Introduction
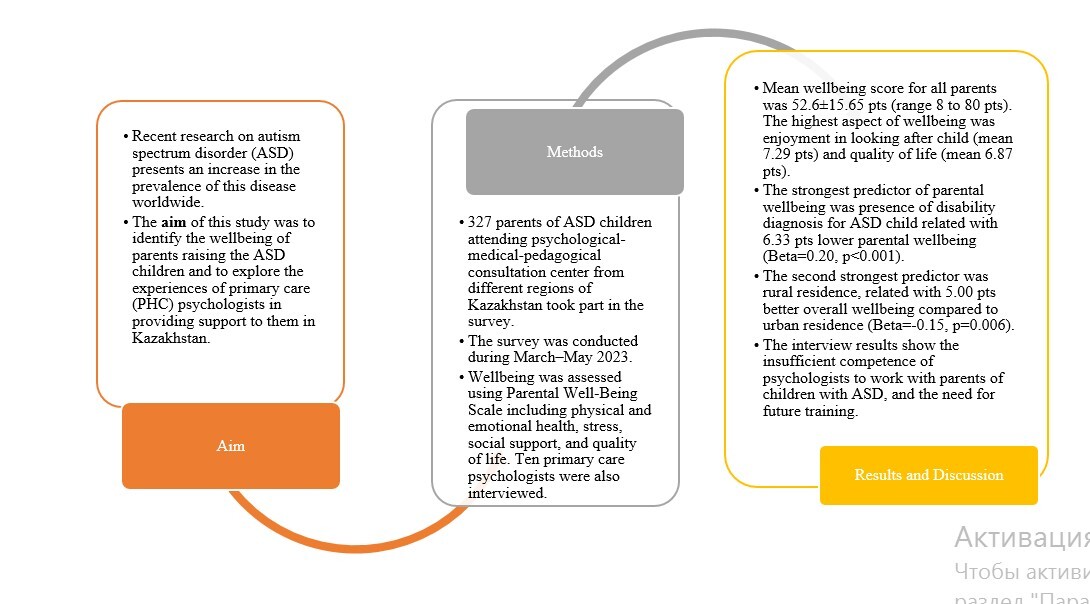
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by “varying but often marked and persistent deficits in social communication and social interaction, including difficulties with social-emotional reciprocity, non-verbal communication behaviors, and social relationships, along with restricted and repetitive patterns of interests, behaviors, and/or activities” [1]. During recent decades, there has been an increase in the number of identified cases of ASD children. According to Salari et al. the prevalence of ASD ranges from 0.02% in China to 3.66% in Sweden [2], whereas Zeidan et al. estimated the median prevalence of ASD worldwide as 65/10 000 [3].
The condition of a child with ASD and care for them affect the psychological state of the parents of that child. The systematic review and meta-analysis by Schnabel et al. revealed the presence of depressive disorders as 31%, anxiety disorders 33%, obsessive-compulsive disorder 10%, personality disorders 4%, alcohol and substance use disorders 2%, and schizophrenia spectrum disorders 1% [4]. Studies showed that parents of ASD children are more stressed than parents of normal children and even parents with other diseases [5, 6]. The psychological state of parents with ASD children may be due to a number of factors such as additional expenses and change in social status, low physical health, child’s age, severity of autistic symptoms, child’s sex, and absence of access to individual therapy [7–10]. In addition, parents of ASD children had low mental health, which manifested as anxiety and depression [11]. Thus, previous studies showed that the well-being of parents of children with ASD is worse, which is reflected by stress symptoms (negative parental self-views, lower satisfaction with parent-child bond, etc.) or depressive states [12, 13].
In Kazakhstan the identification of ASD children is carried out by contacting various healthcare professionals (such as general practitioners, pediatrics, psychiatrists, speech therapists, speech pathologists, and neurologists) [14]. Costs related to medical treatment for children including those with ASD are free and covered by the State Benefit Package [15]. Children aged 0–18 years are eligible to undergo the screening procedures at home and at health facilities by the trained medical specialist. Moreover, the clinical protocol “General disorders of psychological (mental) development (autism spectrum disorders)” approved by the Joint Committee on Quality of Health contains all recommended procedures for children and caregivers (including the ASD screening tool M-Chart-R/F).
The parents are also a resource for ASD children – in addition to organized services not only within health care, but also in social and educational fields. Therefore, the patient-oriented perspective on ASD alone may not always be sufficient to provide the ASD children with the best care and assistance they need. However, many studies on parental health have been conducted in Western countries, where the psychological states of the parents of children with ASD were assessed, and they also have more resources to provide multidisciplinary and professional assistance [12, 13, 16]. Meanwhile, research from developing countries is limited and highlights the insufficient health resources to support parents of children with ASD, as well as the importance of taking into account the cultural aspects of the country [17, 18]. Given the fact that the parents of ASD children can suggest areas of improvement related to the family and close social environment around the child, the aim of this study was to identify the wellbeing of parents raising ASD children and to explore the experiences of primary health care (PHC) psychologists in providing support to them in Kazakhstan.
Material and methods
To fulfil the aim of this study, the mixed method approach was used, with a sequential design. In the first phase, the quantitative survey for parents of ASD children was organized. Then, in the second stage, qualitative interviews were conducted with psychologists of primary health care. The study design was approved by the Research Ethics Committee of SDU University, Kazakhstan (Protocol No. 6, 6 March 2023).
Quantitative survey
The cross-sectional survey was conducted with a target group of parents with ASD children. We adapted the Parental Well-Being Scale questionnaire developed by McConkey R. [6]. The questionnaire was provided in Kazakh and Russian languages (the majority of the population in Kazakhstan use these two languages) and posted online using Google Forms. Researchers of the project conducted the survey. Participants filled in the questionnaires independently. The questionnaire comprised two sections – parental wellbeing and sociodemographic items. The questionnaire was adapted using back-translation. Four independent experts carried out the translation process: the first translated from English into Russian, the second from English into Kazakh, the third from Russian into English, and the fourth from Kazakh into English. The criteria for selecting two translators for translation from English into Russian and Kazakh were the presence of a diploma as a translator and participation in health care projects. Thus, they had experience and knowledge in medical terminology. Retranslation was performed by two independent experts who were at doctoral level in Public Health and educated in foreign English-speaking countries (with proficiency in English). They were involved in translation from Russian and Kazakh into English. In addition, to ensure clarity and readability of the survey questions, we conducted a pilot survey among 5 parents of ASD children as well as 8 healthcare specialists from medical universities: neurologists (n = 2), psychologists (n = 2), biostatisticians (n = 2), and public health specialists (n = 2). For the pilot testing of the questionnaire, we selected parents based on their education: having a higher education, preferably in medicine, nursing, or related to social service or experience working with children with ASD. Our project initially involved two parents with ASD children; they were involved in pilot testing of the questionnaire and three others were selected from the National Psychological-Medical-Pedagogical Consulting Center (NPMPC). In pilot survey, the participants were given the questionnaire in its preliminary format with the chosen scales to receive the comments if items’ text and formulations were clear. When receiving feedback, we focused on perception and understanding of the survey questions. Experts from the local ethical committee (which included a specialist with knowledge of the care of patients with ASD) were taken into account in adaptation of the questionnaire. The scale includes 8 items assessed on a 10-point Likert rating scale (where 1 is poor and 10 is good). Items address physical and emotional health, stress, coping, social support and quality of life of parents with ASD children. The following significant variables were taken into account for the regression analysis: disability diagnosis, residency, family status from all the variables such as: age of respondents, marital status, working status of parents in family, education, residence, child’s age, child’s disability diagnosis, level of income. Variables were selected based on their associations with the primary outcome of interest. The total score was calculated as the sum of eight items, ranging from 8 to 80, with higher scores indicating better parental wellbeing. In this study, the internal consistency of the scale was Cronbach’s α 0.89.
The target sample of the survey consisted of parents with ASD children registered at a psychological-medical-pedagogical consulting center in all regions of Kazakhstan to cover Western, Southern, Eastern, Northern Kazakhstan, and three metropolitan cities. The NPMPC is an arm-length governmental organization, which has branches in all regions of Kazakhstan. In addition, it is responsible for collecting the national data of children with special educational needs, providing educational and methodological support to regional educational facilities and preparing proposals for the legislative documents for the Ministry of Education. At the NPMPC, children with ASD receive pedagogical and other services. At this time parents or guardians of children with ASD are in the waiting room. Thus, we invited to participate in the survey parents or guardians of children with ASD who were in the waiting room in the NPMPC.
It was planned to reach 384 parents. After processing, 57 questionnaires that had not been completed qualitatively were identified. As a result, 327 questionnaires were included in the analysis. The survey was conducted during March–May 2023. The participation of parents was voluntary, with prior consent to participate being obtained. Before starting to fill in the questionnaire, there was also a tick box where participants were informed about the survey and agreed to participate.
Qualitative interviews
The purpose of interviews was to investigate the current practices how psychologists in PHC provide assistance to parents of ASD children and what needs the psychologists have when providing support and assistance to such parents. The interview was conducted among ten psychologists from ten different PHC facilities where ASD children registered. Five of these PHC facilities were located in the city, the remaining five at the district level. In these PHC facilities where we interviewed psychologists, there was only one psychologist working. In Kazakhstan from 2013 per 10000 registered populations who receive PHC services, one psychologist is recommended. However, in Kazakhstan this standard is not always met due to a lack of specialists.
The interviewer visited ten PHC facilities to interview psychologists face to face. The interviewer was a trained project researcher. The interview took place in the psychologists’ office without strangers, so that the psychologist would not be distracted by anything and answers would be kept confidential. The interviewer wrote down the psychologists’ answers on paper. The interview took about 15–25 min. In interviews, the following questions were asked:
Do you know if there are registered children with ASD in this PHC facility? What is the number of registered children with ASD in this PHC facility?
Have you had experience providing psychological support to parents of children with ASD? Do you provide support to parents of children with ASD in this PHC facility? If the answer was positive, then What kind of work do you do with them? What symptoms did they most often experience? Stress or anxiety, or something else? Do you have a plan for monitoring their condition? What difficulties do you encounter when helping parents of children with ASD? If the answer is negative, then Why you did not contact or provide assistance to parents of children with ASD? What is this associated with?
What are your general needs for helping parents of ASD children? Do you need training, and if so, on what issues? What duration?
Will there be any other additions or suggestions on this topic?
The analysis of the results was carried out by coding the main results using keywords. For example, for the first question, the presence of experience or lack thereof was divided into two categories. A separate analysis was carried out on those who have experience and those who do not; have interests in parents and guardiancy health condition or not; common symptoms in psychological support; future needs as training or other needs.
Statistical analysis
All data were entered into an SPSS spreadsheet along with relevant details of parent and child characteristics. Statistical analysis was carried out using the SPSS software (IBM Corp. Released 2020. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp). The significance level was set at p < 0.05.
In descriptive analyses, the data were reported in absolute numbers and percentages (%) as well as means and standard deviations (M ± SD) for continuous variables. To establish the potentially vulnerable groups, which could be in greater need of help and assistance, we made a comparison. To compare the wellbeing of parents depending on residence and marital status, as well as the child’s diagnosis of disability, the independent samples t-test was used. One-way ANOVA was used to compare the subjective wellbeing of parents with sociodemographic indicators. The Pearson correlations were calculated for associations between continuous variables, the Spearman correlations in the case of ordinal variables. The 95% confidence intervals (CI) were also calculated. Cronbach’s α was calculated to measure internal consistency.
Finally, linear regression was conducted to find independent variables of parental wellbeing. The model was built as explanatory (not predictive); therefore its model fit and equation were not assessed [19]. The effect size of factors was expressed in standardized β coefficients (β).
Results
Wellbeing of parents with ASD children
In our study 327 parents of children with ASD participated. The majority of participants were aged 25–44 years, and more than a third were married and from urban areas. Slightly more than half of the respondents had higher education (59.3%). From the perspective of ASD children of participants, in the majority of the cases children were aged more than 3 years and mostly had an approved diagnosis of autism according to ICD-10 from psychiatrics of the primary care provider or mental health centers (62.8%). The detailed characteristics of the study sample are presented in Table I.
Table I
Demographic and clinical characteristics of study sample
The mean wellbeing score for all parents was 52.6 ±15.65 points. The highest aspect of wellbeing was enjoyment in looking after the child (mean 7.29 points out of 10), which can be interpreted as above average, whereas quality of life (mean 6.87 points out of 10) was moderate. The lowest wellbeing aspect was feeling great (mean 5.97 points out of 10; Table II). Comparison of the total parental wellbeing by demographic and clinical characteristics revealed that parents in rural areas reported higher wellbeing (p = 0.003), as did parents of children without a diagnosed disability (p < 0.001). These subgroup differences were quite consistent across different aspects of parental wellbeing (Table II).
Table II
Parental wellbeing and its aspects by demographic and clinical characteristics (M ± SD)
| Variable | Value | 1. Overall health | 2. Feeling great | 3. Feeling relaxed | 4. Having others for support | 5. Enjoy looking after child | 6. Daily household tasks | 7. Going out of home | 8. Quality of life | Total wellbeing |
|---|---|---|---|---|---|---|---|---|---|---|
| Min-max values for the given subscales | 1–10 | 1–10 | 1–10 | 1–10 | 1–10 | 1–10 | 1–10 | 1–10 | 8–80 | |
| Total sample | 6.57 ±2.43 | 5.97 ±2.69 | 6.13 ±2.62 | 6.55 ±2.95 | 7.29 ±2.52 | 6.51 ±2.60 | 6.51 ±2.71 | 6.87 ±2.45 | 52.60 ±15.65 | |
| Age | 18–24 years | 8.40 ±1.52 | 6.80 ±1.92 | 7.60 ±2.07 | 7.00 ±3.32 | 8.00 ±2.55 | 6.8 ±3.42 | 7.00 ±2.92 | 8.20 ±2.17 | 59.80 ±18.29 |
| 25–34 years | 6.57 ±2.54 | 6.11 ±2.81 | 6.18 ±2.66 | 6.96 ±2.82 | 7.21 ±2.62 | 6.53 ±2.63 | 6.73 ±2.56 | 6.91 ±2.54 | 53.53 ±16.65 | |
| 35–44 years | 6.61 ±2.33 | 5.84 ±2.68 | 6.05 ±2.67 | 6.38 ±3.04 | 7.40 ±2.36 | 6.62 ±2.57 | 6.20 ±2.69 | 7.04 ±2.29 | 52.29 ±14.71 | |
| 45+ years | 5.83 ±2.25 | 5.82 ±2.25 | 6.07 ±2.34 | 5.59 ±2.75 | 6.79 ±2.96 | 5.63 ±2.5 | 6.86 ±3.37 | 5.52 ±2.61 | 48.81 ±15.46 | |
| P-value | 0.131 | 0.732 | 0.621 | 0.105 | 0.588 | 0.328 | 0.321 | 0.011* | 0.368 | |
| Marital status | Divorced, widowed, single | 6.04 ±2.20 | 5.33 ±2.58 | 5.66 ±2.80 | 6.04 ±3.2 | 7.19 ±2.64 | 6.51 ±2.89 | 6.40 ±2.86 | 6.25 ±2.61 | 49.9 ±16.08 |
| Married | 6.68 ±2.46 | 6.13 ±2.69 | 6.26 ±2.56 | 6.70 ±2.87 | 7.30 ±2.49 | 6.5 ±2.52 | 6.53 ±2.67 | 7.04 ±2.39 | 53.34 ±15.48 | |
| P-value | 0.073 | 0.025* | 0.084 | 0.094 | 0.737 | 0.977 | 0.718 | 0.017* | 0.104 | |
| Working status | Both parents work | 6.70 ±2.23 | 6.05 ±2.39 | 6.31 ±2.45 | 6.69 ±3.05 | 7.56 ±2.38 | 6.27 ±2.59 | 6.87 ±2.64 | 7.11 ±2.13 | 53.66 ±14.17 |
| One parent work | 6.50 ±2.44 | 5.91 ±2.78 | 6.06 ±2.67 | 6.44 ±2.89 | 7.20 ±2.59 | 6.58 ±2.56 | 6.39 ±2.71 | 6.75 ±2.6 | 52.18 ±16.38 | |
| Both parents do not work | 6.50 ±3.04 | 6.00 ±3.02 | 6.00 ±2.96 | 6.96 ±3.21 | 6.88 ±2.38 | 6.83 ±2.99 | 5.96 ±2.85 | 6.88 ±2.35 | 51.92 ±15.20 | |
| P-value | 0.790 | 0.908 | 0.733 | 0.622 | 0.370 | 0.514 | 0.214 | 0.512 | 0.730 | |
| Education | School | 6.95 ±2.78 | 5.86 ±3.04 | 5.77 ±3.09 | 6.56 ±3.39 | 7.84 ±2.59 | 7.02 ±2.84 | 6.48 ±2.91 | 7.41 ±2.5 | 54.37 ±16.54 |
| College | 6.43 ±2.54 | 6.07 ±2.7 | 6.29 ±2.67 | 6.36 ±3.22 | 7.47 ±2.64 | 6.85 ±2.68 | 6.47 ±2.76 | 6.85 ±2.66 | 52.93 ±17.13 | |
| Higher (university) | 6.52 ±2.29 | 5.93 ±2.61 | 6.13 ±2.49 | 6.64 ±2.72 | 7.06 ±2.43 | 6.22 ±2.48 | 6.52 ±2.65 | 6.75 ±2.33 | 52.03 ±14.72 | |
| P-value | 0.492 | 0.893 | 0.558 | 0.760 | 0.131 | 0.062 | 0.991 | 0.272 | 0.657 | |
| Residence | Rural | 6.83 ±2.59 | 6.34 ±2.79 | 6.56 ±2.89 | 6.86 ±2.92 | 8.08 ±2.34 | 6.89 ±2.64 | 7.1 ±2.75 | 7.47 ±2.50 | 56.33 ±16.83 |
| Urban | 6.42 ±2.33 | 5.78 ±2.62 | 5.92 ±2.47 | 6.41 ±2.96 | 6.91 ±2.52 | 6.32 ±2.57 | 6.21 ±2.65 | 6.58 ±2.38 | 50.83 ±14.77 | |
| P-value | 0.155 | 0.074 | 0.040* | 0.197 | < 0.001 | 0.065 | 0.006* | 0.002* | 0.003* | |
| Child’s age | Under 3 years | 7.24 ±2.48 | 6.50 ±2.73 | 6.13 ±3.00 | 6.72 ±3.21 | 7.20 ±2.46 | 6.35 ±2.88 | 7.02 ±2.45 | 7.09 ±2.65 | 54.67 ±17.87 |
| 4 to 6 years | 6.28 ±2.42 | 5.98 ±2.65 | 6.15 ±2.48 | 6.76 ±2.74 | 7.28 ±2.52 | 6.41 ±2.51 | 6.63 ±2.63 | 6.73 ±2.35 | 52.45 ±14.58 | |
| 7+ years | 6.59 ±2.38 | 5.77 ±2.70 | 6.11 ±2.64 | 6.32 ±3.05 | 7.31 ±2.56 | 6.64 ±2.60 | 6.23 ±2.84 | 6.91 ±2.49 | 52.11 ±15.88 | |
| P-value | 0.067 | 0.268 | 0.990 | 0.414 | 0.967 | 0.686 | 0.172 | 0.657 | 0.624 | |
| Child’s diagnosis of disability | Yes | 6.21 ±2.49 | 5.44 ±2.76 | 5.80 ±2.65 | 6.38 ±3.01 | 7.11 ±2.60 | 6.28 ±2.72 | 5.93 ±2.78 | 6.53 ±2.48 | 49.96 ±15.78 |
| No | 7.14 ±2.19 | 6.84 ±2.30 | 6.70 ±2.48 | 6.85 ±2.84 | 7.58 ±2.35 | 6.90 ±2.34 | 7.46 ±2.30 | 7.72 ±2.32 | 57.08 ±14.41 | |
| P-value | 0.001* | < 0.001** | 0.002* | 0.159 | 0.106 | 0.036* | < 0.001** | 0.002* | < 0.001** | |
| Level of income (tenge) | Up to 70 thousand | 6.87 ±2.59 | 5.87 ±2.90 | 5.47 ±3.02 | 7.38 ±3.44 | 7.87 ±2.80 | 6.36 ±2.47 | 6.06 ±3.26 | 7.27 ±2.22 | 53.13 ±12.05 |
| 71–150 thousand | 6.26 ±2.36 | 5.85 ±2.70 | 6.07 ±2.58 | 6.17 ±3.06 | 7.30 ±2.37 | 6.45 ±2.48 | 6.32 ±2.56 | 6.47 ±2.47 | 50.96 ±14.84 | |
| 151–250 thousand | 6.31 ±2.52 | 5.85 ±2.64 | 6.00 ±2.66 | 5.94 ±2.87 | 6.98 ±2.62 | 6.51 ±2.71 | 6.30 ±2.76 | 6.76 ±2.48 | 51.25 ±16.78 | |
| 251+ thousand | 6.99 ±2.31 | 6.22 ±2.68 | 6.45 ±2.53 | 7.36 ±2.68 | 7.50 ±2.50 | 6.54 ±2.63 | 6.94 ±2.70 | 7.29 ±2.41 | 55.41 ±15.52 | |
| P-value | 0.100 | 0.705 | 0.409 | 0.001* | 0.370 | 0.991 | 0.240 | 0.096 | 0.153 | |
To determine which demographic and clinical indicators might be independent factors for parental wellbeing, first the bivariate analysis was conducted. In general, the majority of correlations were non-significant (Table III). However, two aspects could be noted: first, younger parents with younger ASD children tended to report lower support from friends and others (rho = –0.12 and –0.14), while higher parental education correlated with more enjoyment in looking after the child and better management of day-to-day tasks of running a home (rho = 0.14) (Table III). As regards other indicators, it was observed that married marital status, rural residence, and absence of disability diagnosis were all related to better wellbeing of parents with ASD children (Table IV).
Table III
Correlations of wellbeing indicators by child and parent characteristics
| Aspect of wellbeing | Child’s age | Parental age | Working status | Parental education |
|---|---|---|---|---|
| 1. Overall health | –0.30 | –0.07 | –0.02 | 0.05 |
| 2. Feeling great | –0.07 | –0.06 | –0.01 | 0.02 |
| 3. Feeling relaxed | –0.06 | –0.04 | –0.03 | 0.00 |
| 4. Having others for support | –0.12* | –0.14* | –0.02 | 0.00 |
| 5. Enjoy looking after child | –0.07 | –0.01 | –0.08 | 0.14* |
| 6. Daily household tasks | –0.01 | –0.05 | 0.07 | 0.14* |
| 7. Going out of home | –0.06 | –0.04 | –0.09 | –0.01 |
| 8. Quality of life | –0.06 | –0.09 | –0.03 | 0.08 |
| Total wellbeing | –0.08 | –0.09 | –0.04 | 0.05 |
Table IV
Comparisons of wellbeing indicators by child and parent characteristics
| Aspect of wellbeing | Marital status | Residence | Disability diagnosis | |||
|---|---|---|---|---|---|---|
| t | P-value | t | P-value | t | P-value | |
| 1. Overall health | 1.84 | 0.070 | 1.37 | 0.170 | –3.35 | < 0.001** |
| 2. Feeling great | 2.28 | 0.020* | 1.73 | 0.090 | –4.86 | < 0.001** |
| 3. Feeling relaxed | 1.74 | 0.080 | 1.95 | 0.050 | –3.07 | < 0.001** |
| 4. Having others for support | 1.66 | 0.100 | 1.33 | 0.190 | –1.45 | 0.150 |
| 5. Enjoy looking after child | 0.37 | 0.710 | 4.08 | < 0.001** | –1.70 | 0.090 |
| 6. Daily household tasks | –0.02 | 0.990 | 1.76 | 0.080 | –2.09 | 0.040* |
| 7. Going out of home | 0.24 | 0.810 | 2.70 | 0.010* | –5.25 | < 0.001** |
| 8. Quality of life | 2.22 | 0.030* | 3.07 | < 0.001** | –3.17 | < 0.001** |
| Total wellbeing | –2.95 | < 0.001** | 2.99 | < 0.001** | –4.04 | < 0.001** |
The findings indicated that the presence of a child’s disability is factor strongly influencing the negative well-being of parents of children with ASD with 6.33 points out of 10 lower parental wellbeing (β = 0.20, p < 0.001).
The second strongest predictor was rural residence, related to 5.00 points out of 10 better overall wellbeing compared to urban residence (β = –0.15, p = 0.006). Meanwhile, family status was non-significant (Table V). Other demographic and clinical factors were not included in the multivariate analysis due to their non-significance in bivariate calculations.
Qualitative insights of PHC psychologists
The age of interview participants was from 22 to 50 years. The work experience of 10 PHC psychologists ranged from 1 to 15 years.
Only in one PHC facility did the psychologist not know how many ASD children were registered; in the others, psychologists had this information. Even with knowledge of the presence of ASD children, psychologists were not always interested in the health status of parents or guardians of ASD children. In general, psychologists have placed more emphasis on working with children themselves rather than with parents. Only three psychologists noted the following work with parents of ASD children:
rural PHC psychologist: “provides psychological support to parents of ASD children, but only if necessary and at the request of parents themselves”;
city PHC psychologist: “Parents do not turn to a psychologist, and there is also no action plan for the management of ASD children. However, in accordance with regulatory documents, the PHC facility can be contacted for advice and assistance”;
city PHC psychologist: “Parents are provided with psychological support in the form of a conversation. During conversation, we study the parent first. With a special child, it is most difficult for mothers and they must first be diagnosed with depression, anxiety, and stress. Afterwards, parents carry out psycho-correction. It happens that a parent initially refuses to talk about his problems concerning their child. This may be because the parents themselves did not completely accept their situation with the ASD child. But after a conversation and diagnosis, it can be easier to work with parents”.
All psychologists unanimously noted the need for their own professional training. For example, they noted “It is necessary to train medical staff at the PHC facility in organizing and conducting therapeutic, preventive, and psychosocial assistance to parents of ASD children” or “… for children with special needs, it is imperative to work with their parents, as they perceive it painfully and become more vulnerable, so first of all, working with the parents is mandatory. To do this, we need to train our psychologists, introduce some kind of algorithm, definitely some kind of program”.
Discussion
It was found that wellbeing of parents raising the ASD children was slightly above the theoretical scale’s mean, with the highest scores for enjoyment in looking after the child and quality of life. In addition, rural residence and the children with ASD lacking disability status are the conditions related to significantly higher parental wellbeing. Previous research identified that parents of an ASD child had higher levels of depression symptoms in comparison to parents of typically developing children [18]. Our results, similarly to other research, including in Kazakhstan, showed the presence of stress in parents of ASD children [20]. Research highlights the presence of anxiety as well as the greater stress-related somatic complaints among parents or caregivers of children with ASD [21–23]. The level of stress depends on the profile of parents of children with ASD, two-parent or single-parent families. Moreover, factors contributing to the psychological state in parents or caregivers may be related to higher levels of stress when caring for children with ASD and difficulties in management that are associated with the condition or severity of the child’s illness and adaptive abilities [24].
Also, we identified a higher mean wellbeing score for all parents (52.6) than Roy McConkey’s results (50.29) [6]. In this study, the author introduced an intervention to increase the mean wellbeing score to 57.6 [6], which indicates the need to introduce measures to improve the health of parents of children with ASD in Kazakhstan.
In Kazakhstan, PHC includes the services of a general practitioner and specialized physicians, including psychologists and a healthy lifestyle specialist. Our study revealed insufficient work by psychologists with parents of children with ASD. This is most likely due to the fact that in Kazakhstan, as a post-Soviet country, there was no training of clinical psychologists. However, recent changes in the education system have made it possible to introduce double-diploma and other programs at the master’s level that make it possible to train psychologists in healthcare. PHC also has additional resources to improve the skills of employees, including psychologists. When training psychologists, their skills to work in a multidisciplinary team are important. Multidisciplinary support is necessary in the first step for parents or caregivers of children with ASD to accept the diagnosis. Early acceptance of the diagnosis by parents or caregivers of children with ASD allows effective treatment and interaction with the child [25]. In addition, the adaptation of parents in the upbringing of ASD children and the development by an interdisciplinary team are crucial to support and improve the quality of life of parents [12, 26]. Gowin et al. showed the effectiveness of a program to improve the quality of medical care in primary care, which was based on assessing the frequency of preventive procedures performed by GPs [27]. This program can serve as an example for the development of a similar program to assess the effectiveness of a multidisciplinary team in primary care in providing support and assistance to children with ASD and their parents.
In this regard, it is necessary to develop a model for helping parents of ASD children, including an assessment of their psychological and physical state. The development of the model should emphasize the health of the mother, as some studies note that mothers of ASD children have more stress [10, 28]. Given the social and cultural aspects of people living in Kazakhstan, this factor may take effect in the upbringing of ASD children [29]. Also, other psychological programs for parents with moderate to severe anxiety and/or depression, such as the SilverCloud study, can be adapted in PHC in Kazakhstan [30]. Karst and Van Hecke suggested a model of treatment evaluation which includes child outcomes and parent outcomes [31]. Another randomized trial showed the effectiveness of the Acceptance and Commitment Therapy program, where parents were able to overcome stress more quickly compared to a control group that did not participate there [32]. Moreover, low physical activity of ASD children has also been reported, which also affects their quality of life [11].
Another aggravating factor in the health of parents of children with ASD is a decrease in their immune system, which negatively affects their overall health condition [33]. To improve care, it is important to understand the priority concerns of parents of ASD children, which may be related to other sectors – education and social services [34, 35]. In Kazakhstan, issues of strengthening interdisciplinary cooperation are outlined in the state programs [36]. Consequently, in PHC it is possible to create conditions for the work of a multidisciplinary team involving GPs, nurses, psychologists, neurologists and the parents of children with ASD themselves. Our analysis shows on the positive side that the majority of respondents have higher education and college degrees. This can help to quickly understand on the part of parents the importance of their participation in the treatment process and support of their children. In general, it is worth noting that in Kazakhstan there is accessible education, financed by the state; accordingly, the majority of the population have completed a course at a higher education institution, or at least college, allowing them to start working.
Nurses can coordinate and support families with an ASD child [37]. Nursing education is being reformed in Kazakhstan, as is a review of the function of nurses, with a number of tasks being transferred from the physician to nurses [38, 39]. In this regard, nurses, within the framework of the developed model, can take on the functions of coordinating care for parents of ASD children. Moreover, the insufficient work of psychologists in PHC with parents of ASD children in Kazakhstan is most likely due to the need for their training. The results of our study with psychologists clearly indicate the need for training. Eventually for an effective and functioning model, it is necessary to take into account the above aspects, making it possible to cover the minimum range of assistance to parents of ASD children at the PHC level.
Social stigma can also be a reason for the development of stress among parents of ASD children, and it is important to raise public awareness [40]. For instance, a study of the awareness of the population of Kazakhstan about autism showed that it is at a low level, although this is one of the important factors for accepting families with children with ASD [41]. Therefore, local executive bodies need to develop measures to disseminate correct information through social media and other means.
Limitations: We initially planned to reach a larger number of respondents; however, due to mental and cultural differences, many parents of children with ASD did not agree to participate. This may be due to a culture where having a child with autism is perceived as shameful. Similarly, Meyrav Gaziel-Guttman found that the adult population has a higher level of shame in comparison to the younger population [42]. We were only able to interview 10 psychologists, and a limitation was their differences in work experience, which may affect the interpretation of the results. In the future, it is important to conduct intervention studies related to psychological support and the provision of multidisciplinary team assistance to parents of children with ASD at the city and village level, which can evaluate their effectiveness. There is also a need to explore the influence of culture and society in supporting parents of children with ASD. The questionnaire was adapted with the involvement of all stakeholders (parents of children with ASD, psychologist, neurologist, public health specialist, certified translators). Therefore, it may be necessary to interpret the results with caution.
In conclusion, the wellbeing of parents raising ASD children is slightly above the theoretical mean of the Parental Well-Being Scale, with the highest scores for enjoyment in looking after the child and quality of life. The strongest predictors for better parental wellbeing were rural residence and the children with ASD lacking disability status. Insufficient work is carried out by primary health care psychologists with parents of children with ASD, which is most likely due to low knowledge on how to support them and monitor their condition. Consequently, there is a need for future training of psychologists in the management of children with ASD and their parents.