The number of patients operated due to degenerative spinal disease is constantly increasing. This condition is caused by the ageing of the population, the development of new surgical techniques and stabilizers, generally available imaging diagnostics, and high public awareness of a dignified life without pain [1–3]. The number of reoperations increases with the increase in the number of operations. Reoperation is commonly due to the progression of degenerative lesions and adjacent segment disease.
The development of degenerative lesions in the segment adjacent to the stabilized lumbar or lumbo-sacral segment is referred to as adjacent segment disease and may require surgical intervention in the future [4].
There is an ongoing debate in the literature as to whether adjacent segment disease is the result of spondylodesis or the progression of degenerative lesions [5–7]. Moreover, an increasing number of reports discuss adjacent segment disease as a consequence of previous stabilization.
The concept of stabilizing the operated segment as a method of treatment of spinal pathology has a very long history – the first reports on this subject were published over 100 years ago. Albee and Hibbs were the first to describe spinal fusion in the treatment of spinal deformities [8, 9]. However, at the end of the 1990s, spinal fusion took on a special dimension. It was mainly due to the explosion of stabilizations performed in connection with the introduction of numerous new stabilization systems and increasingly accurate imaging of the pathology thanks to magnetic resonance imaging (MRI). Younger and younger people were also operated on, who could quickly return to professional and physical activity [10–12].
On the one hand, the introduction of internal stabilization into spinal surgery caused the acceleration of the mobilization of patients after operations. However, new problems appeared in connection with that aspect. Rapidly emerging degenerative lesions and instability in adjacent segments became the main problem [13, 14].
Adjacent segment disease (ASD) has no clear definition or classification. Nevertheless, it is used to define and unify degenerative and proliferative lesions in a segment adjacent to an operated and stabilized one [15, 16].
Same-segment disease (SSD) is a condition in which a recurrence of the disease is found in the segment already operated on, and reoperation is required due to the development of degenerative changes and disease recurrence [15, 17].
Both forms of degeneration result from the developing degenerative disease in the adjacent or the same segment, occurring both after spondylodesis and in patients after operations without stabilization. Developing degenerative lesions are the most common reason for problems occurring in patients who have already been operated. After a period of clinical improvement following the surgery, some patients experience recurrence of lumbar and radicular pain, which prompts them to seek help. The surgeon diagnoses the disease and identifies indications for surgical treatment based on clinical examination confirmed with X-ray imaging and magnetic resonance imaging.
We observed a large number of patients who required reoperation. Therefore, it seemed necessary to analyse the underlying causes. However, no explicit answer was found because there is no evidence of the impact of stabilization – especially comprising short segments – on the development of degenerative lesions in the adjacent segments. Our analysis of the cases of lumbar reoperation without the use of stabilization and patients with stabilization was carried out to help us understand whether developing degenerative lesions resulted from stabilization or from natural aging processes.
The aim of the study was to determine whether there is a significant difference in the rate of reoperations due to degenerative disease in patients with spondylodesis using implants and in patients after non-fusion surgery.
Methods
The clinical material included 2194 patients treated surgically due to degenerative disease of the lumbar spine in the Department of Neuro-orthopaedics Rehabilitation Centre in the years 2018–2021. The whole group was divided into 2 categories. Patients after fusion surgery, i.e. those who underwent surgery with spondylodesis using implants, and patients after non-fusion surgery, i.e. those who underwent surgery without the use of stabilization. Patients who were reoperated for degenerative disease were distinguished from the group. Each unplanned subsequent lumbar spine operation was defined as reoperation.
Patients who were operated due to other diseases, i.e. cancer, infection, or after spinal injuries, and patients who underwent reoperation due to loosening or fracture of implants were excluded from the group.
The reoperated patients were divided into three groups: 133 patients operated due to adjacent segment disease (57% women, 43% men, mean age: 63.3 ±10.68 years), 111 patients operated due to the progression of degenerative lesions (43% women, 57% men, mean age: 57.6 ±14.83 years), 88 patients with recurrent intervertebral disc herniation (48% women, 52% men, mean age: 50.2 ±13 years).
Adjacent segment disease was defined as degenerative lesions in the segment of the spine above or below stabilization, which constituted an indication for surgery.
The progression of degenerative lesions was defined as a degeneration of operated segment or other segments in the patients after non-fusion surgery, who needed additional surgical treatment.
Recurrent lumbar disc herniation was defined as the intervertebral disc herniation of a segment that had already been operated.
Patients without improvement after conservative treatment or with the occurrence or exacerbation of neurological deficits were qualified for reoperation. ASD and the progression of degenerative lesions were evaluated on X-ray, MRI, or computed tomography (CT) scan before the first operation and before reoperation. Recurrent intervertebral disc herniation was evaluated on MRI or CT scan.
The results were subjected to statistical analysis. Pearson’s χ2 test was used for the analysis to compare the occurrence of reoperation between groups and gender differentiation between groups. The non-parametric Kruskal-Wallis test was used to compare the age of patients due to the failure to meet the criterion of homogeneity of variance in Levine’s test. The analysis was performed using the R language.
Results
The percentage of patients operated due to adjacent segment disease in the group of patients with stabilization ranged from 7 to 10% and was on average 8.9% (Table I).
Table I
The number and percentage of reoperations due to adjacent segment disease in patients after degenerative disease of the lumbar spine with the use of stabilization in individual half-years in 2018–2021
The rate of reoperations due to the progression of degenerative lesions in the group of patients operated due to degenerative disease without the use of implants was on average 15.9% (Table II).
Table II
The number and percentage of reoperations due to the progression of degenerative lesions in patients without the use of stabilization in individual half-years in 2018–2020
The percentage of recurrent disc herniation in the group of patients operated without the use of implants ranged from 10.5% to 15.8%, with the average of 12.6% (Table III, Figure 1).
Table III
The number and percentage of reoperations due to recurrent disc herniation in individual half-years in 2018–2020
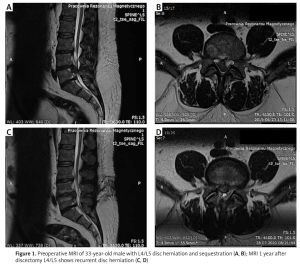
Figure 1
Preoperative MRI of 33-year-old male with L4/L5 disc herniation and sequestration (A, B); MRI 1 year after discectomy L4/L5 shows recurrent disc herniation (C, D)
The rate of reoperations due to recurrent disc herniation and the progression of degenerative lesions in the group of patients without implants ranged from 22.4% to 38% with the average being 28.6% (Table IV).
Table IV
The number and percentage of reoperations in patients without the use of stabilization in individual half-years in 2018–2020
Statistical analysis showed a significant difference between the percentage of reoperations in individual groups of patients (p < 0.00001) in Pearson’s χ2 test (χ2 = 150.8774).
As regards the group of patients without spondylodesis, the rate of reoperations was significantly higher than in the group of patients with spondylodesis, with the average being 28.6% and 8.9%, respectively.
The percentage of patients operated due to adjacent segment disease was significantly lower compared to the rate of reoperations due to the progression of degeneration and recurrent hernia. The respective average values were as follows: 8.9%, 15.9%, and 12.8%.
The rate of reoperations due to recurrent disc herniation was significantly lower than in the case of progression of degeneration.
Statistical analysis showed a significant difference in the age of patients reoperated in individual groups (p < 0.01 in the Kruskal-Wallis test with a post hoc test for multiple comparisons).
Patients reoperated due to recurrent hernia were the youngest, and those with adjacent segment disease were the oldest.
No significant difference was observed as regards the percentage of reoperations depending on sex in Pearson’s χ2 test (p = 0.1495, χ2 = 3.8016).
Discussion
Analysis of reoperation in degenerative spine disease is the subject of numerous publications. The basic question that needs to be answered concerns the impact of spondylodesis on the acceleration of the degenerative process in adjacent segments and whether such changes are caused by the natural disease process or surgical intervention. Spondylodesis is a common procedure that improves the results of treatment and the patient’s functional condition. However, reoperation is necessary in some cases. Adjacent segment disease is a complex and difficult problem, constantly discussed and analysed by spinal surgeons worldwide (Figure 2).
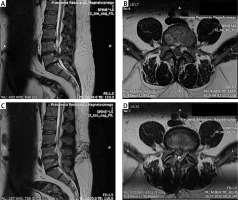
Figure 2
55-year-old female with spondylolisthesis L4/L5 treated with transpedicular stabilization and fusion; 2 years later patient underwent reoperation because of adjacent segment instability L3/L4; transpedicular stabilization was extended with usage rod’s connector. X-rays 1 year after reoperation show subsequent adjacent segment instability L2/L3 (A, B); MRI additionally revealed L2/L3 disc herniation with sequestration (C, D); postoperative X-ray after discectomy L2/L3 and extended transpedicular stabilization (E, F)

The main risk factors of ASD include patient’s age, genetic factors, high body mass index, previous degenerative lesions in the adjacent segment, insufficient lumbar lordosis, and osteoporosis. The influence of surgical technique is also considered, i.e. laminectomy at the level of a segment adjacent to the stabilized one, excessive distraction of the stabilized segment, and stabilization of several segments [5, 18].
In 2020, the Spine Journal published an analysis of 1751 patients. As regards the group, a total of 791 patients underwent spondylodesis, and in 960 patients the mobility of the operated segment was preserved. The adjacent segment degeneration rate on X-ray, the adjacent segment symptomatic disease rate, and the reoperation rate were 27.8%, 7.6%, and 4.6%, respectively. The above results did not reveal a statistical difference in the occurrence of ASD diagnosed based on X-ray, symptomatic ASD, and reoperation due to ASD in the group of patients with and without stabilization of the operated segment [17].
The analysis published by Wang et al. in 2017 showed no statistical difference in the occurrence of adjacent segment disease, regardless of whether the group of patients had initially undergone fusion surgery or non-fusion [3].
A study conducted by Zhang et al. included 4206 patients. The authors reported the annual degeneration rate of the adjacent segment of 5.9%, and the occurrence of adjacent segment disease of 1.8% per year. In addition, the degeneration rate of the adjacent segment increased with the number of segments that were stabilized. The study reported no influence of age, sex, and stabilization methods on the increase in the risk of adjacent segment disease [7].
The highest risk of ASD development was observed in patients originally operated due to degenerative spondylolisthesis [19].
Conversely, other authors reported that the rate of reoperation after spondylodesis was higher compared to operations preserving the mobility of the operated segment. According to Malter, the rate of reoperations within 5 years was higher in patients who were stabilized than in patients without spondylodesis (18% vs. 15%, respectively) [20].
Hwang et al. reported that the rate of reoperations was 16.3% in patients who had undergone micro-decompression (laminotomy) due to lumbar stenosis. The authors concluded that moderate degeneration of the intervertebral disc in the lower lumbar segments was a risk factor for intervertebral disc herniation or spinal stenosis requiring reoperation after micro-decompression in lumbar stenosis [21]. A high rate of reoperations after discectomy was also reported in the literature, and recurrent intervertebral disc hernia was the most common cause of reoperation after microdiscectomy. Siccoli et al. studied a group of 3013 patients who underwent tubular microdiscectomy due to lumbar disc herniation and reported that 166 (5.5%) were reoperated for recurrent disc herniation [22].
A 2-year follow-up of 119 patients who had undergone L4-L5 discectomy for disc herniation showed that 21 (17.6%) patients required a reoperation for recurrent disc herniation, and the average time between operations was 17.6 ±21.1 months [23]. Yaman et al. reported an even higher rate of reoperations due to recurrent disc herniation after L4-L5 discectomy, i.e. 24.7% [24]. The rate of reoperations 5 years after discectomy was 13.4% according to Kim et al., while Heindel et al. claimed that it was 12.2% after 4 years [25, 26].
A study conducted in a group of 751 patients who had undergone single-level discectomy without spondylodesis in the years 1990–2012 showed that the total rate of reoperations due to degeneration was 10.79%, including a rate of reoperations in the adjacent segment of 4% [27].
The analysis presented by us is based on just a few years of assessment of the treatment of patients. However, it is also based on over 20 years of experience in the treatment of spinal disorders in the course of degenerative lesions without primary stabilization and with the use of transpedicular stabilization. The presented clinical material includes not only patients reoperated in the years 2018–2021, but it also encompasses the entire group of patients who had been initially operated in previous years. It was demonstrated that patients who underwent reoperation without prior spondylodesis constituted a significantly larger group than patients with spondylodesis.
In the literature there are plenty of publications showing that the reoperation rate was higher in patients after non-fusion surgery in comparison with patients after spondylodesis with the use of implants [7, 17, 22–26]. The following causes of reoperation after decompression without fusion can be listed: instability induced by the decompression and facet resection, insufficient decompression, and recurrent disc herniation. A recent review showed that 1.6–32.0% of patients developed postoperative symptomatic spondylolisthesis after decompression surgery. Insufficient discectomy or the decompression of neural structures may result in recurrent disc herniation or persistent stenosis [28–30].
Our study and literature review demonstrated that stabilization does not exert a significant impact on the increase in the number of reoperations. However, a lower percentage of reoperations due to degenerative disease in the group of patients with stabilization compared to those without stabilization indicated that adjacent segment disease might result from the progression of degenerative lesions associated with body ageing. Based on the analysis, it may be stated that the indications should not be limited to performing spondylodesis when planning operative treatment in patients with spinal degenerative disease. We observed multiple cases of instability of the operated segment due to surgeries involving the decompression of neural structures. In many spinal disorders there is a need for facet resection to precisely decompress neural structures, which leads to instability in the future. The surgical decompression of neural structures may also be insufficient, which contributes to persistent medical problems. The degenerative lesions of the adjacent segment in patients with spondylodesis were also observed in operated patients without spondylodesis (Figure 3).
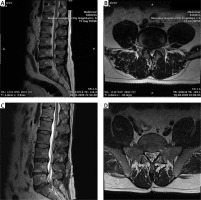
Figure 3
MRI of 30-year-old male suffering from severe low back pain and radicular pain presents L4/L5 disc herniation (A, B); MRI 2 years after discectomy L4/L5, due to recurrent lumbar and radicular pain, revealed adjacent segment L5/S1 disc herniation (C, D)
Surgical treatment of spondylolisthesis and instability is an unquestionable indication for performing spondylodesis. Indications for stabilizing or preserving the mobility of the operated segment should provide for the nature of the lesions, and anatomical and surgical conditions.
The present paper showed that the number of reoperations was significantly higher in a group of patients without spondylodesis compared to those with spondylodesis.
In conclusion, based on the presented analysis, it may be claimed that spondylodesis performed with the use of implants contributes to a reduction in the number of reoperations necessary in selected conditions. The lowest percentage of reoperations performed due to adjacent segment disease compared to other indications for reoperation showed that it was not the most important problem in spinal surgery.