The receptor-binding domain (RBD) of S protein plays an important role in facilitating coronavirus entry. These proteins facilitate the binding of human angiotensin-converting enzyme 2 (hACE-2), forming a complex. This RBD and ACE2 complex is a hot topic for researchers to investigate the viral mechanisms and to search for the possible intermediate host. CD26, CD147, and RBD have also been reported to facilitate virus entry. Over the past 20 years, several viral epidemics have taken place. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the causative agent for coronavirus disease 2019 (COVID-19) [1].
Recently, an association of the messenger RNA (mRNA)-based COVID-19 vaccine has been reported, raising concerns about vaccine safety in children and youth [2]. A number of side effects have been reported in children and youth, including pain, swelling, and redness in the arm where the shot is received, fever, tiredness, irritability, headache, chills, arthralgia, myalgia, and lymphomegaly. Postvaccine myocarditis and pericarditis are increasingly reported following mRNA vaccination against SARS-CoV-2. Rarely the associated myocardial tissue changes have been satisfactorily evaluated, while the degree of cardiac involvement seen in multisystemic inflammatory syndrome in children (MIS-C) remains exceedingly rare in children. The 2018 revised Lake Louise cardiovascular magnetic resonance (CMR) criteria are difficult to achieve, particularly in low- and middle-income countries or even in high-income countries with limited resources. There is substantial evidence that myocarditis may be underreported in this age group. The final consequences of such heart inflammation may remain unpredictable for a long time.
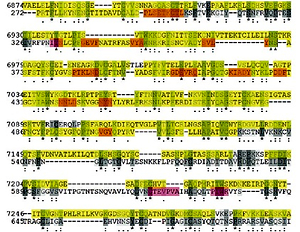
Titin is the most significant human protein (~33,000 amino acids) and the 3rd most abundant striated-muscle protein. Two titin molecules together span the sarcomere and are anchored at the Z-line and M-line. Titin is necessary for sarcomere assembly, modulates the active contractile force, and provides passive stiffness to cardiomyocytes [3]. DXR, a cardiotoxic anti-cancer drug, enhances oxidative stress and stimulates cardiomyocytes’ matrix metalloproteinase-2 (MMP-2). Recently, we demonstrated that MMP-2 activation is an early event in DXR cardiotoxicity and contributes to myofilament lysis by proteolyzing cardiac titin. Two orally available MMP inhibitors improved DXR cardiotoxicity. The intracellular and extracellular matrix remodeling was attenuated, suggesting that their use may be a potential prophylactic strategy to prevent heart injury during chemotherapy [3]. It has been proved that anti-interleukin 6 (anti-IL-6) receptor antibody improves cardiac dysfunction and left ventricular remodeling in an experimental myocarditis model induced by Coxsackievirus B3 (CVB3). Compared to controls, infected mice exhibited impaired systolic and diastolic function of the left ventricle associated with increased inflammation, fibrosis, and impaired titin phosphorylation. IL-6 receptor blockade constantly led to a shift of the immunologic response to a Th1 direction and significant viral load reduction. IL-6 receptor blockade exerts beneficial cardiac effects by antiviral and immunomodulatory actions after induction of an acute murine CVB3 virus myocarditis. In numerous cases of acute myocarditis, titin and the cytoskeleton are dysregulated. The CMR-identified myocardial edema may be a substantial issue for children and youth in the future due to a potentially dysregulated titin. Proteomic analysis revealed a striking similarity between the SARS-CoV-2 spike glycoprotein (gp) and the cardiac human protein titin (Figure 1). Twenty-nine pentapeptides are shared between the two proteins [4]. The peptide commonality does not reflect mere peptide sharing. Instead, it has relevant immunological potential. Nearly all of the shared sequences are present in experimentally validated SARS-CoV-2 spike gp-derived epitopes, thus supporting the possibility that the virus can trigger anti-titin autoimmune disease cross-reactions. The peptide sharing between the two species may evoke immune responses that cross-react with human proteins, thus causing harmful autoimmunity. More recently, a different pattern of characteristics and outcomes in patients hospitalized with COVID-19 was observed in the early phase of the fourth wave due to the Omicron variant compared with earlier waves in South Africa, with younger patients having fewer comorbidities, fewer hospitalizations, and respiratory diagnoses, and a decrease in severity and mortality [5].
Figure 1
A20220109F248CABF64506F29A91F8037F07B67D1010CE6C (job identifier in UniProt) showing some of the 239 identical positions and some of the 428 similar positions. Proteomic analysis revealed a striking similarity between the SARS-CoV-2 spike glycoprotein (gp) and the cardiac human protein titin
In our opinion, there is substantial evidence suggesting that we do not know how rare myocarditis and pericarditis are after COVID-19 mRNA vaccination without a proper animal model. The underreporting is probably one major issue in both industrialized countries and countries with low and medium income. Physicians and families should be aware of this risk, which should be considered in subjects presenting with even minimal chest pain within a week after vaccination. The initial evaluation should not be limited to ECG, cardiac troponin level, and inflammatory markers, but include echocardiography and cardiac MRI, despite the increasing costs that such evaluation may trigger. It is not a matter of debate that children rarely experience a severe disease following SARS-CoV-2 infection. It is important to consider at this time the true cost–benefit relationship for this kind of vaccination in children and youth. MIS-C is dreadful, but remains an infrequent complication of COVID-19. The dictum “primum non nocere (first, do no harm)” should remain revered in medicine.
Conflict of interest
The author is an associate editor of Archives of Medical Science. The article has been double-blind peer-reviewed by two external reviewers with anonymous text and citations. The author is responsible for the material and the text of this article. Affiliated institutions had no role in study design, data collection, analysis, decision to publish, or manuscript preparation. The author declares that receives royalties from Springer Publisher. All royalties go to pediatric charities.