Lupus cystitis, a rare complication of systemic lupus erythematosus (SLE), was first reported in 1983 by Orth et al. and occurs in 0.5–1% of patients with SLE [1]. Lupus cystitis is mainly characterized clinically by urinary symptoms, while urinalysis is generally normal [1]. Ultrasound and CT scans demonstrate reduced bladder volume and irregular thickening of the bladder wall [1]. The diagnosis of lupus cystitis can be made when a patient with SLE has urinary symptoms combined with a bladder biopsy confirming interstitial cystitis [1].
SLE is characterized by deposition of circulating immune complexes, leading to necrotizing vasculitis of small arteries and veins [2]. The bladder wall and intestinal wall have numerous small vessels where circulating immune complexes can also be deposited. Therefore, bladder and bowel involvement can be an important part of the clinical presentation of SLE. Nishizaki et al. found that 81.7% of patients with lupus cystitis had combined lupus enteritis [3]. Kim et al. reviewed 17 of 19 patients with lupus enteritis who also had lupus cystitis [4]. Mok et al. reviewed 18 cases of SLE combined with intestinal pseudo-obstruction, 12 of which were associated with bilateral ureterohydronephrosis [5]. This suggests a strong correlation in the pathogenesis of lupus cystitis and lupus enteritis, as evidenced by the presence of common autoantigens in the bladder and gastrointestinal tract [6]. The clinical presentation of lupus enteritis is dominated by gastrointestinal symptoms, and enhanced CT of the abdomen helps in the diagnosis, which may manifest as the target sign or the comb sign [6]. A clinical diagnosis of lupus enteritis, once made, may be highly suggestive of combined lupus cystitis and vice versa. In order to fully assess the disease activity in SLE, both of these systems must be evaluated to avoid missed diagnoses.
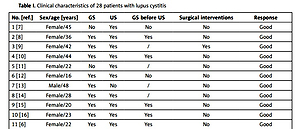
The Table I retrospectively analyzes the clinical data of lupus cystitis patients with a clear diagnosis and complete data published in PubMed since 2000 (using “systemic lupus erythematosus” and “cystitis” or “lupus cystitis” as search terms) to determine the population, symptoms, treatment, and prognosis of the disease [2, 6–26]. A total of 28 patients, 25 women and 3 men, with a mean age of 30.9 years, were enrolled in this study. In this study, 22 (78.6%) patients had both urinary and gastrointestinal symptoms, and 15 (53.6%) patients had gastrointestinal symptoms preceding urinary symptoms, exceeding the 35% reported by Shimizu et al. [18]. Twenty-five (89.3%) patients improved after the use of glucocorticoids and immunosuppressants, and only 3 patients had rapid deterioration and eventual death. Nine (32.1%) patients were treated with surgical procedures, including percutaneous nephrostomy.
Table I
Clinical characteristics of 28 patients with lupus cystitis
| No. [ref.] | Sex/age [years] | GS | US | GS before US | Surgical interventions | Response |
|---|---|---|---|---|---|---|
| 1 [7] | Female/45 | No | Yes | No | No | Good |
| 2 [8] | Female/36 | Yes | Yes | Yes | No | Good |
| 3 [9] | Female/42 | Yes | Yes | / | Yes | Good |
| 4 [10] | Female/44 | Yes | Yes | Yes | No | Good |
| 5 [11] | Female/22 | No | Yes | / | No | Good |
| 6 [12] | Female/16 | Yes | Yes | No | No | Good |
| 7 [13] | Male/48 | Yes | No | / | No | Good |
| 8 [14] | Female/28 | Yes | Yes | / | No | Good |
| 9 [15] | Female/20 | Yes | Yes | Yes | No | Good |
| 10 [16] | Female/23 | Yes | Yes | Yes | No | Good |
| 11 [6] | Female/22 | Yes | Yes | Yes | No | Good |
| 12 [17] | Female/14 | Yes | Yes | No | No | Good |
| 13 [2] | Male/56 | Yes | Yes | Yes | No | Good |
| 14 [18] | Female/37 | Yes | Yes | Yes | No | Good |
| 15 [19] | Female/38 | Yes | Yes | Yes | No | Good |
| 16 [20] | Female/27 | Yes | Yes | Yes | Yes | Good |
| 17 | Female/33 | Yes | Yes | Yes | No | Good |
| 18 [21] | Female/20 | No | Yes | / | Yes | Died |
| 19 [22] | Female/36 | Yes | Yes | Yes | Yes | Good |
| 20 [23] | Female/16 | Yes | Yes | Yes | No | Good |
| 21 [24] | Female/24 | Yes | Yes | / | Yes | Good |
| 22 | Female/28 | Yes | Yes | Yes | Yes | Died |
| 23 | Female/37 | Yes | Yes | / | Yes | Died |
| 24 | Male/20 | Yes | Yes | / | No | Good |
| 25 | Female/63 | No | Yes | No | Yes | Good |
| 26 | Female/15 | Yes | Yes | Yes | Yes | Good |
| 27 [25] | Female/44 | Yes | Yes | Yes | No | Good |
| 28 [26] | Female/11 | No | Yes | / | No | Good |
Lupus enteritis and lupus cystitis are closely related and share a common pathogenesis of smooth muscle dysmotility secondary to immune complex-mediated damage [6]. Lupus cystitis can lead to hydronephrosis due to edema or fibrosis of the tissue at the junction of the ureter and bladder, which is an obstructive urologic disease [21]. When SLE disease activity is controlled, the obstruction can be released and renal function can be reversed. If patients delay diagnosis and treatment, it will lead to irreversible pathological changes, resulting in a progressive decline in renal function and secondary pyelonephritis [21]. Once lupus cystitis or lupus enteritis is diagnosed, glucocorticoids are the first choice of treatment [19]. Given that lupus enteritis affects the absorption of drugs in the intestine, intravenous glucocorticoids can be used for these patients [4]. Immunosuppressive therapies such as cyclophosphamide, azathioprine, cyclosporine and mycophenolate are also effective [21]. However, one-third of lupus cystitis cases have to be treated surgically due to severe urinary obstruction [4].