Heart failure (HF) is a complex clinical syndrome with high prevalence, affecting up to 5 per 1,000 citizens in Europe [1]. With aging populations, comorbidities, and rising hospitalizations, HF has become a significant clinical, social, and economic challenge [2]. Contemporary data on the clinical profile and prognosis of Polish patients are limited [3]. The HF-POL registry [3] described HF with left ventricular ejection fraction (LVEF) > 40% in Poland, while European registries, such as the Swedish Heart Failure Registry [4], the ESC EORP Heart Failure III Registry [5], and the ESC-HFA EORP Heart Failure Long-Term Registry [6], have provided broader perspectives. However, Polish data covering the full HF spectrum remain lacking. To address this, the nationwide Heart Failure Observational Study (HEROES) was initiated [7]. The study rationale and methodology were published previously [7]. Its primary goal was to collect contemporary clinical data on hospitalized and outpatient HF patients in Poland across all phenotypes: reduced ejection fraction (HFrEF), mildly reduced ejection fraction (HFmrEF), and preserved ejection fraction (HFpEF), diagnosed per European Society of Cardiology (ESC) guidelines [2]. Recruitment began on February 20, 2022, closed in February 2024, and follow-up ended on May 21, 2024. This paper presents baseline epidemiological and clinical data from 1,422 patients enrolled in HEROES.
Material
Follow-up, concluded on May 21, 2024, included all-cause mortality verified via the Polish Ministry of Digital Affairs. The study protocol was approved by the Medical University of Lodz ethics committee (RNN/316/20/KE, Dec 20, 2020; amendments/update KE/762/23, Sep 12, 2023). HEROES was funded by the Polish Cardiac Society (CRU 0120-KCKB-2023). Dataset and eCRF are available via the Medical University of Lodz repository (DOI: 10.60941/JVH1-5190).
This subanalysis included demographic data (sex, age), HF phenotype (HFrEF, HFmrEF, HFpEF by LVEF), body mass index (BMI), New York Heart Association (NYHA) class, NT-proBNP, comorbidities (atrial fibrillation [AF], coronary artery bypass grafting [CABG], chronic kidney disease [CKD], chronic obstructive pulmonary disease [COPD], diabetes mellitus [DM], arterial hypertension [HA], myocardial infarction [MI], percutaneous coronary intervention [PCI], stroke/TIA), and mortality.
Statistical analysis
Statistical analysis was performed with Statistica 13.1 (Tibco, Palo Alto, CA, USA). Nominal variables are given as absolute values and percentages. Continuous variables, non-normally distributed (Shapiro-Wilk test), are expressed as medians with interquartile range (IQR). Group differences were tested with chi-squared or Kruskal-Wallis H test, with Bonferroni correction as appropriate.
Results
Thirty-nine active sites (7 outpatient, 32 hospital) recruited a median of 20 patients per site (IQR 8–61; range: 2–203). A total of 1,422 patients were included; 80.4% hospitalized and 19.6% outpatient. Median age was 69 years, median EF 38%, and most patients were men. HFrEF accounted for 49.9% (n = 709), HFmrEF 13.4% (n = 190), and HFpEF 22.5% (n = 320); EF was missing in 14.3%. Across phenotypes, the proportion of women, BMI, and age increased, while NT-proBNP decreased. HFrEF patients were typically younger, thinner men with ischemic heart disease, whereas HFpEF patients were older women with higher BMI and more comorbidities (HA, COPD, AF, CKD). DM was the most frequent extracardiac comorbidity. COPD and HA were most prevalent in HFpEF. Median follow-up was 485 days (IQR: 397–599). All-cause mortality exceeded 16%, highest in HFrEF, both overall and annually (p > 0.05; Tables I and II).
Table I
Results of the HEROES – study population overall
| Parameter | Overall N = 1422 | HFrEF N = 709 | HFmrEF N = 190 | HFpEF N = 321 | P-value |
|---|---|---|---|---|---|
| Type of visit [n] | |||||
| Hospitalization | 1143 | 602 | 136 | 251 | NA |
| Outpatient | 279 | 107 | 54 | 70 | |
| Sex | |||||
| Men | 71.4% (1016) | 82.7% (586) | 68.4% (130) | 50.8% (163) | < 0.001 |
| Women | 28.6% (406) | 17.3% (123) | 31.6% (60) | 49.2% (158) | |
| Age [years] median (IQR) | 69 (60–76) | 66 (57–74) | 71.5 (67–78) | 73 (65–81) | < 0.001 |
| BMI [kg/m2] median (IQR) | 27.9 (24.8–32.0) | 27.8 (24.9–31.4) | 28.1 (24.8–32.1) | 29.3 (25.2–33.6) | 0.03 |
| EF (%) median (IQR) | 38 (27–50) | 30 (20–35) | 45 (44–47) | 55 (52–60) | < 0.001 |
| NT-proBNP [pg/ml] median (IQR) | 2629 (835–6478) | 3639.5 (1279–8443) | 2606 (878–5684.5) | 1238.7 (408.4–3318.5) | < 0.001 |
| NYHA* | |||||
| I | 12.7% (175) | 8.5% (60) | 20.0% (38) | 12.8% (41) | < 0.001 |
| II | 37.3% (515) | 37.0% (262) | 36.3% (69) | 38.3% (123) | |
| III | 37.1% (512) | 39.1% (277) | 32.6% (62) | 39.3% (126) | |
| IV | 13.0% (179) | 15.5% (110) | 11.1% (21) | 9.7% (31) | |
| Comorbidities | |||||
| Previous MI | 34.8% (409) | 35.9% (203) | 30.7% (51) | 19.9% (64) | < 0.001 |
| Previous PCI | 29.2% (343) | 29.9% (165) | 25.3% (42) | 29.7% (53) | < 0.001 |
| Previous CABG | 8.5% (100) | 9.9% (56) | 7.2% (12) | 7.2% (23) | 0.25 |
| HA | 65.9% (775) | 64.8% (366) | 68.7% (114) | 76.9% (247) | < 0.001 |
| AF | 51.8% (730) | 52.0% (369) | 47.9% (91) | 53.9% (173) | 0.44 |
| DM | 38.0% (536) | 38.4% (272) | 37.4% (71) | 35.8% (115) | 0.94 |
| COPD | 9.6% (135) | 8.0% (57) | 7.9% (15) | 12.8% (41) | 0.04 |
| CKD | 27.2% (383) | 28.1% (199) | 22.6% (43) | 28.3% (91) | 0.21 |
| Previous stroke/TIA | 10% (118) | 9.9% (56) | 7.2% (12) | 10.0% (32) | 0.98 |
| Mortality – median follow–up: 485 days (IQR: 397–599 days) | |||||
| Overall mortality | 16.2% (231) | 17.8% (126) | 12.6% (24) | 13.1% (42) | 0.07 |
| 1–year mortality | 12.9% (183) | 14.2% (101) | 10.5% (20) | 10.3% (33) | 0.10 |
AF – atrial fibrillation, CABG – coronary artery bypass grafting, CKD – chronic kidney disease, COPD – chronic obstructive pulmonary disease, DM – diabetes mellitus, EF – ejection fraction, HA – arterial hypertension, HFmrEF – heart failure with mildly reduced ejection fraction, HFpEF – heart failure with preserved ejection fraction, HFrEF – heart failure with reduced ejection fraction, IQR – interquartile range, MI – myocardial infarction, NT-proBNP – N-terminal prohormone of brain natriuretic peptide, NYHA class – New York Heart Association classification, PCI – percutaneous coronary intervention, TIA – transient ischemic attack.
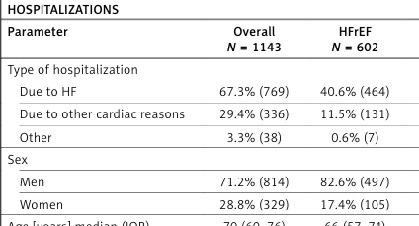
Table II
Results of the HEROES – among hospitalized and outpatient subjects
[i] AF – atrial fibrillation, CABG – coronary artery bypass grafting, CKD – chronic kidney disease, COPD – chronic obstructive pulmonary disease, DM – diabetes mellitus, EF – ejection fraction, HA – arterial hypertension, HFmrEF – heart failure with mildly reduced ejection fraction, HFpEF – heart failure with preserved ejection fraction, HFrEF – heart failure with reduced ejection fraction, IQR – interquartile range, MI – myocardial infarction, NT-proBNP – N-terminal prohormone of brain natriuretic peptide, NYHA class – New York Heart Association classification, PCI – percutaneous coronary intervention, TIA – transient ischemic attack.
HEROES provides a representative overview of HF in Poland. Findings show systematic variation across phenotypes: HFrEF patients were younger males with lower BMI and higher NT-proBNP, while HFpEF patients were older females with higher BMI, lower NT-proBNP, and more comorbidities. HFmrEF patients had intermediate features. The high prevalence of DM, CKD, and COPD underscores the need for comprehensive management addressing both cardiac and extracardiac conditions. Alarmingly, mortality exceeded 16% within 16 months, particularly among hospitalized patients, underscoring the vulnerability of this group.
Comparisons with European and U.S. cohorts [8–11] show similar trends. HFpEF patients were older, more often female, with higher BMI, lower NT-proBNP, and higher prevalence of AF and COPD. HEROES and HF-POL [3, 12] populations of HFmrEF and HFpEF were comparable, though HF-POL (EF > 40%) did not differentiate between these phenotypes, and mortality data are pending.
Compared with the Swedish Heart Failure Registry [4], Polish patients more often had DM but less CKD. HEROES patients were older overall but younger within subgroups. Men predominated in HEROES overall, especially in HFrEF and HFmrEF, but were fewer in HFpEF compared to Sweden (HEROES vs. Swedish: overall 71.4% vs. 67.5%; HFrEF 82.7% vs. 66.9%; HFmrEF 68.4% vs. 61.6%; HFpEF 50.6% vs. 60.8%). Median age was 69 vs. 60 years overall, but lower in Polish HFrEF (66 vs. 71), HFmrEF (71.5 vs. 78), and HFpEF (73 vs. 79).
Differences between inpatients and outpatients mirrored ESC-EORP HF registries [5, 6]. Outpatients were younger, more often NYHA I–II, with lower NT-proBNP. Data from ESC-EORP HF III [6] confirm hospitalized HFpEF patients were older women, and HFrEF patients were younger men with ischemic etiology. However, that registry included only acute HF admissions, while HEROES included all HF hospitalizations, including two-thirds HF-related.
Poland has the highest age-standardized HF mortality in high-income ESC countries [13]. In 2018, HF caused nearly 41,000 deaths, 9.8% of all Polish deaths [14]. In Sweden, 40% of patients died during 1.9 years’ median follow-up [4]. The latest Swedish report (1997–2022) found annual mortality of 24% [15], higher than in HEROES. Differences may reflect younger HEROES patients and the introduction of SGLT2 inhibitors in Poland.
This observational study may contain missing or inaccurate data and cannot be fully generalized. HFpEF prevalence may be underestimated, as these patients are often hospitalized in non-cardiology wards. Nonetheless, HEROES provides one of the first current datasets on all-cause mortality in Polish HF.
In conclusion, HEROES delivers the first nationwide data on the full spectrum of HF in Poland. Differences across phenotypes align with European trends. Compared to Swedish data, Polish HF patients were older overall, with higher rates of hypertension and diabetes, but lower rates of AF, COPD, CKD, and stroke/TIA. Mortality remains high, emphasizing the need for improved HF care in Poland.
Study URL: https://heroes.umed.pl. Dataset: https://doi.org/10.60941/JVH1-5190. [dataset] Polskie Towarzystwo Kardiologiczne/Polish Cardiac Society 2023. “Badanie Obserwacyjne Niewydolności Serca Polskiego Towarzystwa Kardiologicznego”. Medical University of Lodz. https://doi.org/10.60941/JVH1-5190.