [10]. Studies have shown that the longer a foreign body is present, the higher the incidence of ulcers and perforation [11].
The patient in the present case study had a history of DM, no history of Hp infection, and the foreign body had been in the duodenum for at least 1 year. Upon an endoscopy, a large duodenal ulcer was observed.
Endoscopic treatment is both safe and efficient and is the first choice for the removal of foreign bodies in the upper gastrointestinal tract using equipment such as mesh baskets and biopsy forceps [12]. In the present case, the food residues were too large and could not be removed directly. A lithotripter was used to crush the residues and remove them in batches using mesh baskets. Finally, biopsy forceps were used to remove the surgical ligation clip.
Laparoscopic cholecystectomy and common bile duct exploration used to be standard surgical procedures for removing gallbladder stones and the common bile duct. During surgery, a Hem-o-lok® clip is generally used by surgeons to clip the cystic duct and blood vessels. Clip displacement is an extremely rare complication of laparoscopic cholecystectomy; data from 1978 to 2008 reported only 69 cases of clip displacement [13]. Among these, there were only 3 cases of clip displacement in the duodenum after laparoscopic cholecystectomy, one of which involved a clip entering the duodenum during fiberoptic gastroduodenoscopy screening 13 months after surgery. Due to severe adhesions, in this case, the clip had not been removed; upon a fiberoptic gastroduodenoscopy, the clip was found to have been covered by scar tissue following 2 months of proton pump inhibitor therapy [14]. Another case presented with abdominal pain 8 months after surgery. Fiberoptic gastroduodenoscopy showed two Hem-o-lok® clips in the duodenal wall, which were successfully removed using grasping forceps [15]. In the third case, a fiber gastroduodenoscopy was conducted due to melena 1 year after surgery, and a Hem-o-lok® clip was found to have punctured the duodenal wall. The removal of the clip failed on the initial attempt. Three months later, a fiberoptic gastroduodenoscopy showed that the clip had been displaced into the lumen, and it was subsequently removed successfully [16].
The present case, i.e., Hem-o-lok® clip displacement more than 10 years after laparoscopic cholecystectomy, is even rarer. The patient also suffered from coronary heart disease and had been taking aspirin as part of antiplatelet therapy over an extended period, which was not conducive to the healing of peptic ulcers. In addition, when the foreign body was removed 1 year ago, the long-term administration of proton pump inhibitors had failed to heal the peptic ulcer and instead resulted in large-sized food residues embedding. The present authors removed the foreign body, and the prognosis for the present case was satisfactory.
In conclusion, for recurrent duodenal ulcers in clinical practice, rare causes should be considered, including the presence of a foreign body.



