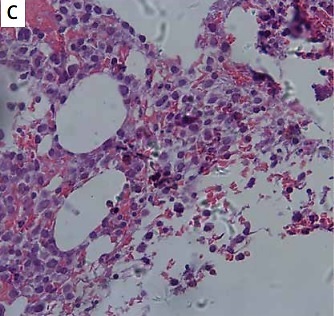
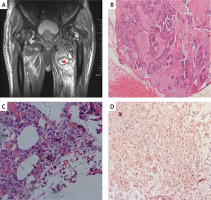
A 74-year-old man with a history of hypertension presented to the rheumatology department with polyarticular swelling and tenderness, followed by progressive pain in the hip. Physical examination revealed stiffness of the joints of both hands in a fixed position with limited joint motion. Ultrasound of the hand joints showed symmetric synovitis with bone erosion involving the proximal interphalangeal joints, metacarpophalangeal joints, and wrist joints. Subsequent magnetic resonance imaging of the hip revealed a swollen mass of soft tissue around the right hip joint, measuring approximately 16 × 16 × 10 cm, along with severe synovial hyperplasia in both hips (Figure 1 A). Histopathological examination showed massive amyloid deposition and calcification (Figure 1 B, Congo red staining), along with massive synovial cell proliferation and inflammatory cell infiltration (Figure 1 C, Crystal violet staining), and immunohistochemistry showed positivity for λ chains (Figure 1 D). Laboratory tests were negative for rheumatoid factor, anti-citrullinated protein antibody, antinuclear antibodies, ANCA, HLA-B27; hemoglobin was 80 g/l, blood calcium 3.11 mmol/l, serum creatinine 322 µmol/l, serum β2-microglobulin 13943.7 ng/ml, urine protein was 5.85 g/day. Inflammatory indicators showed that erythrocyte sedimentation rate of 60 mm/h and C-reactive protein of 43.2 mg/l.
Figure 1
A – Magnetic resonance imaging of the hip revealed a swollen mass of soft tissue around the right hip joint, measuring approximately 16 × 16 × 10 cm, along with severe synovial hyperplasia in both hips. Histopathological examination showed massive amyloid deposition and calcification (B, Congo red staining), along with massive synovial cell proliferation and inflammatory cell infiltration (C, Crystal violet staining), and immunohistochemistry showed positivity for λ chains (D)
Serum immunofixation electrophoresis showed that IgG-λ M-type protein accounted for 14.9%, and urine λ light chain concentration of 585 mg/l (κ light chain 23.8 mg/l), and peripheral blood λ free light chain concentration > 1470 mg/l (κ free light chain 182 mg/l). Bone marrow aspiration revealed plasma cells comprising 51% of the cells, and immunophenotyping indicated that these cells were clonal plasma cells. A diagnosis of multiple myeloma (IgG-λ type D-S stage IIIB)-associated amyloid arthropathy (MAA) was made with seronegative rheumatoid arthritis at the first presentation. At the 6-month follow-up, the patient received chemotherapy in the hematology department and experienced a reduction in symptoms.
Approximately 20% of multiple myeloma cases can be associated with immunoglobulin light chain amyloidosis. Of these, 3.7–9.2% of patients have immunoglobulin light chain amyloidosis involving the joints, leading to multiple myeloma-associated amyloid arthropathy [1–4], a rare complication of multiple myeloma with mechanisms related to light chain amyloid deposition. A systematic review revealed that of 101 patients with amyloid arthropathy associated with multiple myeloma, 63 presented with arthritis prior to the diagnosis of multiple myeloma, 33 of which were initially misdiagnosed as RA [5]. There were 72 cases of polyarthritis, 17 of oligoarthritis, and 3 of monoarthritis. The shoulder joint was most frequently involved, followed by the knees and small hand joints [5]. Multiple myeloma-associated amyloid arthropathy mainly presents as symmetrical rheumatoid factor-negative nonerosive symmetric polyarthritis and is easily confused with rheumatoid arthritis [6]. Studies have shown that multiple myeloma-associated amyloid arthropathy usually has a relatively bland synovitis, with a few presenting with massive synovial inflammation. It is helpful to distinguish RA from multiple myeloma-associated amyloid arthropathy in synovial biopsies, for example, by finding synovial plasma cells, which are a common feature of RA. The absence of plasma cells in synovial biopsies should raise a suspicion of multiple myeloma-associated amyloid arthropathy [5]. Previous studies have shown that multiple myeloma and amyloid bone lesions can be complicated in patients with seropositive rheumatoid arthritis [7]. This case was seronegative rheumatoid arthritis and met the diagnostic criteria for rheumatoid arthritis [8]. More importantly, this case brings to light the fact that rheumatoid arthritis can be the first presentation in patients with multiple myeloma-associated amyloid arthropathy, which has not been previously described in the literature, and highlights the diagnostic value of magnetic resonance imaging, histopathology, and immunofixation electrophoresis in the field of rheumatology. Future studies are necessary to investigate the variability of clinical features between multiple myeloma-associated amyloid arthropathy with seronegative or seropositive rheumatoid arthritis and multiple myeloma-associated amyloid arthropathy with or without combined rheumatoid arthritis.