Introduction
Colonoscopy is crucial for detecting and localising pathological lesions within the colon. Colonoscopy quality is defined by a number of parameters, such as the caecal intubation rate (CIR), withdrawal time (WT), adenoma detection rate (ADR), and polyp detection rate (PDR). Adenomatous polyps are the most common precancerous lesions identified during endoscopic colorectal cancer (CRC) screening, and the removal of adenomas identified during colonoscopy is widely accepted as an effective means of preventing CRC morbidity and mortality [1, 2]. CRC is one of the major causes of cancer-associated morbidity and mortality in developing and well-developed countries. It is the second most prevalent cancer, affecting men and women almost equally. Approximately 600,000 deaths from CRC are estimated worldwide each year, representing 8% of all cancer deaths, which makes it the fourth leading cause of death among all malignancies [3, 4]. However, several studies have reported that 20–30% of precancerous adenomas are not detected with standard-viewing colonoscopy (SVC) [5, 6]. As such, missed adenomas can trigger interval CRC, and improving the adenoma detection during colonoscopy is important for enhancing screening efficiency. It is relatively difficult to visualise polyps on the proximal sides of the haustral folds, in the internal curves of flexures, and in the area around the ileocecal valve [7]. The newly introduced full-spectrum endoscope (FUSE®, EndoChoice®) provides a wider field of view, thereby potentially allowing endoscopists to observe more of the colon anatomy than with standard forward viewing endoscopes. By adding two lateral lenses to the tip of the scope, full-spectrum endoscopy (FUSE) increases the maximum field of view by nearly two-fold, from the previously ≤ 170° reported with standard forward viewing (SFV) colonoscopy to 330° with FUSE colonoscopy. The introduction of FUSE is intended to increase detection of pathological lesions, especially those situated behind the haustral folds of the bowel. This diagnostic modality should increase the ADR, especially in the right colon.
The primary aim of this study was to evaluate whether the use of FUSE colonoscopy in a population-based organised CRC screening program increases the detection rate (DR) of any adenoma and advanced adenomas compared with SFV colonoscopy.
Material and methods
We explored the efficacy of FUSE colonoscopy in a retrospective, single-centre feasibility study performed between January 1 and June 30, 2017. The study was conducted at a private nondependent hospital that performs approximately 9000 colonoscopies each year in Krakow, Poland. The hospital is equipped with Olympus Exera III 190 series endoscopes with high resolution and with a viewing angle of 170°. The FUSE equipment was made available by a Polish representative from the manufacturer. The study was approved by the local Ethics Committee and was conducted in accordance with the principles of the Declaration of Helsinki. As a clinical trial, the study was registered in a centralised clinical trials registry (ClinicalTrials.gov – NCT02929381). All study authors had access to the study data and reviewed and approved the final manuscript. The study enrolled 408 patients aged 18–80 years, who were eligible for colonoscopic examination performed for different indications, such as colorectal cancer screening, polyp surveillance, or diagnostic evaluation. Patients with prior abdominal surgery, colorectal resections, or inflammatory bowel disease were excluded from the study. The patients were randomised to either a standard frontal view (SFV) (Olympus Evis Exera III 190) or the novel full-spectrum colonoscopy (FUSE colonoscope CDVL slim c38, EndoChoice, Alpharetta, Georgia, USA). A total of 209 patients were examined with SFV and 199 with FUSE. The subject flow chart is represented in Figure 1.
All patients were given the same bowel preparation guidelines including oral ingestion of liquid propulsive agents (i.e. 420 g of polyethylene glycol (PEG) in 4 l of water taken in four doses every 6 h 1 day before the colonoscopy). Each colonoscopy was performed by one of three experienced endoscopists (each of whom had performed more than 5000 colonoscopies). A standard, commercially available, high-definition colonoscope (190 series Exera III NBI system with DF capability) was used for all SFV colonoscopies in this study.
The FUSE colonoscopy platform features a video colonoscope and a processor. The colonoscope is a standard adult device (168 cm in working length, outer diameter of 12.8 mm) that is flexible, re-usable, re-processable, and appropriate for repeated clinical use (for diagnostic visualisation and/or therapeutic interventions). The device has a high-resolution 330° field of view with all standard colonoscopic capabilities. The technical features are identical to those of current SFV colonoscopes in terms of manoeuvrability (including full tip deflection (up or down 180° and left or right 160°)); working channel diameter (3.8 mm); the availability of air or CO2 insufflation options; a suction feature; and forward water-jet irrigation. The FUSE colonoscopy features three imagers and light-emitting diode groups positioned at the front and on the sides of the distal tip of the colonoscopes. Olympus and FUSE towers are presented in Figure 2.
FUSE colonoscopes transmit images on three contiguous video displays. The left, centre, and right displays show colonic images transmitted from the left-facing, forward-facing, and right-facing lenses, respectively (Figure 3).
Figure 3
FUSE endoscopy display. The full-spectrum endoscopy (FUSE) helps to visualise the proximal sides of the haustral folds

After caecal intubation, the colonic mucosa was carefully visualised with WL while withdrawing the colonoscope. All polyps detected during the procedure were documented for size, location, and morphology (Paris, Kudo, and NICE endoscopic classifications of colorectal lesions). All images were captured and stored as high-definition JPEG files (200–300 kb, 1280 × 1024 pixel array, 32-bit RGB representation).
Statistical analysis
The materials acquired in this study were systematised and analysed, and variable distributions were determined. Because the analysed parameters did not have normal distributions, nonparametric tests were used in the analysis. Qualitative variables were compared using the independent χ2 test. The Mann-Whitney U test was used to compare quantitative variables between two groups. The Kruskal-Wallis test was used for comparisons of quantitative data in more than two groups. The materiality threshold was established at p < 0.05.
Results
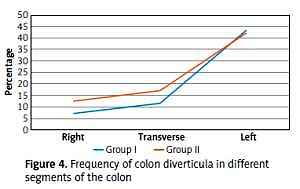
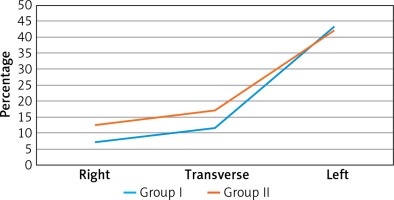
In total 209 patients were examined with SFV and 199 with FUSE endoscopes. The mean age of patients was 64.3 ±11.67 years. Both groups were comparable in terms of sex (p = 0.412), age, and BMI (p = 0.198) and the preparation of individual colonic regions. Patient characteristics are presented in Table I. All patients completed the study, and the success rates of caecal intubation were 100% with the SFV and FUSE colonoscopes. The CIT was significantly longer in the FUSE than in the SFV group (p < 0.001) (Tables II and III). Withdrawal times were comparable among the groups (p = 0.972). The PDR was higher in all colonic regions examined with FUSE (p < 0.001) (Table IV). The ADR and advanced ADR (aADR) in respective regions of the colon were similar between the groups; however, the total number of adenomas detected with FUSE was higher in the right and middle regions of the colon compared with SFV (p < 0.05) (Tables V and VI). Moreover, FUSE yielded a higher diverticula detection rate (DDR) in the right and middle colon (p < 0.001) (Table VII and Figure 4).
Table I
Patient characteristics
| Group | Sex | N | Age | BBPS | BMI | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | ± SD | Mean | ± SD | Min. | Max. | Mean | ± SD | |||
| I | F | 126 | 62.6 | 11.25 | 8.07 | 1.14 | 17 | 41 | 27.3 | 5.89 |
| M | 83 | 62.8 | 11.44 | 8.02 | 1.17 | 17 | 41 | 28.3 | 5.41 | |
| II | F | 112 | 65.5 | 11.98 | 8.13 | 1.22 | 17 | 40 | 27.2 | 4.33 |
| M | 87 | 66.4 | 11.72 | 8.02 | 1.23 | 18 | 38 | 26.5 | 4.26 | |
Table II
Caecal intubation time
| Group | Sex | Min. CIT [s] | Max. CIT [s] | Mean CIT [s] | ± SD | ||||
|---|---|---|---|---|---|---|---|---|---|
| I | F | 60 | 60 | 520 | 520 | 237.2 | 235.1 | 98.3 | 97.60 |
| M | 60 | 510 | 231.93 | 97.1 | |||||
| II | F | 90 | 90 | 585 | 585 | 297.80 | 311.6 | 121.5 | 122.04 |
| M | 100 | 560 | 329.6 | 121.1 | |||||
Table III
Withdrawal time
| Group | Sex | Min. CIT [s] | Max. CIT [s] | Mean CIT [s] | ± SD | ||||
|---|---|---|---|---|---|---|---|---|---|
| I | F | 360 | 360 | 970 | 970 | 509.0 | 510.9 | 114.38 | 118.43 |
| M | 360 | 915 | 513.7 | 124.98 | |||||
| II | F | 365 | 360 | 870 | 970 | 497.3 | 512.0 | 104.78 | 120.61 |
| M | 360 | 970 | 530.9 | 136.67 | |||||
Table IV
The incidence of polyps in segments of the colon
Table V
The incidence of adenomas (A)/advanced adenomas (AA) in segments of the colon
Table VI
Polyp, adenoma, and advanced adenoma burden in segments of the colon
| Group | Right part of the colon | Transverse part of the colon | Left part of the colon | Whole colon | |
|---|---|---|---|---|---|
| I | PB | 45 | 20 | 130 | 195 |
| AB | 24 | 13 | 59 | 96 | |
| AAB | 8 | 7 | 18 | 33 | |
| II | PB | 67 | 43 | 129 | 239 |
| AB | 36 | 15 | 46 | 97 | |
| AAB | 5 | 7 | 19 | 31 |
Table VII
The incidence of colon diverticula
The subjective opinions of the endoscopists performing the study on the insertion manoeuvrability and observation ability of the FUSE colonoscope were that they were inferior to those of the SFV colonoscope. However, the field of view of the FUSE colonoscope was superior to that of the SFV colonoscope.
Discussion
Endoscopic removal of adenomatous polyps has a significant long-term impact not only on reducing the rate of colon cancer occurrence but also colon cancer-related deaths [1, 2, 8]. Zauber et al. analysed mortality from colorectal cancer among patients who had adenomas removed compared with the incidence-based mortality from colorectal cancer in the general population as estimated from the Surveillance Epidemiology and End Results (SEER) Program and the observed mortality from colorectal cancer among patients with non-adenomatous polyps [2]. The authors observed a 53% reduction in mortality rate in the colonoscopic polypectomy group. This study supports that colonoscopic removal of adenomatous polyps is a successful approach to preventing colorectal cancer-related mortality [1, 2, 8].
According to many studies based on different populations of patients, a significant number of adenomas are missed with standard viewing colonoscopy [5–7]. Cases of CRC detected after a recently performed colonoscopy are most likely due to a missed lesion [7, 8]. The misdetection rate may be multifactorial and related to patient factors (position, adequate preparation of the colon, location and size of the lesion) and the level of the endoscopist’s experience with skills and manoeuvres that may increase the detection rate of colonic lesions [5, 7].
Rex et al. investigated 183 patients who underwent back-to-back colonoscopies, and they reported an overall adenoma miss rate of 24% [5]. Misdetection was present regardless of the polyp size. Even for adenomas of size 1 cm or larger, the misdetection rate still reached 6%. The highest misdetection rate was observed for the smallest polyps 5 mm or less in size, for patients who had two or more adenomas detected during first approach, and for lesions found on the right side of the colon. The high adenoma miss rate in this study was observed regardless the level of fluency in performing the exam, whereas all endoscopists who participated in the study had performed a high number of examinations during training and practice [5]. This supports other studies that the adenoma misdetection rate remains substantial, even when the exam is performed by an endoscopist considered as nearly infallible, who is highly experienced with a large number of cases. This high rate of misdetection during colonoscopy prompts action to be taken for further advancements in scoping technology to increase the overall detection feasibility.
Full-spectrum colonoscopy (FUSE) appears to have a clear advantage over standard colonoscopy in the detection of colonic lesions. The main feature of FUSE is an expanded viewing angle, which results in a significantly broader diagnostic spectrum. In addition to having identical technical features as the standard forward-viewing devices that are currently available on the market, FUSE allows for easy switching between a high-resolution viewing mode, from standard 160-degree, up to 330-degree “full-spectrum” viewing [9–12]. Increasing the field of vision makes this method more effective in diagnosing lesions located in blind spots, which are usually invisible to standard forward-viewing devices. Gralnek et al. in their pilot, prospective, single-centre study with total enrolment of 50 individuals, presented excellent results of FUSE feasibility in colorectal screening, polyp surveillance, and diagnostic evaluation [9]. The main goal of this study was to estimate the rate in caecal intubation, which was achieved in all cases examined. Moreover, some collateral endpoints were measured, such as the time to reach the caecum, withdrawal time, and total procedure time, with no acute and delayed adverse events observed as well as generally high patient satisfaction and high endoscopist subjective evaluation of this method. These favourable outcomes should prompt wide consideration of full-spectrum colonoscopy in clinical practice and further technical advancement in visualisation ranges of emerging devices [9–12].
According to our experience with the utilisation of full-spectrum endoscopy, we would like to support the findings of Gralnek et al., showing that this recently introduced diagnostic method is safe and efficacious in the detection of colonic lesions, especially in anatomic locations considered to be challenging for standard scoping. Although in our study the total number of adenomas detected with utilisation of full-spectrum colonoscopy (FUSE) was higher, especially when located in the middle and right side of the colon, we did not find a statistically significant difference in adenoma detection rate when compared with standard viewing. Potential distorting factors impacting the adenoma detection rate (ADR) were the high experience level of all endoscopists enrolled and the location of the study in a high-volume endoscopic centre (average 9000 colonoscopies annually).
In conclusion, full-spectrum colonoscopy allows for effective recognition of pathological lesions in the right and middle regions of the colon. Although it did not statistically affect ADR, the absolute number of adenomas detected was higher than with traditional SFV endoscopy.