The patient, a 36-year-old man, presented to the rheumatology department 3 days ago with sudden onset of severe, sharp low back pain after eating seafood. On examination, he had impaired spinal mobility, but a negative neurological examination and the Flexion Abduction External Rotation (FABER) test. He had received a diagnosis of gout 3 years prior to this presentation yet was not on any urate-lowering therapy. He also had a history of fatty liver and a body mass index (BMI) of 31.3 kg/m2, indicating poor lifestyle habits. Laboratory tests were negative for antinuclear antibodies, rheumatoid factor, anti-CCP antibodies, HLA-B27, T-SPOT for tuberculosis infection, tumor markers, immunofixation electrophoresis, and ANCA. He had a white blood cell count of 11.9 × 109/l (normal range 3.5–9.5 × 109/l), erythrocyte sedimentation rate (ESR) was 46 mm/h (normal range 0–15 mm/h), C-reactive protein (CRP) was 221 mg/l (normal range 0–10 mg/l) and serum uric acid was 483 μmol/l (normal range: 89–420 μmol/l). Computed tomography (CT) imaging of the spine showed degenerative lesions and magnetic resonance imaging (MRI) showed degenerative lesions, which is consistent with the imaging findings of the CT. No signs of spondylodiscitis, sacroiliac arthritis, disc herniation or spinal tuberculosis were visualized, and the MRI provided no explanation for his low back pain. Subsequent dual-energy CT (DECT) of the spine demonstrated numerous monosodium urate crystals around the bilateral costovertebral joints and scapular bones (Figure 1). Treatment with non-steroid anti-inflammatory drugs (NSAIDs) and colchicine to relieve acute attacks of gout was initiated, leading to a remarkable improvement in symptoms and laboratory findings. The final diagnosis of axial gout was made according to the 2015 gout classification criteria [1]. The ESR on subsequent reexamination decreased to 35 mm/h and CRP was 64.5 mg/l. At the 1-month follow-up, the patient reported no recurrence of his low back pain and no acute attacks of gout. In this patient, isolated gout attacks in the bilateral costovertebral joints and scapular bones can radiate to the periphery, manifesting as lower low back pain.
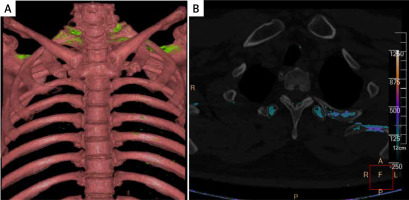
Figure 1
Dual-energy CT revealed numerous monosodium urate crystals around the bilateral costovertebral joints and scapular bones
Causes of low back pain usually include lumbar strain, lumbar disc herniation, spinal fracture, ankylosing spondylitis, spinal tumor, urinary tract stone, Mycobacterium tuberculosis and septic bacterial infections, while those caused by gout in the peri-scapular region are rare. The clinical presentation of spinal gout is diverse, with axial pain symptoms such as low back pain usually presenting in the corresponding areas affected by urate deposition. The study showed that of 131 patients with spinal gout in different locations, the most common presentation was low back pain (89 patients, 68.5%) [2]. Among a sample of 54 patients with gout, Jajic found that 12 of them (22%) had abnormal radiographs with hyperostotic spondylosis or diffuse idiopathic spinal hyperostosis, and the results suggest that patients with gout usually have spinal disease [3]. Therefore, the hypothetical mechanism for the association between acute low back pain and numerous monosodium urate crystals around the bilateral costovertebral joints and scapular bones in our patient may be triggered by degenerative disease of the lumbar spine, as demonstrated by his spinal CT and MRI. Previous studies have shown that gouty sacroiliac arthritis can be an often overlooked cause of inflammatory back pain [4]. However, CT imaging of the sacroiliac joint in our patient was normal and did not suggest sacroiliac arthritis. Meanwhile, spinal gout may be more common than thought, with up to 1/3 of patients with gout reporting spinal gout [5]. Back pain is the most common presenting symptom, followed by neurological symptoms due to spinal cord or nerve root compressions [5, 6]. However, our patient had normal neurological symptoms and no signs of gout entrapment in the spinal cord or lumbar disc herniation on MRI of the lumbar spine. The association between acute low back pain and numerous monosodium urate crystals around the bilateral costovertebral joints and scapular bones needs to be validated by following up on the case and evaluating the possibility to “wash out” the deposits with the administration of a long-term therapy that lowers the uric acid level.
In the 2015 classification criteria for gout, imaging evidence of urate deposition in symptomatic (ever) joint or bursa, including ultrasound evidence of double-contour sign or DECT demonstrating urate deposition, was considered one of the criteria [1]. The first metatarsophalangeal joint is most commonly affected by gout. Other common sites such as gout located in the costovertebral joints and scapular bones are very unusual conditions [7]. In addition, axial gout should be considered in the presence of severe neck or back pain, fever, and increased inflammatory parameters, despite abnormally normal or even decreased serum urate concentrations [8]. A systematic review of the diagnostic accuracy of dual-energy CT in gout found a pooled sensitivity of 88% and a specificity of 90% [9]. Dual-energy computed tomography is a noninvasive technique that may be beneficial in detecting axial gout when joint fluid aspiration is considered unsafe.



