Low-dose aspirin currently represents the milestone of antiplatelet therapy for patients with coronary artery disease (CAD), with proven efficacy in reducing recurrent ischemic events [1, 2].
Among patients with acute coronary syndrome (ACS) or undergoing percutaneous coronary intervention (PCI), the use of P2Y12 receptor inhibitors on top of aspirin has shown to reduce ischemic events at the cost of increased bleeding compared with aspirin alone [3].
In addition, the newer P2Y12 inhibitors, prasugrel and ticagrelor, have shown to further reduce ischemic events compared with clopidogrel, but with an additional trade-off in bleeding [4]. Therefore, dual antiplatelet therapy (DAPT) with aspirin and clopidogrel is considered the gold standard for stable patients undergoing PCI, while DAPT with a newer P2Y12 receptor inhibitor currently represents the gold standard for ACS patients [1, 5].
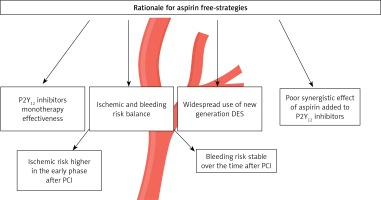
Despite that low-dose aspirin is largely administered worldwide and its use is endorsed by the main cardiology societies [5], a hot topic currently emerging in cardiovascular research is the dropping of aspirin after a short course of DAPT, the so-called aspirin free-strategies (Figure 1) aiming at reducing bleeding without any trade-off in ischemic events [1, 6].
Indeed, after ACS or PCI, the risk of ischemic events is higher during first months, as opposed to the risk of bleeding which tends to remain unchanged over the time, greatly impacting the prognosis of CAD patients [1, 7]. This holds true especially in patients with frailty, to the point that Kanenawa et al. proposed to consider frailty as a predictor for major bleeding [8].
Furthermore, there is an increasing understanding of the prognostic implications of bleeding, which are particularly relevant among patients with a high bleeding risk (HBR). With the aim of promptly identifying these patients and standardizing bleeding risks across trials, the Academic Research Consortium for High Bleeding Risk (ARC-HBR) have proposed a classification based on 14 major and 6 minor criteria, including items such as hemoglobin levels, renal and hepatic function, cancer or thrombocytopenia [1] (Table I).
Table I
The Academic Research Consortium for high bleeding risk definition (at least 1 major criterion, at least 2 minor criteria)
In addition, in vitro and ex vivo studies have suggested that the addition of low-dose aspirin on top of P2Y12 receptor inhibitors does not result in enhanced platelet inhibition compared with a strategy of P2Y12 receptor inhibitor monotherapy [1, 9].
Furthermore, the aspirin-free strategy lays its rationale on two other issues: 1) the widespread use of new generation drug-eluting stent (DES), remarkably associated with reduced ischemic events, and 2) aspirin gastrointestinal (GI) toxicity, a major drawback of aspirin, leading to increased GI bleeding and discontinuation of antithrombotic therapy [1, 6].
Hence, over the years we have seen the development of aspirin-free strategies testing P2Y12 inhibitor monotherapy (clopidogrel, ticagrelor and prasugrel) in different clinical settings and applied to different patient phenotypes with satisfying clinical results [10].
Focusing on ticagrelor, the first trial to investigate this strategy was the GLOBAL-LEADERS, comparing ticagrelor monotherapy for 23 months after 1-month DAPT versus standard DAPT (aspirin plus ticagrelor) for 12 months. Ticagrelor monotherapy was not superior to standard DAPT but proved to be non-inferior in preventing ischemic recurrences [11].
The safety of ticagrelor monotherapy emerged in the GLOBAL LEADERS trial paved the way for the design of other randomized controlled trials (RCTs), such as the TICO trial and the TWILIGHT trial, both comparing ticagrelor monotherapy after 3 months of DAPT versus standard 12-month DAPT, showing a clear reduction of major bleeding events in the ticagrelor monotherapy group especially in ACS patients [12, 13].
Major concerns surrounding the use of ticagrelor monotherapy include its most common side effect, dyspnea, which is the cause of antithrombotic therapy discontinuation in up to 25% of patients [6].
Clopidogrel is a P2Y12 inhibitor characterized by high interindividual variability in the pharmacodynamic response, leading to high platelet reactivity (HPR) and increased ischemic events in about 30% of treated patients [14]. The results of the SMART-CHOICE and STOPDAPT-2, which included both ACS and stable patients, were encouraging, with a reduction of bleeding without any trade-off in ischemic events with clopidogrel monotherapy after 1 or 3 months of DAPT versus standard 12-month DAPT. Nevertheless, when this strategy was tested selectively among ACS patients in the STOPDAPT-2 ACS trial, there was an increase in ischemic events in the clopidogrel monotherapy arm [1, 15].
Accordingly, there is still no convincing evidence about the safety and efficacy of a clopidogrel monotherapy after a short course of DAPT, especially among high ischemic risk patients such as those with ACS. The difference in the results of RCTs testing clopidogrel as opposed to those testing ticagrelor monotherapy is likely to be attributed to the fact that 30% of treated patients are non-responders to clopidogrel, while non-responsiveness to ticagrelor is very rare [14, 16]. For this reason the implementation of genetic testing and platelet function guide the use of clopidogrel represent a very promising strategy [1, 16, 17].
Few pieces of evidence are available on prasugrel monotherapy, tested only in the chronic coronary syndrome setting (CCS) in a pilot study, the ASET trial [18].
Several meta-analyses have focused on aspirin discontinuation with maintaining a P2Y12 inhibitor monotherapy, especially in ACS patients treated with ticagrelor [10, 19–21].
Eventually, a strategy of P2Y12 inhibitor monotherapy (mainly clopidogrel) have been tested in patients undergoing PCI with concomitant atrial fibrillation. The administration of a triple antithrombotic therapy, consisting of aspirin, clopidogrel and an oral anticoagulant is recommended for a period between 7 and 30 months, but the optimal duration of triple therapy is still a topic of debate [22].
In conclusion, recent European guidelines for the management of ACS propose several aspirin-free strategies: ticagrelor monotherapy after 3 months of DAPT, clopidogrel monotherapy after 1 or 3 months of DAPT in non ST-elevation acute coronary syndromes (NSTE-ACS) with HBR and clopidogrel monotherapy after 6 months of DAPT in ST-elevation acute coronary syndromes (STE-ACS) with HBR [1, 5].
Altogether, P2Y12 inhibitor monotherapy is a possible strategy according to current guidelines, even if not as the first-line therapy, but this strategy is not fully implemented in daily clinical practice.
Some argue that the use of aspirin should be completely abandoned after a short course of DAPT, others call for a reappraisal of the use of aspirin in light of its reliability over the years. We believe that it is worth gauging in detail clinical features of each patient, providing a personalized use of antithrombotic therapy [23].
Patients with poor risk factor control, such as those still smoking after an ACS, conducting sedentary life with low-density lipoprotein (LDL) levels not optimized and poor diabetes control, and concomitant low bleeding risk are the ones who may benefit the most from an intense DAPT regimen with aspirin. In contrast, HBR patients, such as those with chronic renal failure, anemia, history of cancer or episodes of bleeding and concomitant low ischemic risk are ideal candidates for aspirin-free strategies.
Conflict of interest
Giuseppe Biondi-Zoccai has consulted for Balmed, Cardionovum, Crannmedical, Eukon, Innovheart, Guidotti, Meditrial, Microport, Opsens Medical, Replycare, Teleflex, and Terumo. Pierre Sabouret reports consulting fees paid by Astra Zeneca, Amgen, BI, BMS, Lilly, Novartis, Sanofi, Servier, Vifor outside the submitted work.