Left ventricular assist device (LVAD) therapy as a treatment option for heart failure (HF) has significantly improved patients’ overall performance and prognosis, requiring re-evaluation of postoperative care protocols, particularly in the field of cardiac rehabilitation [1]. In patients with advanced HF, the use of LVAD significantly improves survival, functional capacity and quality of life [2]. Rehabilitation of LVAD patients is more complex. Under physiological conditions, cardiac output (CO) depends on the heart rate (HR). Stroke volume (SV) is generated by the left ventricle. The presence of LVAD ensures CO production and unloads the failing left ventricle. Pump flow depends on the activity of the pump motor, its rotational speed and the characteristics of the LVAD itself, as well as the preload and afterload of the heart [3]. Additionally, the contractility of the native heart also contributes to the generation of cardiac output, especially during exercise [4, 5]. The HR does not influence LVAD flow rate [6]. The role of early hospital rehabilitation in shaping exercise tolerance and functional capacity among LVAD recipients has been studied [7]. The rehabilitation should be implemented relatively quickly if the clinical and hemodynamic condition of the patient and the proper functioning of the LVAD pump allow this [7, 8]. However, there are no guidelines regarding the optimal time and methods of rehabilitation in this group of patients. The aim of the study was to evaluate the impact of comprehensive hospital rehabilitation on exercise tolerance, muscle strength and team coordination in patients after LVAD implantation.
Methods
Eligible patients were enrolled in the study between February 2019 and December 2021 after giving informed consent. They were discharged from the cardiac surgery department and referred to the rehabilitation ward for a 4–5 weeks’ stay. Training took place 6 times a week and lasted for 60 min. The rehabilitation program consisted of: endurance training, general fitness exercises (dynamic, stretching, coordination, balance) with elements of resistance exercises. Interval endurance training on cycle ergometer loads was determined according to cardiopulmonary exercise test (CPET) results. ECG and saturation were monitored. The rehabilitation department had contact with the attending physician and the emergency department. The training was interrupted if the patient experienced excessive fatigue, shortness of breath, chest pains, arrhythmia, headaches, as well as if the device alarm signals and sudden changes in pump parameters occurred. Before the start of rehabilitation (study 1) and after its completion (study 2), all patients underwent: 1) cardiopulmonary exercise testing (CPET, peak VO2, peak VO2%, VE/VCO2 slope, load, Borg scale evaluation); 2) 6-minute walking test (6-MWT); 3) testing of the grip strength of the right and left hands (kilograms); 4) lower limb muscle strength test – sit to stand test within 30 s; 5) the test assessing complex coordination and the risk of falling (Up&Go test) and 6) Fall Skip test used to assess the risk of falls. Patients’ risk of falls was determined based on the results obtained for each component. All patients had regular psychological support. The study was supported by the State Committee for Scientific Research grant (STRATEGMED2/266798/15/NCBIR/2015). Bioethical Committee approval was issued on April 2, 2019 (IK-NPIA-0021-55/1784/2019).
Statistical analysis
Numerical variables were expressed as mean and standard deviation (SD) or median and 25th – 75th percentiles [Q1–Q3], as appropriate, and categorical variables were expressed as counts and percentages. The normality of distribution was verified using the Shapiro-Wilk test. For normally distributed continuous variables for changes over time, the paired Student’s t-test was used. For data violating a normal distribution, the Wilcoxon’s signed-rank test (for changes over time) was used. The strength of linear relationships between the studied variables was assessed with the Pearson or Spearman correlation coefficient, as appropriate. In all analyses, the tests were two-sided and the level of significance was set at 0.05. Statistical analyses were performed using SAS ver. 9.4 software (SAS Institute Inc, , NC, Durham, USA).
Results
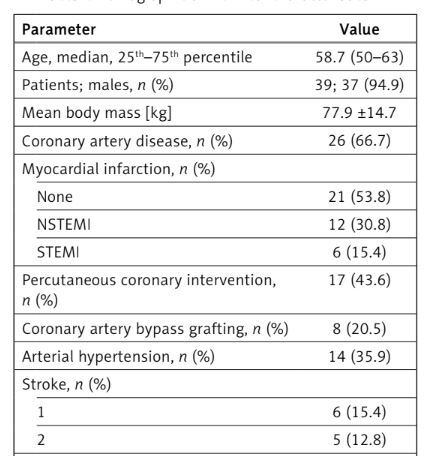
The study comprised 39 patients (37 males, 2 females) aged 58.7, median, (50–63), after LVAD implantation. Demographic and clinical characteristics are presented in Table I. A significant increase in the loads used during endurance training was observed in study 2 vs. 1: 45.6 ±16.1 vs. 26.1 ±8.8 watts, p < 0.001. Significant functional improvement occurred in study 2 vs. 1: 30-second chair stand test: 11.7 (4.2) vs. 9.0 (3.5) number of stands, p < 0.001; Up&Go test: 7.6 (6.6, 8.9) vs. 9.1 (7.6, 10.5) s, p < 0.001; left hand grip strength test: 32.1 (8.1) vs. 30.3 (8.2) kg, p = 0.006; right hand grip strength test: 33.5 (8.8) kg vs. 31.9 (8.7), p = 0.008. The parameters of the Fall Skip test did not change, except for the deflection of the center of gravity during walking, which improved significantly (Table II). An improvement in physical performance was observed after completion of rehabilitation: peakVO2: 13.6 (3.2) vs. 11.9 (3.1) ml/kg/min, p < 0.001, and 6-MWT: 420 (107) vs. 323 (105) m, p < 0.001 (Table II). No significant relationships were found between the number of training sessions, resting and exercise heart rate and parameters tested in functional and exercise tests. Only the improvement in the exercise test measured in watts influenced the results of the walking tests and the improvement in peakVO2.
Table I
Demographic and clinical characteristics
Table II
Results obtained in functional, 6-minute walking tests and ergo-spirometry tests before (study 1) and after rehabilitation (study 2) in the study group
Discussion
The main finding of our study is that multimodal, hospital cardiac rehabilitation is safe and has significant benefits in improving exercise tolerance, muscle strength, and complex coordination in patients after LVAD implantation. There were no adverse events related to the function of the implanted LVAD or the rehabilitation process. We suggest early initiation of rehabilitation. Immediately after discharge from the cardiac surgery department, interval training on an ergometer and general fitness exercises with elements of resistance training may begin. We used standard measures such as HR, 6-MWT and CPET for monitoring the progress of endurance training. After the training period, significant differences were observed in the loads (measured in watts), but not in the level of perceived fatigue measured by the Borg scale [9]. The lack of changes in training HR is attributed to chronotropic incompetence and does not have a significant impact on the flows in the LVAD [10]. After completing the program, there was a significant improvement in physical endurance, confirmed by the results of the CPET and 6-MWT. Previous studies have documented increases in distances in 6-MWT after training [11, 12]. Peak VO2 levels observed both before and after the intervention appear to be lower compared to data reported in other studies, in which the median peak VO2 level at baseline was 13 ml/kg/min and increased to 17 ml/kg/min after the rehabilitation cycle within 3–6 months of follow-up [13]. Our results confirm data presented in the previous studies [14, 15]. Potential explanation for the decreased oxygen consumption noted in the present study may be the relatively short period between LVAD implantation and further evaluation. Another factor may be the specific type of LVAD used (third-generation CF) as in the previous studies older generation LVADs were used in patients. In our study, we utilized the 25 HeartMate 3 (HM3) and 14 HeartWare (HW) LVADs, with an average time from implantation to evaluation of 42.6 days prior to rehabilitation [14, 15]. An important aspect in patients with HF and LVAD is the improvement of muscle strength, because patients with long-term HF often suffer from weakening of muscle function as a result of progressive malnutrition [1, 2, 7]. However, to design effective strength training regimens, a comprehensive evaluation of muscle strength in this patient group is necessary. We have also observed significant improvement in functional capacity and changes between the initial and final parameters in the tests assessing comprehensive coordination and the risk of falls, which indicates the safety of the cardiac rehabilitation program. To our knowledge, there have been no data assessing lower limb muscle strength in the sit-to-stand test and the get-up-and-go test in patients with LVADs so far. These tests provide additional data for the physical evaluation of LVAD patients. A comprehensive approach to the rehabilitation process in LVAD patients, including continuous psychological support, is important. In conclusion, early multimodal hospital cardiac rehabilitation results in significant benefits in exercise tolerance, muscle energy, complex coordination and overall performance in patients after LVAD implantation. The procedures used were safe and effective.