Male erectile dysfunction (ED) is primarily driven by an impairment in the normal physiological processes required for penile erection, which involve vascular, neurological, hormonal, and psychological systems [1]. Vascular dysfunction, in particular, is a key determinant in the pathophysiology of ED, with endothelial dysfunction leading to reduced nitric oxide bioavailability and impaired vasodilation of penile arteries [2]. Neurogenic ED, on the other hand, involves disruptions in the nerve pathways that mediate erectile responses, while hormonal imbalances, especially low testosterone levels, are also implicated in the development of ED [3]. Given the complexity of these underlying mechanisms, there is growing recognition of the need for a comprehensive understanding of the various biological pathways contributing to ED risk, including nutritional factors such as vitamin intake. Both hypervitaminosis and hypovitaminosis have been suggested to impact erectile function. Excessive vitamin intake (hypervitaminosis) may lead to oxidative imbalances, endothelial dysfunction, or hormonal disruptions, while vitamin deficiencies (hypovitaminosis) can impair nitric oxide production, reduce vascular health, and negatively affect nerve function, all of which contribute to erectile dysfunction.
In this study, we employed a sex-stratified Mendelian randomization (MR) approach to investigate the potential causal relationships between 18 vitamin-related phenotypes, including vitamin B6, vitamin B12, folate, vitamin C, retinol, and carotene, and the risk of male erectile dysfunction. MR is a method that leverages genetic variants associated with specific exposures (in this case, vitamins) as instrumental variables (IVs) to infer causal effects while minimizing confounding. By utilizing significant single nucleotide polymorphisms (SNPs) as genetic instruments, MR mimics the randomization process of clinical trials, offering a robust way to assess the causal impact of modifiable exposures on health outcomes.
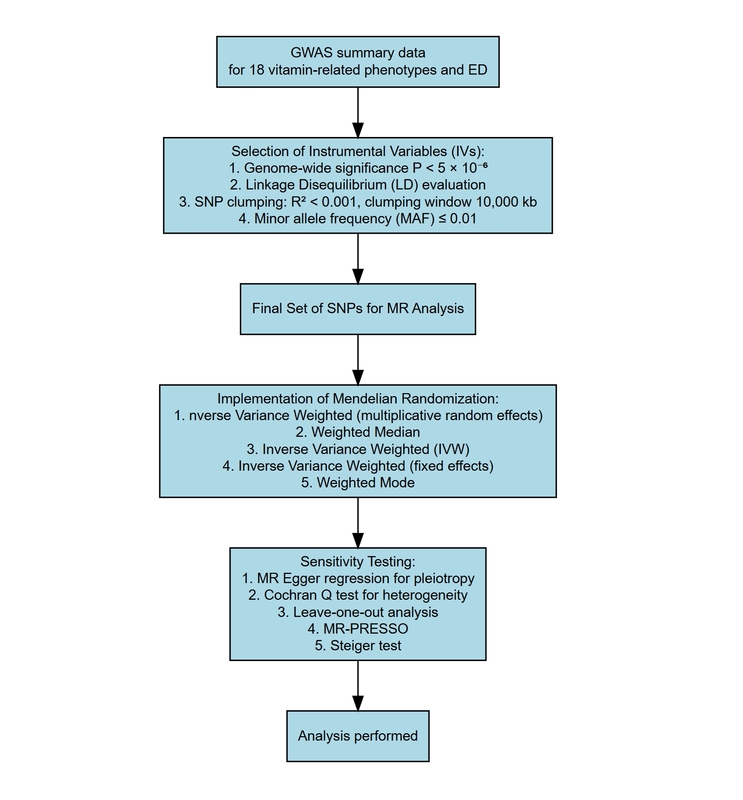
Methods
Data source
All genome-wide association study (GWAS) summary data used in this study were derived exclusively from male participants to ensure the accuracy and relevance of the analysis. The GWAS data for 18 vitamin-related phenotypes were obtained from GWAS round 2 results, provided by the Neale Lab. Detailed information regarding population recruitment criteria and the quality control of the genetic data can be accessed via the Neale Lab website (http://www.nealelab.is/uk-biobank). Detailed descriptions of the vitamin-related phenotypes are available in Supplementary Table SI. Additionally, GWAS summary data for ED were obtained from a separate GWAS study that identified risk loci associated with erectile dysfunction [4]. Although there is some overlap between the populations used in the exposure and outcome GWASs, specific Mendelian randomization methods were applied to minimize the impact of this overlap on the results. As this is a secondary analysis based on publicly available GWAS summary statistics, ethical approval and informed consent for the data collection had been previously obtained in all original studies. No additional ethical approval was required for this secondary analysis.
Instrumental variable selection
Stringent criteria were applied to ensure the appropriate selection of IVs. First, each single nucleotide polymorphism had to exhibit a significant association with one or more of the 18 vitamin-related phenotypes, meeting the genome-wide significance threshold of p < 5 × 10–6. Second, linkage disequilibrium (LD) between SNPs was evaluated using European ancestry data from the 1000 Genomes Project reference panel. To minimize biases related to LD, only the SNPs with the strongest associations were retained, with a threshold of R2 < 0.001 and a clumping window of 10,000 kilobases (kb) applied. Third, SNPs with a minor allele frequency (MAF) ≤ 0.01 were excluded from the analysis to reduce the potential for biases stemming from genetic pleiotropy.
Implementation of Mendelian randomization
Five methods were employed for the MR analysis of the exposure factors: Inverse Variance Weighted (multiplicative random effects), Weighted Median, Inverse Variance Weighted (IVW), Inverse Variance Weighted (fixed effects), and Weighted Mode [5, 6]. Among these, IVW served as the primary method for determining whether significant causal relationships exist between vitamin and ED. These methods were selected because, even in the presence of confounding factors, two-sample MR approaches – including fixed-effect and (multiplicative) random-effects meta-analysis, weighted median estimator, and weighted mode estimator – generally perform comparably to one-sample MR. The Inverse Variance Weighted (multiplicative random effects), used as the primary assessment tool, indicated a causal relationship whose p-values under 0.05 after false discovery rate (FDR) correction.
Sensitivity testing
Causal relationships were evaluated using MR Egger regression and Cochran’s Q test to assess pleiotropy and heterogeneity, respectively, with p-values greater than 0.05 indicating no evidence of horizontal pleiotropy or heterogeneity. Additionally, leave-one-out analysis and Steiger directionality test was used to verify the stability of the results. MR-PRESSO method was employed to rule out horizontal pleiotropy.
The analysis was performed using R (version 4.3.3) and the TwoSampleMR package (version 0.5.9).
Results
A total of 338 single nucleotide polymorphisms were identified as instrumental variables, each with an F-value exceeding 10, indicating strong instrument strength. The number of SNPs per exposure ranged from 7 to 20. Details of these instrumental variables are provided in Supplementary Table SII.
As shown in Figure 1, after FDR correction, Carotene was significantly associated with male erectile dysfunction (OR (95% CI) = 1.58 (1.20–2.09), p = 1.21E-3), and Vitamin D was associated with male erectile dysfunction (OR (95% CI) = 1.40 (1.03–1.91), p = 3.22E-2). After FDR correction, carotene showed a significant association with male erectile dysfunction.
Figure 1
Implementation of Mendelian randomization. A – SNP effect on Vitamin D. B – SNP effect on Carotene. C – MR effect size for Vitamin D on Erectile dysfunction. D – MR effect size for Carotene on Erectile dysfunction
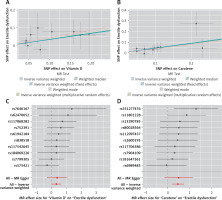
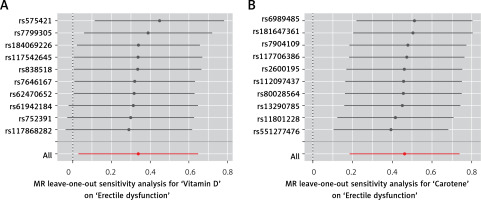
The full results of the Mendelian randomization analyses, including findings from all five MR methods, are provided in Supplementary Table SIII. Sensitivity analyses revealed no evidence of heterogeneity or pleiotropy in this significant finding, as detailed in Supplementary Tables SIV–VII. As shown in Figure 2, the leave-one-out analysis indicated that no single SNP significantly influenced the overall result.
Discussion
Our findings suggest that higher carotene levels was significantly associated with an increased risk of male erectile dysfunction, with an odds ratio of 1.58 (95% CI: 1.20–2.09, p = 1.21 × 10-3) after false discovery rate correction. This indicates that higher carotene levels may play a potential role in the development of ED. Carotene, a precursor to vitamin A, is well-known for its antioxidant properties, which help mitigate oxidative stress [7, 8]. However, while antioxidants are generally considered protective against vascular dysfunction, excessive or imbalanced levels of carotenoids may lead to adverse effects. Some studies have reported that carotene can interfere with the balance of other antioxidant systems or potentially exert pro-oxidant effects under certain conditions, leading to endothelial dysfunction, a key mechanism in ED [9]. The vascular endothelium plays a critical role in penile erection by regulating nitric oxide (NO) production and vasodilation, and any impairment in this pathway may contribute to ED [10]. Our results are consistent with emerging evidence that suggests a non-linear or complex relationship between antioxidant levels and vascular health. Further studies are needed to explore the precise biological mechanisms by which carotene influences erectile function and whether dietary modifications could mitigate this risk. Additionally, recent studies have highlighted the role of vitamin D and the microbiome in modulating immune responses, which may indirectly influence ED risk. Vitamin D deficiency has been linked to immune dysregulation, chronic inflammation, and endothelial dysfunction, all of which are potential contributors to ED. Similarly, the gut microbiome plays a crucial role in maintaining immune homeostasis, and imbalances in microbial composition have been associated with systemic inflammation, oxidative stress, and metabolic disorders [11]. Since immune dysregulation can contribute to vascular and endothelial dysfunction, further studies are needed to explore whether ED patients exhibit signs of immunodepression and how vitamin D and microbiome interactions may influence erectile function. Future research should consider these factors in larger cohorts with immune profiling to better understand their role in ED pathophysiology. And future studies should explore whether dietary modifications or targeted supplementation strategies could help mitigate ED risk while maintaining overall vascular health.
This study has several limitations. First, the GWAS summary statistics used in our Mendelian randomization analysis were derived predominantly from individuals of European ancestry, which may limit the generalizability of our findings to other ethnic populations. Second, due to the nature of summary-level data, we were unable to account for potential confounders such as age, lifestyle factors, or comorbidities, which may influence both vitamin levels and erectile function. Third, although multiple MR methods and sensitivity analyses were used to reduce bias from horizontal pleiotropy and instrument invalidity, the possibility of residual pleiotropy cannot be entirely excluded. Lastly, carotene levels in our analysis reflect genetically predicted exposure rather than actual serum concentrations, and future studies incorporating direct measurements of carotene and longitudinal data are warranted to validate these findings.
In conclusion, our Mendelian randomization study identified a significant association between carotene levels and male erectile dysfunction, suggesting a potential causal relationship. These findings contribute to the growing body of research on nutritional influences on erectile function and highlight the need for further investigation into the mechanisms underlying this association. Future studies should explore the potential clinical implications of carotene intake and whether dietary interventions may mitigate ED risk.