All over the world, dietary risk factors are associated with millions of deaths and hundred millions of disability-adjusted life-years each year [1]. An energy-controlled Mediterranean diet is deemed to be the most scientifically tested eating pattern showing substantial health benefits for the general population. However, there is still a debate about what the best diet is for each person, especially with regard to the balance of macronutrients [2].
Overall, the Western world – but also most developing countries – eats too much energy. This is progressively increasing the scientist attention towards low-energy diets and different form of fasting as therapeutic and preventive tools [3, 4].
In the Mediterranean diet, carbohydrates are the main source of energy. A recent meta-analysis including data from 771,609 individuals with 223,657 all-cause deaths, 14,045 cardiovascular deaths, 18,264 cardiovascular non-fatal events and 3,643 non-fatal coronary heart disease, concluded that extremely low-carbohydrate diet is associated with a mildly increased coronary artery diseases risk (0.93, 95% confidence interval (CI): 0.81–1.06; I2 = 0%; n = 2) compared to high carbohydrate intake, without any impact on other main health outcomes. However, it must be recognized that the association between low-carbohydrate diet and coronary artery diseases was affected by the small cohort of individuals included in the analysis (2 studies on 17).
Available literature strongly supports the promotion of plant-based diets. A very recent and comprehensive meta-analysis of 76 studies including 2,230,443 individuals (with 60,718 cases of incident type 2 diabetes, 157,335 cardiovascular disease events, 57,759 cancer cases and 174,435 deaths) suggested the existence of an inverse association between higher adherence to a plant-based dietary pattern and risks of type 2 diabetes (risk ratio (RR) = 0.82, 95% CI: 0.77–0.86), cardiovascular diseases (0.90, 95% CI: 0.85–0.94), cancer (0.91, 95% CI: 0.87–0.96) and all-cause mortality (0.84, 95% CI: 0.78–0.92), with a moderate-to-high heterogeneity across the studies (I2 ranging from 47.8% to 95.4%) [5].
The most important challenge is to feed the world and warrant an adequate intake of proteins, to prevent the onset of tissue damages, anemia and sarcopenia. Plant proteins are the healthiest sources of amino acids, but their biological value is poor. On the other side, red meat (in particular, processed and grilled red meat) is associated with the worst cardiovascular and oncological outcomes [6]. Proteins derived from poultry, fish and dairy products are in the middle, however long-term high-protein diets should be avoided [7].
On a positive note: the modern diet is not just punitive, because cumulative evidence supports the use of pleasant beverage to healthy aging, in particular as regards coffee and tea, that are particularly rich in antioxidant and anti-inflammatory bioactive compounds [8, 9].
What about dietary supplementation? Recently, the findings from the COcoa Supplement and Multivitamin Outcomes Study (COSMOS) randomized double-blind, placebo-controlled, 2-by-2 factorial clinical trial were made available. During a median follow-up of 3.6 years, this study failed to demonstrate the effect of cocoa flavanols supplementation (500 mg/day) on the occurrence of cardiovascular events. However, among the secondary endpoints of the study, cocoa dietary supplementation was associated with a significant reduction in the risk of cardiovascular death (0.73, 95% CI: 0.54–0.98), without any safety concern [10]. As a part of the COSMOS trial, the COSMOS-Mind was also carried out. The COSMOS-Mind was a large randomized two-by-two factorial 3-year trial, during which cognitive functions were assessed by telephone at baseline and annually in 2,262 individuals (mean age = 73 years; 60% women; 89% non-Hispanic White). In this study, dietary supplementation with multivitamin resulted in a statistically significant benefit on global cognition compared to placebo (mean Z = 0.07, 95% CI: 0.02–0.12; p = 0.007), and this effect was most pronounced in participants with a history of cardiovascular disease (no history: 0.06, 95% CI: 0.01–0.11; positive history: 0.14, 95% CI: –0.02–0.31; interaction, nominal p = 0.01). Multivitamin-mineral benefits were also observed for memory and executive functions [11].
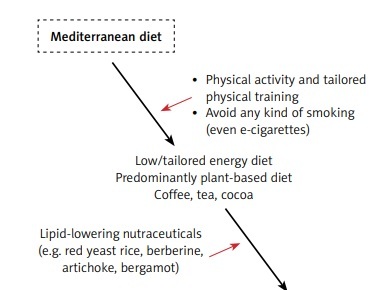
In different settings, a great attention has been given to the possibility of improving plasma cholesterol levels in healthy individuals at low-risk for cardiovascular diseases. In this context, a recent interesting network meta-analysis of 131 trials enrolling 13,062 participants showed that several bioactive substances are able to significantly reduce total and low-density lipoprotein cholesterol in plasma, being bergamot extract (–36.4 mg/dl) and red yeast rice (–46.8 mg/dl) the most effective/in the most effective way [12]. These findings were subsequently confirmed by more recent clinical trials testing the efficacy of standardized bergamot extracts [13] or combined nutraceuticals, including red yeast rice and artichoke extracts [14]. Of course, red yeast rice remains the most evidence-based dietary supplement for the management of suboptimal cholesterolemia in the general population [15].
Well-selected and adequately dosed nutraceuticals could exert a positive impact on largely prevalent diseases like non-alcoholic fatty liver disease [16] and in severe pathological conditions, including the skeletal muscle wasting in patients with heart failure [17].
Therefore, nutrition science is evolving either in a quantitative or a qualitative way. Nonetheless, all that glitters is not gold. For instance, at the beginning of the year, there was published a double-blind, placebo-controlled clinical trial that randomized participants to rosuvastatin 5 mg daily, placebo, fish oil, cinnamon, garlic, turmeric, plant sterols or red yeast rice for 28 days. The authors concluded that only rosuvastatin 5 mg was able to significantly reduce LDL-C plasma level, while the tested dietary supplements did not exert any lipid-lowering effect [18]. Unfortunately, this study was an example of research guiltily designed to attempt a result against the use of dietary supplements in clinical practice. The authors compared the lipid-lowering effect of a powerful statin to dietary supplements without any recognized effect on LDL-C (i.e. fish oil and cinnamon) or with a small effect on LDL-C (i.e. garlic and phytosterols). Moreover, a 4-week follow-up period of observation was too short since most of the lipid-lowering nutraceuticals exert their LDL-C lowering effect after 8–12 weeks, according to previous evidence [19]. Therefore, the true conclusion of the study should be that high-risk patients should be treated with statins and nutraceuticals are not effective in the very short term.
By the way, lifestyle measures do not include only diet. For example, we should not forget the importance of the physical activity in preventing obesity [20], and our attention should also focus on new potential behavioral risk factors, such as electronic nicotine delivery systems use (Figure 1) [21].
In conclusion, every day an increasing number of systematic reviews and meta-analyses of cohort studies help us to define better and better what a healthy diet is. Preclinical evidence and some clinical trials have recently introduced the need to individual tailored diet and the use of some dietary supplements that could safely support our healthy aging.