China has been under strict prevention and control of COVID-19. The front-line nurses in China are responsible for nucleic acid collection and patient care, and they are under great psychological pressure. China’s front-line nurses who participate in the fight against the epidemic will have various psychological problems in the isolation ward, which need our attention, but there is currently no public report investigating the psychological stress and psychological needs of front-line nurses [1, 2]. The rapid spread of COVID-19, its wide range of coverage, and its acute nature have put tremendous pressure on China’s medical staff. China’s frontline nurses fighting the epidemic, i.e. nurses who have direct contact with confirmed or suspected cases and are in close contact with patients, are usually under tremendous psychological pressure. Although the frontline nurses are carefully protected, they are still in a state of high-risk occupational exposure during various nursing operations. Most of them are in a state of high stress, with increased psychological pressure [3]. Studies [4] have shown that among medical staff, as many as 60% may experience psychological crises in the event of an acute respiratory infection in the hospital. These conditions reduce the body’s immunity and resistance to varying degrees and increase the chance of infection for nursing staff.
As COVID-19 is a newly emerged respiratory disease, this study aims to study the psychological pressure feelings of frontline nurses in the early stage of the COVID-19 outbreak.
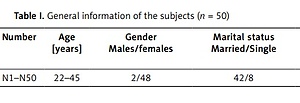
Guided by descriptive phenomenological research methods and using saturation of qualitative research data information as the standard, we used purposive sampling to enrol nurses who had worked for more than 2 weeks in the observation ward or COVID ward of a COVID-19 designated hospital in Hefei as subjects. The following inclusion criteria were used: (1) ≥ 18 years of age, registered nurses who met the health industry standards of the People’s Republic of China; (2) nurses who worked during the epidemic and directly contacted suspected or confirmed cases; and (3) nurses who signed informed consent to participate in this study voluntarily. The following exclusion criteria were used: (1) those who experienced major family changes in the past year; (2) training nurses; and (3) those who could not understand the content of the interview. A total of 50 frontline nurses were interviewed. The subjects’ names were replaced by “N1” to “N50” according to the order of the interviews. The general information is listed in Table I.
Table I
General information of the subjects (n = 50)
| Number | Age [years] | Gender Males/females | Marital status Married/Single | Education Associate/bachelor/Master | Work experience [years] |
|---|---|---|---|---|---|
| N1–N50 | 22–45 | 2/48 | 42/8 | 6/43/1 | 2–28 |
Based on the purpose of the study, a search of the relevant literature, the opinions of experts in infectious diseases and psychological consultation, and experts with qualitative research background, and an interview with a COVID frontline nurse. The interview outline was created and revised by the study team.
Material: Interview outline, informed consent, 2 recording pens, notebook, and pen.
A phenomenological research method of qualitative research was adopted, and one-on-one interviews were conducted using a semi-structured interview method. As the most commonly used method for collecting qualitative research data, semi-structured interviews are relatively focused, do not deviate far from the topic, and can uncover a deep level of information [5]. An interview outline was developed before the interview, and the approval of the Ethics Committee was obtained. Before the start of the interview, we informed the interviewee of the purpose of the interview, summarized the related issues involved, and described the interview method and its meaning. Before the start of the interview, the participant signed an informed consent form. During the interview, we observed and recorded the expressions and other nonverbal behaviours of the interviewees, and we took notes and made recordings on site, which were then archived [6]. The interviews were conducted when the interviewee had had sufficient rest, and night shifts and times when the interviewee was overworked were avoided to prevent psychological and emotional disturbances from affecting the interview results. Interviews were stopped when no new content was being added, and the interviews lasted 30 to 45 min [7].
The study was approved by the Ethics Committee of The First People’s Hospital of Hefei, China (Approval No. 2020-010-01). The study confirmed that all methods were carried out in accordance with relevant guidelines and regulations, and informed consent was obtained from all subjects and/or their legal guardian(s).
The data analysis method was based on the basic principles of text transcription in qualitative research [8]. After each interview, the interview data were transcribed and stored within 24 h. The content recorded during the interview and the interviewee’s expression, gestures, movements, and body postures were noted in the corresponding places in the text.
Quality Control: (1) An interview outline was developed before the interview, and the purpose of the interview was determined to avoid deviation from the subject. (2) An appropriate interview time and place was chosen to facilitate a full understanding of the true thoughts of the interviewee. (3) The interviewer had a thorough understanding of qualitative research methods and interview skills, and we avoided having participants interviewed by their managers, which can cause tension for the interviewee. (4) During the interview, complex, abstract, or sensitive issues were discussed in the second half of the interview to allow the interview to proceed smoothly. (5) Before the formal interview, 2 frontline nurses were pre-interviewed to reduce the Hawthorne effect. (6) According to the rules for reaching consensus, 2 researchers transcribed and analysed the interview content, and both parties needed to reach a consensus.
Based on the results of semi-structured interviews with 50 frontline nurses fighting COVID-19, 4 themes emerged, as follows: (1) emotional responses (tension, anxiety, and loneliness); (2) interpersonal relationship troubles; (3) psychological relief needs; and (4) certain expectations for working hours and working intensity.
There were 26 nurses who felt nervous and anxious about entering the frontline position in the fight against COVID-19. They were afraid that the disease would be highly contagious. In addition, they felt lonely because they were quarantined away from their families and children during their employment. Nurses 11, 23, 28, 39, 45, and 50 expressed the following: “I was on the first batch of nurses to enter the COVID-19 ward and have direct contact with patients. Because many procedures have not been determined, I do not know how to deal with patients. I feel nervous. The hospital isolation environment makes me feel anxious, and I can only fall asleep late at night.” Nurses 2, 9, 12, 35, and 43 said, “I pay more attention to my family and children, and I use WeChat videos to call home every day…I feel lonely without my family around me.” Nurses 4, 44, 47, and 49 said, “I always help my son with homework every day. I cannot go home after work, and I’m not at home for tutoring homework, and his father is not good at tutoring. Yesterday, the teacher criticized my son in the WeChat group. I called and reprimanded my son last night.” Nurses 5, 8, 14, and 19 said, “I feel anxious these days. Maybe because of a change of environment, I do not sleep well at night and often wake up.” Nurses 6, 17, 18, and 31 said, “I think I will feel anxious when I enter the isolation ward, especially for the night shift. I cannot wait for the end of the shift as soon as I enter the ward. I feel very tired when my work is particularly busy.” Nurses 20, 24, and 29 said, “I saw on my phone that the epidemic is so serious, and so many people have died. I am worried about what my family will do if I get infected. Therefore, when I enter the isolation ward, I am very nervous and afraid of not wearing protective equipment in the right way. I ask my colleagues to help me repeatedly check whether the protective suit is torn.”
Thirty-two nurses expressed worry about being infected. Nurses 4, 8, 10, 24, 28, 34, 37, 46, and 48 said, “For the 3 infected people admitted today, they just ate together at one meal. I feel that the COVID-19 is very contagious… We need to take protective measures. There was a patient (in the observation ward) who talks so close to me and coughs, and I am afraid that he is positive.” Nurses 3, 5, 13, 16, 20, 22, 23, 25, 41, and 43 said, “I feel that the medical surgical masks we are using are thinner than before. I am worried that they are not as protective as before. I am still afraid of being infected, even though the head nurse told us that although there is a shortage of supplies, the supplies provided to us are absolutely qualified.” Nurses 14, 17, 30, 35, 41, 44, and 50 said, “When I atomize a patient or perform other nursing operations, the patient coughs, and I will worry for a long time and worry that I will be infected.” Nurses 26, 27, 33, 39, 45, and 49 said, “There is a patient who has repeatedly tested positive for nucleic acid. She can never get out of the hospital. I think she is highly infectious. Every time I perform a nursing procedure for her, I am always scared.”
Forty-one nurses reported that their physical discomfort increased after wearing protective clothing and goggles. Nurses 37, 42, 47, and 49 said, “When I entered the isolation ward for the first time, I had the night shift. I felt a lack of air and then felt very sick and wanted to throw up, but fortunately, I had my colleagues.” Nurses 8, 10, 18, 20, 23, 28, 34, and 44 said, “It’s very hard to breath. When I get busy, my body is all sweaty, and then I feel very cold when I have time to take a break.” Nurses 2, 6, 15, 24, 35, and 39 all said in the interview, “After taking off the protective clothing and protective mask, I feel that the world is mine.” Nurses 12, 21, 25, 40, and 46 said, “After putting on protective equipment, nursing procedures become more difficult. I almost cannot place an intravenous infusion and venous blood.” Nurses 3, 7, 29, and 45 said, “I have become slower. It is hard to walk around the ward and it feels as though someone is dragging me.” Nurses 4, 11, 19, 32, 38, and 41 said, “The N95 mask makes me have an allergic reaction. No matter how good my skin care products are, they cannot save me. The markings caused by the N95 mask will not go away.” Nurses 9, 13, 17, and 27 said, “I am okay. I mainly have hypoxia, and opening my mouth to breathe makes my mouth feel dry.” Nurses 5, 14, 26, and 33 said, “It is very inconvenient to go to the toilet, and I dare not take off my protective clothing to eat and drink on time. I am hungry and thirsty, and sometimes I faint after having a hypoglycaemic reaction.”
In the interview, 18 nurses reported experiencing psychological pressure in their relationships with colleagues and leaders. Nurses 5, 6, 14, 23, 33, and 44 said, “The COVID ward and observation ward are medical teams formed by temporary personnel. Therefore, I am not familiar with many colleagues and doctors here. I feel like I cannot handle relationships with everyone, and I feel like there is no tacit understanding between us.” Nurses 3, 22, 27, 36, 45, and 49 said, “I think doctors go to the isolation ward less frequently and have less contact with patients every day. We go on for hours. We have to go through all kinds of bedside care, and there is a lot of risk of infection and a lot of physical waste.” Nurses 14, 39, and 41 said, “Leaders consider the shortage of protective equipment, and when the number of patients decreased, the manager mentioned something a few days ago about changing the double shift to a single shift. I feel like I am more anxious working alone in the isolation ward with no one to talk with.” Nurses 17, 30, and 32 said, “When I was working with a certain colleague, she always found excuses not to go to the isolation ward, so I spent more time doing aerosol inhalation and measuring vital signs. I am worried that it will increase the risk of infection for me.”
Thirty-one nurses felt that they needed psychological care. Nurses 12, 15, 23, 31, 35, 43, and 50 said, “Communicating more with friends will make me feel happy, and my stress will be reduced a lot.” Nurses 1, 9, 11, 16, 24, 29, and 33 said, “I video chat with my daughter every day, and talking to my daughter reduces my negative emotions.” Nurses 3, 5, 13, 18, 37, and 46 said, “I used to feel anxious and become stressed easily, and sometimes it is difficult for me to adjust by myself…” Nurses 17, 25, 32, 38, 42, and 47 said, “I think sometimes the care and encouragement of the manager is also essential. On the third day, when I had bad sleep and was stressed, I had a conversation with the manager for a while and felt much better.” Nurses 8, 19, 26, 39, and 49 said, “I sometimes feel like I need professional psychological counselling or Chinese Medicine Soothing Intervention.”
In the interview, 29 nurses indicated that they could work continuously for 6 h at most, 11 nurses indicated that 8 h of continuous work is acceptable, and 10 nurses indicated that the best uninterrupted work duration is 4 h. Nurses 1, 4, 6, 39, 44, 46, and 47 said, “It’s too stuffy to wear protective clothing. If I stay in the isolation ward and never come out, I think 6 h is my limit. In terms of work intensity, if the patient’s condition is mild, each nurse can manage about 10 patients.” Nurses 2, 3, 12, 20, and 30 said, “At the beginning of the epidemic, there were not enough people. My single shift lasted 12 h in the ward. To save protective clothing, I did not come out. I think 8 h is acceptable now.” Nurses 11, 13, 15, 17, 19, 22, 24, and 27 said, “Six hours is the most. If the patient needs intravenous infusion or sputum suction, I think I can only manage 3 patients at most.” Nurses 7, 10, 21, 34, 35, and 38 said, “Six hours is the maximum, and after 6 h, I will be a little irritable. As for the intensity of work, I have not encountered severely ill patients up to this point, and there is generally no problem with managing 9 patients.” Nurses 33, 40, 41, 42, 49, 50, 23, and 16 said, “Six hours is already my limit, and maybe I’m used to it….” Nurses 31, 32, 36, 37, 43, and 45 said, “Before entering the isolation ward, if I have made relevant preparations (go to the toilet, adjust the comfort level of protective equipment), I think I can bear it for 8 h.” Nurses 5, 8, 9, 14, 18, 25, 28, 29, 26, and 48 said, “If I cannot eat, drink water, or use the toilet for 12 h, I definitely won’t be able to last. I think 6 h is a bit too long. It’s even better if a shift is only 4 h.”
This study found through interviews that most of the frontline nurses had varying degrees of negative tension. The tension, anxiety, and loneliness of the frontline nurses in the COVID ward and the observation ward were most obvious due to the relatively closed working environment and the risk of infection. The high-stress working environment is accompanied by excessive tension, anxiety, worry about themselves and their family members, becoming ill, guilt related to their families, and even panic, restlessness, helplessness, and pessimism among medical staff, especially those on the front line fighting the epidemic. If these negative emotions are not addressed and resolved in a timely manner, they will have a substantial impact on individuals, hospitals, families, and society [9]. To reduce the psychological stress of frontline nurses, we can invite nationally certified psychological counsellors to provide psychological counselling through individual and group interventions. Individual interventions focus on interviewing; listening, understanding, and paying active attention to nurses after they enter the COVID-19 ward; positive resource utilization; relaxation techniques; mindfulness techniques [10]; group resource utilization and special periods and daily management based on the sunrise model of nursing [11]; the use of non-verbal resources in patient communication, ways to empathize with patients at special times, and the ability to ask for help; and how to gain more understanding and support from family members by expressing gratitude toward them. Group interventions occur during the rest times of nurses working in the COVID ward: first, the nurses are given an opportunity to talk to each other about their feelings and emotions; then, they are given time to talk about their own solutions and initiate discussions while receiving empathy, encouragement, support, and recognition of their hardship. Additionally, the group intervention allows nurses to see their own strength and their future self through narration, constructing signs of the physical behaviour of COVID epidemics, energizing themselves and their peers, giving them tools for relaxation and meditation, and seeing themselves.
The interviews found that because most of the nurses were female, the most frequently mentioned concerns were about their children’s lives and education. The second most frequently mentioned concern was their relationship with managers and colleagues. Social, governmental, organizational, and family support play an essential role in relieving the stress of frontline nurses fighting COVID-19 [12, 13]. Authors [14] showed that the better an individual’s family benefits are, the better the individual’s job performance is. Nurses fighting COVID-19 need more social, governmental, organizational, and family care and support to reduce the psychological pressure and burdens of caring for COVID-19 patients. Supportive acts such as affirmation from leadership and the supply of protective materials, assistance from people from all walks of life, recognition from the government, mutual encouragement between colleagues, and understanding and support from family members are necessary. In addition, the ear acupoint burying technique of traditional Chinese medicine (TMC) can be used as a decompression intervention. Bean pressing of auricular points is a common TCM technique. Vaccaria segetalis seeds or rapeseeds can be placed at a tender point according to acupoint theory and then fixed to stimulate the acupoint or reaction point on the auricle. This technique can adjust the function of the viscera and the human endocrine system through the meridian system to achieve a balanced functional status [15]. According to a survey, the rate of ear acupoint pressure on beans in the Beijing area is as high as 89.3%, and this method was effective for treating constipation, insomnia, and headaches [16–19]. We can invite TCM experts from the nursing clinic to perform ear acupoint pressure with beans to frontline nurses to reduce and relieve their anxiety.
COVID-19 is highly contagious and infects a large number of people, and there are currently no effective drugs for treatment. The number of patient deaths is increasing, and supplies have been scarce during the epidemic. The interviewed nurses were worried that their occupational protection was not adequate. Most of the nurses worried about the risk of infection. The infection of frontline nurses will affect the mental state of other medical staff, who will then be unable to provide good nursing for patients. Therefore, nursing managers should ensure that protective equipment is available, hospitals should exercise prevention and control measures, and various work procedures, and standardized training and guidance for frontline nurses fighting COVID-19 should be implemented. These interventions can reduce the chance of being infected and relieve psychological pressure. We should ensure the supply and quality of protective equipment for frontline nurses, provide rest places during work, and ensure that they are consuming an adequate diet and nutrition, which should be overseen by special personnel. We should also arrange reasonable shifts, solicit opinions from those involved in real time, and make prompt adjustments. We need to encourage treatment and nursing staff to communicate with each other and provide timely feedback on problems to meet their needs.
The results of interviews with multiple frontline nurses show that the most suitable duration for the uninterrupted use of protective equipment is 6 h. Wearing protective equipment for more than 6 h can cause physical discomfort for the nursing staff, and their mental health may be affected. Wearing protective equipment increases the difficulty of performing nursing procedures and increases the workload of nurses. Under conditions requiring intravenous infusion, atomization, inhalation, and sputum suction, one nurse can cover up to 3 patients. When these procedures are not required, one nurse can take care of 10 patients (our hospital did not receive critical patients, so critical care nurses were not interviewed). In terms of schedule, the time during which nurses wear protective equipment should not be too long. A period of 4–6 h is recommended. This period should be adjusted according to the workload and the number of nurses. Everyone’s input should be considered, and timely adjustments should be made.
In conclusion, frontline nurses experience negative mental states such as tension, anxiety, and fear and need relevant support from society and their families to improve their mental health. Due to the nature of COVID-19, the comprehensive skills of nurses are in relatively high demand; most medical facilities require senior and experienced nurses, and most nurses are female. Our hospital did not receive critical patients, so critical care nurses were not interviewed. Therefore, our sample had certain limitations.
The outcomes of our recent study are expected to have both local and global significance. Locally, they will reduce the incidence of nosocomial infections, save the economy, and improve the satisfaction of hospitalized patients with COVID-19. After targeted interventions, nurses will use a positive attitude and correct protection to minimize the incidence of nosocomial infections. It is conducive to the first-line nurses of similar infectious diseases in the future to treat patients in a positive state, provide patients with better care, and promote patient recovery. Globally, new coronary pneumonia is an infectious disease; this research can solve practical problems and enhance the confidence of all frontline nurses participating in the fight against COVID-19, provide a scientific theoretical basis and reference for the mental health maintenance, nurse scheduling, and management of the first-line nurses of similar infectious diseases in the future.
In conclusion, most frontline nurses in the fight against COVID-19 experience different degrees of psychological pressure. Managers should pay attention to frontline nurses, guide them in a timely manner, and take necessary intervention measures to relieve psychological pressure, adjust their psychological state, benefit their physical and mental health, and reduce the chance of infection.