Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
CLINICAL RESEARCH
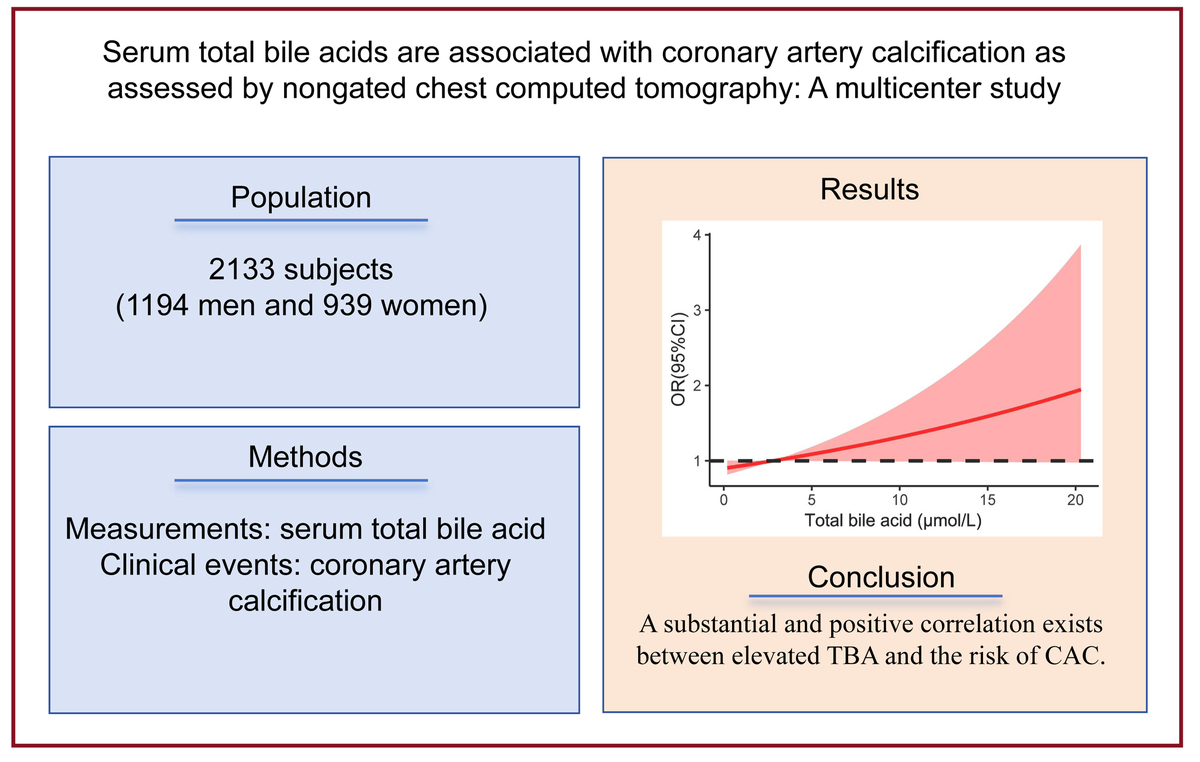
Serum total bile acids are associated with coronary artery calcification as assessed by non gated chest computed tomography: a multicenter study
1
Department of Cardiovascular Medicine, Hospital affiliated with Nanjing University of Chinese Medicine, Nanjing, China
2
Department of Radiology, Hospital affiliated with Nanjing University of Chinese Medicine, Nanjing, China
3
Emergency and Critical Care Medicine Department, Nanjing Medical University’s Affiliated Suzhou Hospital, Suzhou, China
4
Changhai Hospital, Naval Medical University, Shanghai, China
These authors had equal contribution to this work
Submission date: 2025-07-14
Final revision date: 2025-10-28
Acceptance date: 2025-12-23
Online publication date: 2026-01-20
Corresponding author
Xiao Chen
Department of Radiology Affiliated Hospital of Nanjing University of Chinese Medicine Nanjing 210029, China
Department of Radiology Affiliated Hospital of Nanjing University of Chinese Medicine Nanjing 210029, China
Ddongling Lv
Department of Cardiovascular Medicine Affiliated Hospital of Nanjing University of Chinese Medicine Nanjing 210029 China
Department of Cardiovascular Medicine Affiliated Hospital of Nanjing University of Chinese Medicine Nanjing 210029 China
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Coronary artery calcification (CAC) is a risk factor for cardiovascular disease (CVD). The association between serum total bile acid (TBA) concentration and CAC has not been investigated, even though bile acid may act as a mediator between gut microbiota and CVD. We examined this relationship in a general Chinese population.
Material and methods:
This cross-sectional study included 2133 people who underwent computed tomography (CT) scans for lung cancer screening between 2018 and 2020. Information on medical history, laboratory test results, and demographics was collected from medical records. CAC was assessed on non-gated chest CT images. Multivariable logistic regression analysis and restricted triple spline analysis were applied to examine the correlation between TBA and CAC risk.
Results:
CACs were detected in 426 of 2133 participants. Participants with higher TBA concentrations had a considerably higher prevalence of CAC (33.4% in the fourth quartile and 11.5% in the first quartile, p < 0.001). TBA was closely associated with CAC, as determined by multivariable logistic regression analysis (OR = 1.05, 95% CI: 1.00–1.10). The fourth TBA quartile was significantly associated with a high incidence of CAC in the general population (OR = 1.76, 95% CI: 1.02–3.06), in older adults (OR = 1.66, 95% CI: 1.03–2.68), and in subjects without diabetes (OR = 1.62, 95% CI: 1.07–2.45) or hypertension (OR = 1.74, 95% CI: 1.16–2.63) when compared to the first TBA quartile.
Conclusions:
A substantial and positive correlation was found between elevated TBA and CAC. The causal relationship between TBA and CAC risk should be investigated in longitudinal studies.
Coronary artery calcification (CAC) is a risk factor for cardiovascular disease (CVD). The association between serum total bile acid (TBA) concentration and CAC has not been investigated, even though bile acid may act as a mediator between gut microbiota and CVD. We examined this relationship in a general Chinese population.
Material and methods:
This cross-sectional study included 2133 people who underwent computed tomography (CT) scans for lung cancer screening between 2018 and 2020. Information on medical history, laboratory test results, and demographics was collected from medical records. CAC was assessed on non-gated chest CT images. Multivariable logistic regression analysis and restricted triple spline analysis were applied to examine the correlation between TBA and CAC risk.
Results:
CACs were detected in 426 of 2133 participants. Participants with higher TBA concentrations had a considerably higher prevalence of CAC (33.4% in the fourth quartile and 11.5% in the first quartile, p < 0.001). TBA was closely associated with CAC, as determined by multivariable logistic regression analysis (OR = 1.05, 95% CI: 1.00–1.10). The fourth TBA quartile was significantly associated with a high incidence of CAC in the general population (OR = 1.76, 95% CI: 1.02–3.06), in older adults (OR = 1.66, 95% CI: 1.03–2.68), and in subjects without diabetes (OR = 1.62, 95% CI: 1.07–2.45) or hypertension (OR = 1.74, 95% CI: 1.16–2.63) when compared to the first TBA quartile.
Conclusions:
A substantial and positive correlation was found between elevated TBA and CAC. The causal relationship between TBA and CAC risk should be investigated in longitudinal studies.
REFERENCES (51)
1.
Herrmann M, Rodriguez-Blanco G, Balasso M, et al. The role of bile acid metabolism in bone and muscle: from analytics to mechanisms. Crit Rev Clin Lab Sci 2024; 61: 510-28.
2.
Zhang Z, Lv T, Wang X, et al. Role of the microbiota-gut-heart axis between bile acids and cardiovascular disease. Biomed Pharmacother 2024; 174: 116567.
3.
Rodríguez-Morató J, Matthan NR. Nutrition and gastrointestinal microbiota, microbial-derived secondary bile acids, and cardiovascular disease. Curr Atheroscler Rep 2020; 22: 47.
4.
Voiosu A, Wiese S, Voiosu T, Bendtsen F, Møller S. Bile acids and cardiovascular function in cirrhosis. Liver Int 2017; 37: 1420-30.
5.
Charach L, Charach G, Karniel E, et al. Peripheral vascular disease and carotid artery disease are associated with decreased bile acid excretion. Bioengineering 2023; 10: 935.
6.
Jia B, Zou Y, Han X, Bae JW, Jeon CO. Gut microbiome-mediated mechanisms for reducing cholesterol levels: implications for ameliorating cardiovascular disease. Trends Microbiol 2023; 31: 76-91.
7.
Li H, Xu G, Shang Q, et al. Inhibition of ileal bile acid transport lowers plasma cholesterol levels by inactivating hepatic farnesoid X receptor and stimulating cholesterol 7 alpha-hydroxylase. Metabolism 2004; 53: 927-32.
8.
Gylling H, Hallikainen M, Rajaratnam RA, et al. The metabolism of plant sterols is disturbed in postmenopausal women with coronary artery disease. Metabolism 2009; 58: 401-7.
9.
Morozova S, Suc-Royer I, Auwerx J. Cholesterol metabolism modulators in future drug therapy for atherosclerosis. Med Sci (Paris) 2005; 21 Spec No: 53-8.
10.
Witkowski M, Weeks TL, Hazen SL. Gut microbiota and cardiovascular disease. Circ Res 2020; 127: 553-70.
11.
Qian B, Zhang K, Li Y, Sun K. Update on gut microbiota in cardiovascular diseases. Front Cell Infect Microbiol 2022; 12:1059349.
12.
Mori H, Torii S, Kutyna M, Sakamoto A, Finn AV, Virmani R. Coronary artery calcification and its progression: what does it mean? JACC Cardiovasc Imaging 2018; 11: 127-42.
13.
Chen J, Budoff MJ, Reilly MP, et al. Coronary artery calcification and risk of cardiovascular disease and death among patients with chronic kidney disease. JAMA Cardiol 2017; 2: 635-43.
14.
Madhavan MV, Tarigopula M, Mintz GS, Maehara A, Stone GW, Généreux P. Coronary artery calcification: pathogenesis and prognostic implications. J Am Coll Cardiol 2014; 63: 1703-14.
15.
Mehta A, Vasquez N, Ayers CR, et al. Independent association of lipoprotein(a) and coronary artery calcification with atherosclerotic cardiovascular risk. J Am Coll Cardiol 2022; 79: 757-68.
16.
Zhang W, Jin J, Zhang H, et al. The value of HDL subfractions in predicting cardiovascular outcomes in untreated, diabetic patients with stable coronary artery disease: an age- and gender-matched case-control study. Front Endocrinol (Lausanne) 2022; 13:1041555.
17.
Wang J, Huang X, Fu C, Sheng Q, Liu P. Association between triglyceride glucose index, coronary artery calcification and multivessel coronary disease in Chinese patients with acute coronary syndrome. Cardiovasc Diabetol 2022; 21: 187.
18.
Wang B, Hua J, Ma L. Triglyceride to high-density lipoprotein ratio can predict coronary artery calcification. Pak J Med Sci 2022; 38: 624-631.
19.
Santangelo G, Gherbesi E, Donisi L, et al.Imaging approaches in risk stratification of patients with coronary artery disease: a narrative review. Arch Med Sci 2024; 21: 16-31.
20.
Yong Y, Giovannucci J, Pang SN, et al. Coronary artery calcium density and risk of cardiovascular events: a systematic review and meta-analysis. JACC Cardiovasc Imaging 2025; 18: 294-304.
21.
Suzuki Y, Matsumoto N, Yoda S, Amano Y, Okumura Y. Coronary artery calcium score: current status of clinical application and how to handle the results. J Cardiol 2022; 79: 567-71.
22.
Christensen JL, Sharma E, Gorvitovskaia A, et, al. Impact of slice thickness on the predictive value of lung cancer screening computed tomography in the evaluation of coronary artery calcification. J Am Heart Assoc 2019; 8: e010110.
23.
Xie X, Zhao Y, de Bock GH, et al. Validation and prognosis of coronary artery calcium scoring in nontriggered thoracic computed tomography: systematic review and meta-analysis. Circ Cardiovasc Imaging 2023; 6: 514-21.
24.
Rahoual G, Zeitouni M, Charpentier E, et al. Phenotyping coronary plaque by computed tomography in premature coronary artery disease. Eur Heart J Cardiovasc Imaging 2024; 25: 257-66.
25.
Rasmussen T, Køber L, Abdulla J, et al. Coronary artery calcification detected in lung cancer screening predicts cardiovascular death. Scand Cardiovasc J 2015; 49: 159-67.
26.
Chiang JYL, Ferrell JM, Wu Y, Boehme S. Bile acid and cholesterol metabolism in atherosclerotic cardiovascular disease and therapy. Cardiol Plus 2020; 5: 159-70.
27.
Charach G, Karniel E, Novikov I, et al. Reduced bile acid excretion is an independent risk factor for stroke and mortality: a prospective follow-up study. Atherosclerosis 2020; 293: 79-85.
28.
Li W, Shu S, Cheng L, et al. Fasting serum total bile acid level is associated with coronary artery disease, myocardial infarction, and severity of coronary lesions. Atherosclerosis 2020; 292: 193-200.
29.
Zhang BC, Chen JH, Xiang CH, Su MY, Zhang XS, Ma YF. Increased serum bile acid level is associated with high-risk coronary artery plaques in an asymptomatic population detected by coronary computed tomography angiography. J Thorac Dis 2019; 11: 5063-70.
30.
Wang C, Ma Q, Yu X. Bile acid network and vascular calcification-associated diseases: unraveling the intricate connections and therapeutic potential. Clin Interv Aging 2023; 18: 1749-67.
31.
Tong Y, Wang Y, Chen X, et al. The triglyceride glucose: high-density lipoprotein cholesterol ratio is associated with coronary artery calcification evaluated via non-gated chest CT. Cardiovasc Diabetol 2024; 23: 376.
32.
Yamamoto S, Sato I, Fukuhama N, et al. Bile acids aggravate nonalcoholic steatohepatitis and cardiovascular disease in SHRSP5/Dmcr rat model. Exp Mol Pathol 2020; 114: 104437.
33.
Charach G, Argov O, Geiger K, Charach L, Rogowski O, Grosskopf I. Diminished bile acids excretion is a risk factor for coronary artery disease: 20-year follow up and long-term outcome. Therap Adv Gastroenterol 2018; 11: 1756283x17743420.
34.
Jovanovich A, Isakova T, Block G, et al. Deoxycholic acid, a metabolite of circulating bile acids, and coronary artery vascular calcification in CKD. Am J Kidney Dis 2018; 71: 27-34.
35.
Jovanovich A, Cai X, Frazier R, et al. Deoxycholic acid and coronary artery calcification in the chronic renal insufficiency cohort. J Am Heart Assoc 2022; 11: e022891.
36.
Chong Nguyen C, Duboc D, Rainteau D, et al. Circulating bile acids concentration is predictive of coronary artery disease in human. Sci Rep 2021; 11: 22661.
37.
Guan B, Tong J, Hao H, et al. Bile acid coordinates microbiota homeostasis and systemic immunometabolism in cardiometabolic diseases. Acta Pharm Sin B 2022; 12: 2129-49.
38.
Jiang Z, Zhuo LB, He Y, et al. The gut microbiota-bile acid axis links the positive association between chronic insomnia and cardiometabolic diseases. Nat Commun 2022; 13: 3002.
39.
Ridlon JM, Harris SC, Bhowmik S, Kang DJ, Hylemon PB. Consequences of bile salt biotransformations by intestinal bacteria. Gut Microbes 2016; 7: 22-39.
40.
Hanafi NI, Mohamed AS, Sheikh Abdul Kadir SH, Othman MHD. Overview of bile acids signaling and perspective on the signal of ursodeoxycholic acid, the most hydrophilic bile acid, in the heart. Biomolecules 2018; 8: 159.
41.
Li Q, Li Y, Lei C, Tan Y, Yi G. Sphingosine-1-phosphate receptor 3 signaling. Clin Chim Acta 2021; 519: 32-9.
42.
Bishop-Bailey D, Walsh DT, Warner TD. Expression and activation of the farnesoid X receptor in the vasculature. Proc Natl Acad Sci USA 2004; 101: 3668-73.
43.
Yu H, Nie R, Shen C. The role of bile acids in regulating glucose and lipid metabolism. Endocr J 2023; 70: 359-74.
44.
Ding L, Yang L, Wang Z, Huang W. Bile acid nuclear receptor FXR and digestive system diseases. Acta Pharm Sin B 2015; 5: 135-44.
45.
Jonsson AL, Bäckhed F. Role of gut microbiota in atherosclerosis. Nat Rev Cardiol 2017; 14: 79-87.
46.
Lu Q, Chen J, Jiang L, et al. Gut microbiota-derived secondary bile acids, bile acids receptor polymorphisms, and risk of cardiovascular disease in individuals with newly diagnosed type 2 diabetes: a cohort study. Am J Clin Nutr 2024; 119: 324-32.
47.
Sanchez-Gimenez R, Ahmed-Khodja W, Molina Y, et al. Gut microbiota-derived metabolites and cardiovascular disease risk: a systematic review of prospective cohort studies. Nutrients 2022; 14: 2654.
48.
Xu J, Wang N, Yang L, Zhong J, Chen M. Intestinal flora and bile acid interactions impact the progression of diabetic kidney disease. Front Endocrinol 2024; 15: 1441415.
49.
Ramírez-Pérez O, Cruz-Ramón V, Chinchilla-López P, Méndez-Sánchez N. The role of the gut microbiota in bile acid metabolism. Ann Hepatol 2017; 16 (Suppl. 1: s3-105.): s15-20.
50.
Ferraro E, Pozhidaeva L, Pitcher DS, et al. Prolonged ursodeoxycholic acid administration reduces acute ischaemia-induced arrhythmias in adult rat hearts. Sci Rep 2020; 10: 15284.
51.
Christensen JL, Sharma E, Gorvitovskaia A, et al. Impact of slice thickness on the predictive value of lung cancer screening computed tomography in the evaluation of coronary artery calcification. J Am Heart Assoc 2019; 8: e010110.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.