Introduction
Cancer pain is a serious medical problem, as it affects as many as 75% of cancer patients. Moreover, as the disease progresses, the percentage of those suffering from pain increases. Cancer pain is one of the most common symptoms accompanying cancer and the symptom that patients fear the most [1]. The International Association for the Study of Pain (IASP) defines pain as ‘an unpleasant sensory and emotional experience that accompanies or is merely related to existing or impending tissue damage’ [2]. Therefore, pain has two important components: sensory, including nociception and perception of pain, which helps to determine the location of pain, and emotional, related to the patient’s mental reaction to the experienced pain [3]. The emotional component of pain is highly subjective, and therefore the degree of sensitivity to pain sensation varies among patients [4]. Clinically, pain is considered to occur whenever it is reported by the patient and is as severe as the patient judges it. Chronic cancer pain is a specific and multi-level therapeutic problem. It is the result of not only the disease process itself but also the personality and temperamental conditions as well as many psychological, social, and even spiritual factors. Due to its long duration, chronic cancer pain has a negative effect on the patient’s emotional state, often leading to depression, anxiety, insomnia, and physical exhaustion. In the long run, the problem of cancer pain also becomes a social problem, as it begins to affect the family and relatives of the patient, negatively influencing, among other aspects, interpersonal and social relations [5, 6]. It has been proven in many clinical studies that chronic cancer pain contributes to the increase of the patient’s mental discomfort and to the development of anxiety-depressive disorders [5, 7]. The opposite relationship was also confirmed. Chronic cancer pain, if inadequately diagnosed and treated, may overwhelm the patient and affect all spheres of their daily functioning by reducing the quality of life, limiting physical activity, disrupting existing family, professional and social interactions, and causing mental suffering. Strong and chronic pain, as a consequence of the multifaceted impact on the patient, may contribute to a worse course of the neoplastic disease and reduce the chances of remission, as well as the development of suicidal thoughts or requests for euthanasia [8].
The basis of appropriate pain treatment is its proper and thorough diagnosis. The standard diagnosis of cancer pain is based on the diagnosis of the causes and pathophysiology of pain and the assessment of its intensity [9].
Pain is a consequence of the neoplastic disease itself, as well as of the implemented oncological therapies, e.g. chemotherapy or radiotherapy [10]. Pain is most often reported in patients with advanced cancer (64%) and patients undergoing oncological treatment (59%). Approximately 33% of patients in remission require continued therapy because of persistent chronic pain. In Poland, approximately 200,000 cancer patients each year require analgesic treatment. It is estimated that approximately 90,000 patients die of cancer while experiencing pain [11]. This situation is caused by many factors. Often, patients do not report their pain symptoms to doctors for fear of disease progression, which may result in failure to qualify for oncological treatment and to avoid being a troublesome patient. Frequently, doctors do not have time to ask questions about pain during short and cancer-focused visits. In addition to these factors, there is also the fear of opioid drugs, especially as pain in cancer can be severe or very strong and the use of less effective, generally available painkillers is ineffective [12]. A good flow of information between the patient and a member of a healthcare team significantly affects the well-being and subjective assessment of the patient’s health.
Pain, and even the awareness that it may occur, affects a person’s mood and modifies their health behavior, and may change the treatment process. The perception of pain in cancer patients is sometimes so great and long-lasting that it disorganizes the patient’s life, making it impossible for them to function even on a basic level and degenerates the patient’s psyche. Chronic pain is determined somatically, as well as psychologically and socially [13].
The aim of the study was to carry out a multidimensional assessment of pain in cancer patients, including the intensity, location and nature of pain, sensory and affective components of pain, and their dependence on the type of cancer, age, and gender of the patient.
Material and methods
The study group consisted of oncological patients of the Pain Treatment Clinic of the Maria Sklodowska-Curie National Research Institute of Oncology in Warsaw, Poland. Patients were referred to the clinic by oncologists due to the presence of chronic pain associated with the course of cancer, which was not controlled with standard analgesic pharmacological treatment.
The study was voluntary and based on a single measurement during the first visit to the Pain Treatment Clinic.
The study was part of the research plan and was conducted in the period from January 2016 to December 2019.
Patients of the Pain Treatment Clinic underwent extensive pain diagnosis using standardized quality pain assessment tools. The study used an 11-point numerical rating scale (NRS) to assess pain intensity (where 0 means no pain and 10 the worst pain possible) and a qualitative pain assessment questionnaire (the McGill Pain Questionnaire, R. Melzack) to identify the location of pain, when it occurred, whether it was constant, if the pain worsened, in which situations that happened, and how the pain could be described.
Statistical analysis
Statistical analysis was performed using SPSS Statistics. The analysis of column proportions in the crosstabulation was performed with a Z test. The table values, where the column proportions differed significantly, were marked with different subscripts. Statistical significance of differences observed in subgroups was examined using the one-way analysis of variance (ANOVA). A significance level of 0.05 was adopted in all the calculations.
Results
The study included 661 patients (391 women and 270 men) aged 19 to 96 (mean age 64). The percentage distribution of cancer type and sex in the study population is shown in Table I.
Table I
Cancer type, sex. Crosstabulation. Each subscript letter denotes a subset of Sex categories whose column proportions do not differ significantly from each other at the 0.05 level
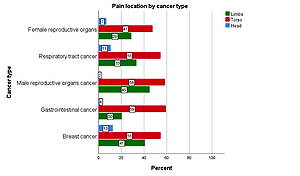
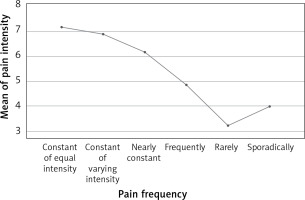
The analysis of the location of the perceived pain showed that the greatest number of patients experienced pain in the trunk area (53.4%), followed by pain in the limbs area (36.3%) and in the head area (11.9%). Detailed results of the location of the perceived pain depending on the type of cancer are presented in Figure 1.
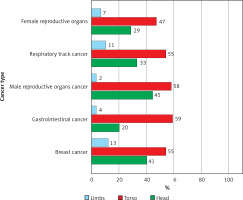
The analysis of the frequency of pain incidence in the study population (Figure 2) showed that the most numerous group consisted of patients with constantly felt cancer pain of varying severity – over half of them.
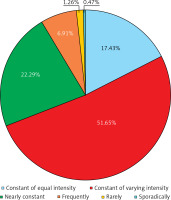
Low pain intensity (1-3 NRS points) was experienced by 58 patients, 214 respondents reported average pain intensity (4–6 NRS points), and high pain intensity (7–10 NRS points) was reported by 389 patients. Cross analysis of the frequency and level of pain showed that high pain levels were most often associated with constant pain of varying severity in 55.8% of all cases. The average intensity of pain most often coexisted with constant pain of varying intensity and it concerned 54.5%.
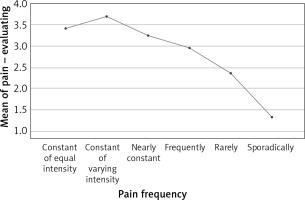
The analysis of the intergroup differences in the frequency of pain occurrence and its severity as well as the sensory, affective, and evaluator character showed a number of statistically significant results (intensity F = 10.958, p < 0.001, sensory F = 2.249, p = 0.048, affective F = 2.258, p = 0.047, evaluator F = 2.766, p = 0.018). Mean pain intensity, including severity on the sensory, affective, and evaluating dimensions, is detailed in Figures 3–6.
Figure 4
Analysis of intergroup differences in frequency of pain occurrence and its sensory dimension
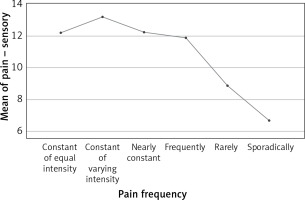
Figure 5
Analysis of intergroup differences in frequency of pain occurrence and its affective dimension
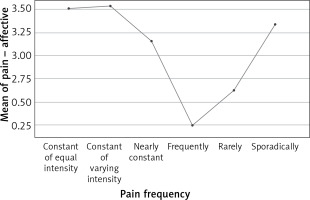
Figure 6
Analysis of intergroup differences in frequency of pain occurrence and its evaluating dimension
Analysis of the severity and nature of pain and its frequency in relation to the patients’ sex showed that men and women did not differ significantly (t = 0.440, p = 0.660) in terms of pain intensity; mean pain intensity was 6.68 and 6.77, respectively. There was also no significant difference in sensory pain (t = 0.382, p = 0.702). A difference was found in the context of the affective dimension of pain (t = 1.979, p = 0.049): women experienced higher pain in the affective dimension than men. With regard to the nature of the perceived pain, no significant difference (χ2 = 1.463, p = 0.917) was found between men and women. Both women (53.2%) and men (49.4%) most often reported persistent pain with varying severity. Overall, 22.1% of women and 22.6% of men reported that they felt pain almost constantly, and 16.8% of women and 18.3% of men reported that they experienced constant pain of the same intensity.
The analysis of the type of cancer with which women and men came to the pain treatment clinic showed that in women the most common cause of pain was breast cancer, which accounted for 37.6%, followed by reproductive organ cancers (14.6%) and gastrointestinal cancers (13.3%). In men, the most common causes of pain with which they reported to the Pain Treatment Clinic were male reproductive organ cancers (33%), followed by gastrointestinal cancers (18.9%) and respiratory cancers (16.3%).
An analysis of the nature of pain and its intensity in individual cancers is presented below.
In cancers of the respiratory system, the most frequent pain was: severe: acute (62.1), radiating (42.5), exhausting (41), lancinating (36.4), and beyond endurance (34.9).
In gastrointestinal cancers, the most frequent pain was: acute (50.5), exhausting (43.7), radiating (38.8), pressing (37.9), and lancinating (30.1).
In breast cancer, the most frequent pain was: acute (44.7), lancinating (36.2), pressing (36.2), rushing (36.1), radiating (35.6), and nagging (30.3).
In cancers of female reproductive organs, the most frequent pain was: acute (45.6), radiating (35.1), exhausting (33.4), nagging (29.8), and pressing (29.8).
In cancers of male reproductive organs, the most frequent pain was: acute (35.2), radiating (33), nagging (27.5), pressing (27), disturbing (23), and tiring (23).
Discussion
Pain is multidimensional in nature, consisting of nociception, pain perception, suffering and attitude towards pain, and behavioral expression of pain [14]. The amount and quality of pain experienced are determined by prior experiences (and memory of them), the ability to understand the cause of the pain and its consequences [15].
Pain diagnostics with the use of pain assessment questionnaires is a very valuable tool, facilitating both the patient and the doctor in assessing the scale of the health problem and selecting the appropriate treatment in order to achieve pain control. Often, extensive pain diagnostics makes it possible to diagnose all pain components, not only sensory, but also affective ones that require psychological and psychiatric therapy [16].
The subject of the research is the quantitative and qualitative development and characterization of pain sensations in the studied group. Experience is multifaceted and subjective; therefore most often there are not enough possibilities to make direct and objective assessments.
The result that is clinically very significant is that 90% of patients who came to the Pain Treatment Clinic had moderate or severe pain intensity, requiring immediate modification of the current treatment and implementation of additional adjuvant drugs. This finding corresponds with previous literature reports that up to 96% of oncological patients suffering from advanced diseases experience pain [17, 18].
In the studied population, regardless of the diagnosed cancer, the most frequent location of pain indicated by the patients was the torso and the least frequently the head (Figure 1). On the diagram, the examined patients indicated several locations of the perceived pain at the same time. This was due not only to the diagnosis that was the reason for the referral to the Pain Treatment Clinic, but also to other types of coincident pain. The coexistence of several types of pain in the patient resulted from the oncological disease, comorbidities and complications of oncological treatment. The results of the study population overlap with the clinical data, suggesting that patients with one type of pain are rare. According to the European Association for Palliative Care (EAPC), approximately 50% of cancer patients experience two to three types of pain simultaneously. More than 75% of oncology patients are likely to achieve pain control [19]. According to the EAPC recommendations, in order to achieve good pain control, it is necessary to diagnose all pain symptoms reported by the patient, thanks to which the appropriate analgesic treatment can be effectively adjusted and, if necessary, adjuvant drugs that treat neuropathic pain, anti-anxiety drugs, antidepressants, intestinal transit medications and many others can be used.
Another aspect of the analyzed pain was its frequency (Figure 2). Analyzing the frequency of pain occurrence helps to distinguish primary pain from episodic pain. In the study population, constant pain of varying intensity suggested the occurrence of more breakthrough pain episodes, which may indicate insufficient control of baseline pain or the appearance of end-of-dose pain. Such a situation requires in-depth diagnostics and modification of the current analgesic treatment. Patients who described their pain as constant and of varying severity at the same time described it in terms of affective and assessed it as: very distressing, tiring, depressing, exhausting, disturbing, terrible, excruciating and cruel. This proves that the perceived pain has an emotional component in addition to its sensory component. Constant pain of variable intensity is the most troublesome for the patient due to the high intensity of basic pain and the occurrence of unpredictable waves of pain of even greater intensity. The feeling of inability to predict when the pain will intensify influences the patient’s belief that he or she has no control over the disease, which generates anxiety, depression and sub-depressive states. It is difficult to get used to constant pain of varying severity and to habituate to it, as sometimes happens in the case with patients with pain of constant intensity. These patients are often on constant alert in the event of an increase in sustained pain intensity. In addition, this group of patients is at risk of self-administration of many over-the-counter pain medications for fear of worsening pain episodes [20].
Chronic pain is a disease in itself that needs to be treated. It is burdensome and affects the quality of life, functioning and therapeutic progress. This is confirmed by the results of pain at the sensory level, where the highest intensity was observed in the case of pain that occurs constantly and varies in intensity and occurs continuously with the same intensity (Figure 4). High pain intensity on the sensory dimension negatively affects all the patient’s sensory modalities, which in clinical practice may translate to the fact that the patient will report tactile, olfactory, visual, auditory and kinesthetic hypersensitivity. Additionally, patients often report eating disorders, disturbances in the circadian rhythm of sleep and wakefulness, and disturbances in mood and psychomotor drive. All these ailments result from pathophysiology where the consequence of constant pain is: disturbance of the ventilation-perfusion ratio, increase in cardiac output, increase in blood glucose, increase in blood pressure, increased secretion of digestive juices in the stomach, lipolysis, sodium and water retention, and increased levels of cortisol and lowered levels of serotonin and dopamine [19].
Assessment of pain in the affective and pain assessment dimensions (Figures 5 and 6) indicates that the most troublesome for the patients was again the constant pain of varying intensity or constant pain of constant intensity. Chronic pain reduces the quality of life and is an emotional burden on the emotional dimension, causes low mood, increased anxiety, subdepressive states, irritability and dysphoria. These results confirm that interdisciplinary cooperation is necessary in the treatment of pain, consisting in combining pain treatment with psychological therapy and psychiatric treatment, which increases the chance of achieving pain control [20].
The differences between sexes concern the affective and behavioral dimensions of pain. Differences in the assessment of pain at the affective level in men and women are mainly due to the biology of the brain and the endocrine system, while the behavioral differences in pain expression are often conditioned by social modeling. Socially, there is greater consent for women to verbalize their pain complaints and show it in behavior, while men are expected to be more tolerant of pain and not to show it outwardly. Such social pressure causes men to suppress, conceal and not report their ailments, which may not translate into the actual level of pain they feel [21].
In cancers of the respiratory system, it was observed that the reported pain was visceral pain with a neuropathic and emotional pain component. In the course of cancer of the respiratory system, and in particular the lungs, the tumor grows, the nerve structures are often infiltrated, and the vertebral bodies are damaged, which is another cause of pain. The disease is associated with reduced lung capacity, with infiltration of the pulmonary parenchyma, pressure on the upper and lower respiratory tract, and exudation into the pleural cavities. All these pathologies cause a feeling of shortness of breath, which in turn generates fear that intensifies the pain sensations. In addition, anxiety increases pain sensitivity and pain increases anxiety. The anxiety in patients with cancer of the respiratory system is usually very strong, as patients fear the development of shortness of breath and death from suffocation [22, 23]. In patients with lung cancer, acute pain occurs suddenly, is severe, and increases the feelings of breathlessness, anxiety and general suffering. Pain may be experienced in the pleura, chest wall, shoulder, and if there are also bone and/or brain metastases, headache and bone pain are often accompanied by pain, which may also have an additional neuropathic component. In some patients, pleural pain, which characteristically increases with respiratory movements, is defined as rushing, splitting, jerking, stabbing, and decreasing after the reduction of chest mobility (e.g. on the side affected by the process) [24]. It is associated with the presence of the tumor itself and metastatic changes in the ribs or the inflammatory process in the area affected by the tumor.
In gastrointestinal cancers, the disease is often detected after a longer period of non-specific symptoms treated as gastric ulcer, irritable bowel syndrome, and others. Patients included in the study reported acute, visceral pain localized in the lower abdomen and epigastrium, sometimes radiating to the lumbar region of the spine, kidneys, and pelvic bones. They are often debilitated patients, significantly underweight and with numerous additional troublesome symptoms, such as gastrointestinal bleeding, urge to stool, diarrhea, constipation, flatulence, dyspepsia, loss of appetite, nausea and vomiting. All of these symptoms lower the pain threshold and increase pain sensitivity. In addition, pain in cancer of the gastrointestinal tract contains a component of sympathetic pain, i.e. neuropathic pain. All this makes the pain extremely burdensome and causes great suffering for the patient.
In breast cancer, female patients reported a high intensity of acute, rushing, radiating and distressing pain. Breast cancer pain may result from crippling surgery, postmastectomy syndrome, and also from therapy. Chemotherapy often causes complications in the form of chemotherapy-induced peripheral neuropathy (CIPN), and radiotherapy causes fibrosis of irradiated tissues and damage to nerve structures. All these complications generate severe chronic pain. It should also be taken into account that breast cancer is strongly associated with endocrine disorders, which also affect emotional functioning. It is also an extremely emotional disease because it concerns the body, femininity, a sense of attractiveness and gender identity. Mastectomy is a disfiguring procedure, which is also important in the psychophysical condition of patients and the pain experienced. Patients are often afraid of rejection by their partner and intolerance of the appearance after surgery, which increases anxiety. After amputation of the breast and lymph nodes, lymphoedema occurs in the operated area and the hand on the operated side, limiting mobility. Moreover, frequently used hormone therapy leads to changes in the levels of neurotransmitters responsible for mood and psychomotor drive.
The nature of the pain perceived by the patients with female cancer of the reproductive organs caused by the growth of the neoplastic tumor, but also by the infiltration of the adjacent structures of the urinary and digestive systems, can be caused by the often occurrence of hydronephrosis, vaginal-bladder and vaginal-rectal fistulas. Pain is also associated with a complication of radiotherapy, which often leads to the formation of adhesions and fistulas, and chemotherapy that causes polyneuropathy. Tumors of the reproductive system are closely related to hormonal balance, which also translates into problems with pain. In the assessment of pain, the emotional and social component of pain should also be taken into account because this type of cancer is associated with a feeling of loss of femininity and mutilation. In addition, there is anxiety related to fertility. All of these factors generate anxiety, and this increases pain sensitivity.
Patients with urinary system cancers reported acute, radiating, pressing and nagging pain of the highest severity. Two groups predominated among patients with tumors of the urinary system: patients with testicular cancer and patients with prostate cancer. Due to different conditions related to age and stage of life, they should not be treated as homogeneous groups. Testicular cancer affects very young men, most often between the ages of 16 and 30. Apart from the crisis related to the diagnosis of the disease with cancer, there are numerous development crises. These are men who are in the period of early adolescence, when they begin to live independently, away from their family, take their first job, make the first important decisions in life, such as buying a flat, partnership/marriage and many others. This is a period in life when physical attractiveness and sexual performance, as well as the ability to have children, are of great importance. Testicular cancer affects all spheres of life of young men. Therefore, in addition to the pain associated with the disease itself, there are also emotional components, such as sadness, fear and anxiety, anger and frustration, that complicate the perception of pain.
Patients with prostate cancer constitute a group of patients aged 60+. These are patients who often already have a stable life and intimate situation. They also have offspring, and physical attractiveness and sexual performance are no longer as important. Moreover, these patients often express a high level of acceptance of the disease [25]. Therefore, in these patients, pain is mainly due to the pathology of the neoplastic disease itself and the side effects of hormone therapy, radiotherapy and chemotherapy. Hormone therapy causes, among other consequences, the occurrence of andropause with symptoms such as decreased libido, sweating, urinary incontinence, micturition disorders, and erectile disorders. Mood disorders with an anxiety component may be associated with hormone therapy. Radiotherapy often causes radiation damage to the intestines with a feeling of fecal urgency and damage to the bladder with impaired micturition. Complications of treatment may also contribute to increased pain intensity.
To sum up, the correct diagnosis of pain in a patient with cancer should take into account the assessment of medical factors, but also all comorbidities as well as the emotional and social functioning of the patient. This direction of diagnosis will make it possible to accurately construct a pain treatment plan containing analgesic drugs in accordance with the analgesic ladder, but also allow the inclusion of adjuvant drugs: anxiolytics, antidepressants, and antiepileptics. In addition, good pain control depends not only on the use of appropriate pharmacotherapy, but also on provision of psychological, psychiatric, and social therapy. Therefore, multidisciplinary cooperation in caring for a patient with cancer pain is necessary.
In conclusion, the vast majority of patients who came to the Pain Treatment Clinic for help (90%) experienced moderate (4–6 NRS points) or severe pain intensity (7–10 NRS points). Moreover, almost 50% of them reported constant pain with varying severity.
The findings of the research, as well as studied literature, show that pain is not only a medical challenge, but also a clinical, psychological, and socio-economic issue.
Pain has a multi-dimensional nature that consists of nociception, pain perception, suffering and attitude towards pain, and behavioral expression of pain. Therefore, when assessing pain, it is not sufficient to determine its intensity, but it is also necessary to determine its etiology, localization, and its affective, evaluative, and behavioral dimensions.
Effective pain control increases the patient’s quality of life, reduces the severity of comorbid symptoms, stabilizes the mood, increases the motivation to fight the disease, and increases cooperation with medical staff.