Familial hypercholesterolemia (FH) is a monogenic disorder (1 : 250–1 : 300) with an autosomal dominant inheritance pattern that leads to premature atherosclerosis and, consequently, to cardiovascular disease (CVD), including coronary artery disease, stroke, and peripheral arterial disease [1, 2]. It is estimated that in Europe, FH affects more than 500,000 children and 2 million adults. However, fewer than 5% of children with FH are diagnosed, and only a small fraction of affected individuals receive lipid-lowering therapy (LLT). Sustained exposure to elevated low-density lipoprotein cholesterol (LDL-C) concentrations from birth accelerates atherosclerotic processes, resulting in up to a 7–10-fold increase in the risk of premature CVD morbidity and mortality [3]. Approximately 50% of untreated men and 30% of untreated women with FH will experience a myocardial infarction before the age of 50 and 60, respectively [4, 5]. This highlights the urgent need for earlier detection and timely intervention to mitigate the lifelong cardiovascular burden of FH. Despite the clinical relevance, the diagnostic rate of FH in Poland remains extremely low, with detection rates estimated at ~3% in children and 4% in adults [6]. Since 3rd May 2025, an universal lipid screening as part of the routine health assessment for 6-year-old children was introduced pursuant to an amendment to the Regulation of the Minister of Health on guaranteed primary care services [7]. This change represents a significant step forward in the early detection of FH and underscores the importance of systematic early-life screening for FH as a public health strategy to improve detection, enable timely initiation of LLT and prevent premature CVD and mortality. Given the extremely low detection rates of FH in Poland and the recent introduction of universal lipid screening in 6-year-old children, assessing the level of knowledge and clinical practice among frontline clinicians becomes critically important. Pediatricians and family physicians are the first point of contact for children and their families. On this account, the awareness, confidence and preparedness of practitioners who undertake care of children to recognize and manage FH directly influence the success of early detection programs. Conducting a structured survey among Polish physicians was therefore essential to identify existing knowledge gaps and barriers to care.
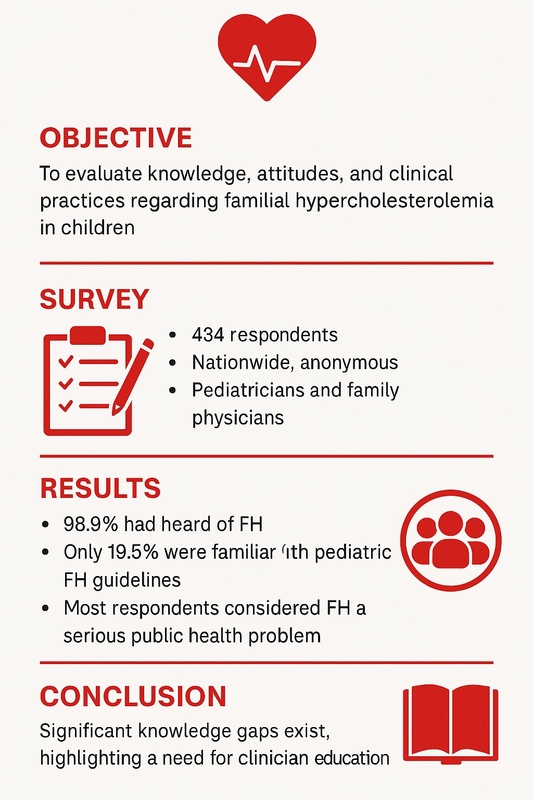
The primary objective of this study was to evaluate the knowledge and clinical practices of pediatricians and family physicians in Poland with respect to the diagnosis and management of FH in children. The survey included also questions assessing physicians’ attitudes toward the importance of FH as a public health issue, their perceived preparedness for FH diagnosis and management, and their willingness to receive further education on the topic.
Methods
The 28-question survey was distributed electronically using Google Forms between May and August 2025 among pediatricians, family physicians, and physicians in training across Poland (Supplementary Material S1). Invitations containing the survey link were sent via e-mail to clinicians involved in the care of pediatric patients.
Additionally, the questionnaire was disseminated through professional social media groups bringing together pediatricians and other physicians working with children, in order to maximize outreach and participation.
The calculated response rate was 10.5%. As the study was based on an anonymous survey conducted among healthcare professionals and did not constitute a medical experiment or involve patient data, according to the statement of the Ethics Committee, it did not require separate ethical approval.
Statistical analysis
Data were analyzed using Python 3.13.8 (Python Software Foundation, Wilmington, DE, USA). Descriptive statistics were used to summarize respondent characteristics and survey responses. Categorical variables were presented as frequencies and percentages; continuous variables as means ± standard deviations. Associations between physician specialty or years in practice and knowledge/practice indicators were assessed using χ2 tests with Cramér’s V for categorical variables, Mann-Whitney U or Kruskal-Wallis tests for ordinal data and Spearman’s correlation for continuous or count variables (e.g., number of diagnostic criteria selected). A p-value < 0.05 was considered statistically significant.
Results
A total of 451 clinicians participated in the survey; after excluding questionnaires with substantial missing data, 434 completed responses were included in the final analysis. The vast majority of respondents were female physicians (413/434, 95.2%). The geographical distribution of respondents covered all Polish regions, with the highest representation from the Silesian Voivodeship (41.5%), followed by the Masovian (8.8%), Lesser Poland (7.8%) and Lower Silesian (7.6%) regions. Regarding professional experience, most clinicians reported 5–10 years (37.6%) or 10–20 years (32.9%) of practice. In terms of specialization/specialty, the largest group consisted of pediatricians (49.3%), followed by residents in pediatrics or family medicine (32.9%) and family physicians (12.0%). The largest proportion of respondents were employed in primary care (32.3%), followed by those working in clinical hospitals (16.4%) and non-academic hospitals (15.2%). The vast majority of respondents had heard of FH (98.9%). Table I summarizes the essential information from the survey. Regarding treatment initiation, 31.6% indicated 6 years of age (the correct guideline-based answer). With regard to clinical practice, 31.8% reported ordering lipid profiles in children aged 2–10 years only when both family history and obesity/hypertension were present, 25.9% only in obesity/hypertension, 16.5% in all children, 14.6% not at all, and 7.8% only with a family history. In the case vignette of an 8-year-old child with LDL-C > 200 mg/dl and a positive family history of myocardial infarction, the most common management choice (31.6%) was diet and education combined with family screening, specialist referral, and consideration of pharmacological treatment. The most frequently reported barriers to care included limited parental awareness and cooperation (45.3%), lack of access to specialized centers (22.0%). In terms of attitudes, over half of respondents (51.7%) considered FH to be a serious public health problem/issue, while only 1.1% believed that pediatricians are adequately prepared for FH diagnosis. The vast majority (94.5%) expressed a strong willingness to receive additional training on FH and lipid disorders. Only 19.5% of respondents reported being familiar with pediatric FH guidelines based on self-assessment. X2 analysis revealed a statistically significant association between physician specialty and awareness of guidelines (χ2 = 45.38, p < 0.001). The effect size, measured by Cramér’s V, was 0.32, indicating a moderate relationship. Kruskal-Wallis test demonstrated significant differences in self-assessed knowledge across physician specialties (H = 31.81, p = 0.004), suggesting that perceived knowledge levels vary substantially between groups. Being a pediatrician was associated with lower odds of guideline awareness compared to other specialties (OR = 0.43, 95% CI: 0.21–0.86, p = 0.018). Years in practice did not independently predict awareness (p = 0.153) (Table I).
Table I
Summary of questionnaire findings amongst Polish physicians on FH care in children (n = 434)
Discussion
This nationwide survey revealed substantial deficiencies in pediatricians’ knowledge and awareness of FH in Poland. Although the vast majority of respondents had heard of FH, fewer than one in five rated their knowledge as above average, and only half were aware of existing guidelines. While most recognized FH as a genetic disorder and correctly identified the characteristic lipid profile, fewer than one-third accurately indicated its prevalence, and only a small proportion were familiar with diagnostic thresholds for premature cardiovascular disease.
Beyond knowledge and clinical practice, the survey also provided valuable insights into physicians’ attitudes. Although most respondents acknowledged FH as a significant public health problem/issue, only a very small fraction believed that pediatricians are adequately prepared for its diagnosis. This discrepancy highlights both a general awareness of FH’s importance and a perceived lack of confidence or available resources to manage affected patients effectively.
Comparable findings have been reported in previous studies conducted among physicians in Asia [8], general practitioners in North-West England [9], and pediatricians in the Netherlands [10]. In particular, the “Ten Countries Study” across the Asia-Pacific region [8] showed that only one-third of primary care physicians considered themselves familiar with FH, and awareness of its prevalence, genetic inheritance, and cardiovascular risk was markedly limited. In contrast, while almost all Polish physicians in our survey (98.9%) had heard of FH, detailed knowledge and familiarity with pediatric guidelines remained similarly suboptimal, suggesting that educational gaps in FH awareness persist across diverse healthcare systems worldwide.
Physician attitudes – particularly self-perceived competence and responsibility – have been shown to play a key role in the success of screening and referral programs. Early identification and treatment not only prevent avoidable cardiovascular events but also align with international recommendations and initiatives such as the Prague Declaration. These findings indicate a high level of perceived importance but limited confidence in personal and institutional readiness to manage FH effectively. Together with global FHSC data [11, 12], our results underscore the urgent need for enhanced clinician education and structured referral pathways.
In conclusion, significant knowledge gaps regarding FH persist among pediatricians in Poland as well as reflect a broader international challenge in pediatric FH care. Addressing these deficiencies through targeted education and standardized care pathways is critical. The recent introduction in Poland of mandatory lipid profiling as part of the 6-year-old health check represents an important step forward and is expected to substantially improve early FH detection, which in turn will contribute to more effective treatment and prevention of cardiovascular disease.
This study has several limitations. The 10.5% response rate was estimated based on the number of physicians personally contacted by e-mail and the approximate reach of mailing lists; thus, it represents only a minimum value. Because some physicians in Poland do not use electronic communication and the survey was not distributed in person, the actual denominator remains uncertain, introducing potential non-response bias. The predominance of female respondents and regional clustering from Silesia likely reflect workforce composition and recruitment networks, limiting generalizability. Finally, although the questionnaire was adapted from instruments previously used in international studies – Including the “Ten Countries Study” [8] and the recent European Journal of Pediatrics survey [10], it was not formally validated in Polish, which may have introduced response bias.