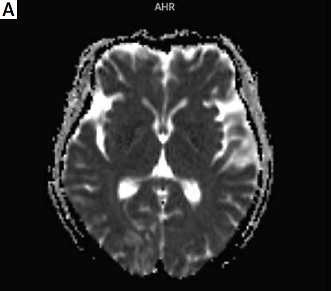
The patient was a 58-year-old female with a thin build who was admitted to the hospital with swollen and hardened skin for 2 years and convulsions with impaired consciousness for 5 h. She had a 2-year history of diffuse cutaneous systemic sclerosis (SSc) with regular hospital review and maintenance treatment with methylprednisolone 8 mg QD. She had no history of hypertension with a baseline blood pressure of 100/75 mm Hg, a baseline creatinine value of 49 μmmol/l, and a body mass index (BMI) of 18.2 kg/m2 before admission. On examination, she presented with transient extremity twitches, normal post-episode extremity muscle strength and tone, and negative bilateral pathological signs; thickened skin on the face and the back of both hands and wrists – sclerodactyly. Laboratory tests showed elevated lactate dehydrogenase (486 IU/l), anemia (HB: 107 g/l), and perfect urine routine suggesting positive urine protein (++) and urine occult blood (+). Blood pressure accelerated to 157/100 mm Hg (new-onset hypertension) over a short period, while serum creatinine rose to 85 μmmo/l (more than a 50%/two-fold increase from baseline). The cranial magnetic resonance imaging (MRI) showed patchy abnormal signal foci in the right frontal lobe, right occipital lobe, and bilateral parietal lobes, and the diagnosis requires consideration of posterior reversible encephalopathy syndrome (Figures 1 A-C). The head computed tomography (CT) revealed no hemorrhage or occupancy, and no other evidence of neurological damage was found, including intracranial infection, cerebrovascular disease, electrolyte balance disorders, craniocerebral trauma, exogenous poisoning, metabolic disease, and hypoglycemia. The initial diagnosis was considered early scleroderma renal crisis with secondary posterior reversible encephalopathy syndrome [1, 2]. The treatment was initiated with an angiotensin-converting enzyme inhibitor (ACEI) against hypertension and methylprednisolone 6 mg QD for the primary condition, supplemented by treatment of seizures to make significant improvements in convulsion symptoms. Serum creatinine decreased to 48 μmol/l on recheck and blood pressure gradually decreased to normal. Repeat cranial MRI showed that the original intracranial patchy abnormal signal foci were absorbed than before (Figures 1 D-F).
Figure 1
A–C – The cranial magnetic resonance imaging showed patchy abnormal signal foci in the right frontal lobe, right occipital lobe, and bilateral parietal lobes. D–F – Repeat cranial magnetic resonance imaging showed that the original intracranial patchy abnormal signal foci were absorbed than before

Posterior reversible encephalopathy syndrome, a group of rare neuroimaging syndromes with acute or subacute onset, mainly manifested as headache, dizziness, nausea, vomiting, seizure, visual abnormality, consciousness impairment and disturbance of mental behavior [3]. The typical imaging findings of posterior reversible encephalopathy syndrome are reversible and symmetric lesions in white matter of the posterior brain areas. There are no specific diagnostic criteria for posterior reversible encephalopathy syndrome, and in certain clinical situations (especially hypertension, renal disease, immunosuppressive therapy), patients presenting with acute onset neurological symptoms such as headache, visual abnormalities, impaired consciousness and seizures, and with characteristic imaging changes on MRI of the head, should be highly suspicious of posterior reversible encephalopathy syndrome when other possible diseases are excluded [3]. Scleroderma renal crisis is a rare and serious complication of SSc characterized by sudden onset of hypertension and acute kidney injury, manifested by elevated blood pressure, elevated plasma renin levels and progressive rise in serum creatinine, which may be accompanied by headache, malaise, encephalopathy and pulmonary edema, microvascular hemolytic anemia, and thrombocytopenia [4]. The patient had an underlying history of diffuse cutaneous SSc and was on long-term hormone therapy, with a short-term increase in blood pressure from baseline normal to hypertension grade I, accompanied by a more than 50%/two-fold increase in serum creatinine values from baseline, with urinary protein (++) and urinary occult blood (+), and an improvement in blood pressure and serum creatinine from before after treatment with ACEI. Although no renal puncture biopsy was performed, scleroderma renal crisis was a comprehensive diagnosis based on clinical and laboratory findings. Fa’ak reported a 73-year-old female patient with scleroderma who developed posterior reversible encephalopathy syndrome induced by scleroderma renal crisis [5]. Chen described a 36-year-old man with diffuse cutaneous SSc who developed scleroderma renal crisis and acute chronic renal failure, ultimately requiring maintenance hemodialysis [6]. However, the coexistence of these two diseases has rarely been described.
The core mechanism of posterior reversible encephalopathy syndrome due to scleroderma renal crisis may be that the sudden rise in blood pressure breaks the cerebrovascular autoregulation and causes vascular endothelial cell damage, resulting in blood-cerebrospinal fluid barrier disruption, increased vascular permeability and vasogenic edema [7]. Studies have shown that scleroderma renal crisis can occur in 10–15% of patients with SSc, and predisposing factors include diffuse cutaneous SSc with extensive progressive cutaneous involvement and positive anti-RNA polymerase I and III autoantibodies, and long-term hormone use [8]. Hormones can trigger or exacerbate SRC, and it is important to weigh the pros and cons of this strategy. In this case, the patient reduced the dosage after the onset of the disease. Although SSc involving the peripheral nervous system is common, regardless of creatinine levels, a diagnosis of scleroderma renal crisis should be considered when a patient presents with sudden onset of central nervous system symptoms in the setting of abnormal renal function and rapidly developing hypertension over a short period of time and may be diagnosed with a combination of secondary posterior reversible encephalopathy syndrome in conjunction with characteristic imaging findings.