Amniocentesis for fetal cell culture and chromosomal karyotyping is a cornerstone of prenatal screening for high-risk pregnancies. High-risk factors include advanced maternal age (> 35 years), abnormal non-invasive prenatal testing (NIPT) results, ultrasound anomalies, high-risk serological screening, familial chromosomal disorders, and adverse pregnancy histories. Prenatal diagnosis through amniotic fluid analysis, combined with genetic counseling, provides critical insights into fetal chromosomal abnormalities, mitigating the emotional and financial burden of birth defects on families and society.
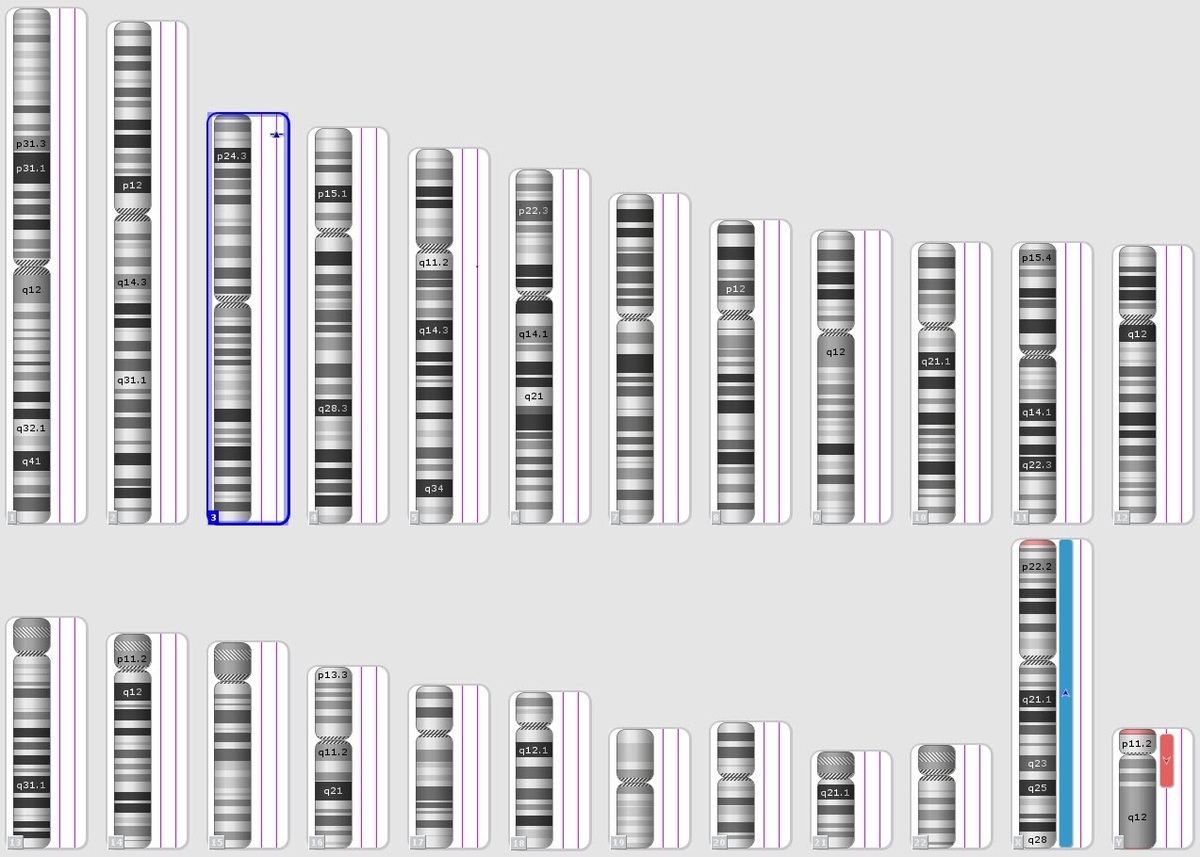
Chromosomal karyotyping, the gold standard for prenatal chromosomal diagnosis, detects significant deletions, duplications, translocations, inversions, and other abnormalities. However, it has limitations, including dependency on cell culture and specimen quality, lengthy processing times, and an inability to detect microdeletions or microduplications smaller than 10 Mb [1]. These challenges underscore the need for integrating karyotyping with advanced diagnostic methods to enhance resolution and efficiency.
Techniques such as fluorescence in situ hybridization (FISH) and quantitative fluorescent polymerase chain reaction (QF-PCR) offer rapid detection of common aneuploidies, such as trisomy 13, trisomy 18, trisomy 21, and sex chromosome abnormalities. However, FISH requires specific probes for rare microdeletions and microduplications [2], while QF-PCR depends on short tandem repeat (STR) markers [3]. BoBs (BACs-on-Beads) technology has shown efficacy in detecting common aneuploidies and at least nine microdeletion and microduplication syndromes [4]. The BoBs assay could be used to detect multiple syndromes caused by these microdeletion regions, which include Angelman syndrome (AS), Prader-Willi syndrome (PWS), DiGeorge syndrome (DGS), Miller-Dieker syndrome (MDS), cri du chat syndrome (CdCS), Wolf-Hirschhorn syndrome (WHS), Smith-Magenis syndrome (SMS), Langer-Giedion syndrome (LGS), and Williams-Beuren syndrome (WBS). Chromosomal microarray analysis (CMA) further enhances detection, identifying abnormalities as small as 100 kb, which are beyond the scope of conventional karyotyping [5]. The integration of karyotyping with BoBs and CMA significantly improves the detection of chromosomal abnormalities, reducing birth defect rates (Table I).
Table I
Differences and advantages of chromosomal karyotyping, BoBs, CMA, FISH and QF-PCR
In this study, we employed a combination of chromosomal karyotyping, BoBs technology, and CMA to analyze amniotic fluid samples from 1,894 pregnant women identified as high-risk based on prenatal screening results. By evaluating the diagnostic outcomes, this study provides valuable insights into the efficacy of various diagnostic methods in prenatal screening and diagnosis. These findings will guide clinicians in tailoring diagnostic strategies to optimize care and outcomes for high-risk pregnancies, ultimately improving patient care and outcomes.
Methods
Subjects
A total of 1894 pregnant women with high-risk factors for chromosomal abnormalities admitted at Weihai Maternity and Child Care Hospital (Weihai, Shandong, China) between January 2022 and February 2023 were enrolled in this study. In this study, the pregnant women or their family members signed informed consent. The indications for prenatal genetic evaluation were advanced maternal age (> 35 years), high-risk NIPT results, abnormal ultrasound, high-risk serological screening results, presence of a chromosomal disorder in one of the spouses, and adverse pregnancy history.
Specimen collection
Guided by B-ultrasound, amniotic fluid samples were taken to obtain information about the fetus’s chromosomes. The gestational age of pregnant women was between 18 and 30 weeks. The procedure was conducted for high-risk patients identified during prenatal examinations.25 ml of amniotic fluid was extracted, 20 ml of which was used for the amniotic fluid cell culture and 5 ml of which was used for the DNA extraction.
Chromosome karyotype analysis
The amniotic cells were cultured, harvested, and treated for chromosome G-banded analysis. For each sample, 20 stained metaphases were examined, and 6 karyograms were created for chromosome analysis.
DNA extraction of samples
The DNA samples were extracted from approximately 5 ml of amniotic fluid using DNA extraction reagents according to the kit’ s handbook (TIANGEN, China).
BoBs assay
A BoBs kit (Perkin Elmer, Waltham, MA, USA) was used for the BoBs assay. The beads were analyzed using a Luminex 200 cytometric acquisition system (Austin, TX, USA) for data collection. Data were analyzed using BoBsoft 1.0 software. Male and female reference samples were used for the internal quality control standards and the comparison standards. The result evaluation criteria: the normal ratio was 1.0. If the ratio was less than 0.8, it indicated that the probe was missing. If the ratio was more than 1.2, it indicated that the probe was repeated. The result suggested a deletion or duplication in the region if there were 3 or more probes in a certain target area exceeding the cut-off of the male and female reference value, which indicated that the region was a deletion or duplication.
CMA assay
Using Affymetrix’s CytoSean750k chip, the amplification, hybridization, scanning, and analysis were performed according to the standard operating procedures of the Infinium HD Assay. ClinGen, ClinVar, DGV, OMIM, DECIPHER and other databases were used for interpretation of results. According to the classification standards recommended by the ACMG (PMID: 31690835), five categories were divided for the clinical determination: pathogenic, likely pathogenic, uncertain significance, likely benign, and benign.
Results
Cell culture results
In the total of 1,894 amniotic fluid samples, the success rate of culturing amniotic fluid cells was 100%. The duration of cell culture harvest ranged from 8 to 10 days on average, with the longest harvest taking up to 15 days. In this study, 1,201 patients with advanced maternal age (> 35 years), 189 patients with abnormal ultrasound, 429 patients with high-risk serological screening results, 10 patients with high-risk NIPT results, 31 patients with adverse pregnancy history, 24 patients with chromosomal disorder, and 10 voluntary patients were included (Supplementary Table SI). Among these cases, 1,700 samples were analyzed using karyotyping and BoBs assay, 99 samples underwent karyotyping and CMA analysis, and 95 samples were subjected to a comprehensive analysis combining karyotyping, BoBs, and CMA. These findings demonstrate the feasibility and efficiency of integrating these diagnostic methods for prenatal chromosomal evaluation.
Chromosomal results detected by karyotyping
Among the 1,894 samples, 54 cases were identified with chromosomal abnormalities, yielding a detection rate of 2.85% (54/1894) (Supplementary Table SI). Among these, 38 cases involved numerical abnormalities, and 16 cases involved structural abnormalities (Table II). The 38 numerical abnormalities included 7 cases of trisomy 18, 23 cases of trisomy 21, 2 cases of 47,XXX, and 4 cases of 47,XXY. Additionally, 2 cases were identified as chimeras, with karyotyping results of 47,XY,+12[28]/46,XY[32] and 47,XXX[6]/46,XX[44]. The 16 structural abnormalities included 4 cases of chromosomal inversions, 8 cases of balanced translocations, and 4 cases of chromosomal deletions. These results highlight the capability of karyotyping to detect both numerical and structural chromosomal anomalies in prenatal diagnostics.
Table II
Abnormal results of chromosome karyotype
| Variable | Karyotype | Case | BoBs | CMA |
|---|---|---|---|---|
| Advanced maternal age | 47,XN,+21 | 10 | 47,XN,+21 | – |
| 47,XN,+18 | 3 | 47,XN,+18 | – | |
| 47,XXY | 2 | 47,XXY | – | |
| 47,XXX | 1 | 47,XXX | – | |
| 46,XX,inv(5)(p12p14) | 1 | 46,XN | – | |
| 46,XX,t(5;11)(q35;q13) | 1 | 46,XN | – | |
| 46,XY,t(2;5)(q21.1;q22) | 1 | 46,XN | – | |
| 46,XY,t(3;10)(p25;q22.1) | 1 | 46,XN | – | |
| 47,XY,+12[28]/46,XY[32] | 1 | 46,XN | – | |
| 46,XY,t(15;17)(q11.2;q11.2) | 1 | 46,XN | – | |
| High-risk NIPT | 47,XN,+21 | 1 | 47,XN,+21 | – |
| 47,XXX | 1 | 47,XXX | – | |
| 47,XXY | 1 | 47,XXY | – | |
| 47,XXX[6]/46,XX[44] | 1 | 46,XN | – | |
| High-risk serological screening | 47,XN,+21 | 8 | 47,XN,+21 | – |
| 46,X,inv(Y)(p11.2q11.2) | 1 | 46,XN | – | |
| 46,XY,t(1;7)(q44;q21.2) | 1 | 46,XN | – | |
| 46,XY,inv(12)(q13q22) | 1 | 46,XN | – | |
| 46,XY,inv(3)(p11.4p14) | 1 | 46,XN | – | |
| 46,XY,del(18)(q22.3) | 1 | 46,XN | 18q22.3q23(72764032-78013728)x1 | |
| 47,XN,+18 | 3 | 47,XN,+18 | – | |
| 46,XX,t(12;20)(q23;q13.2) | 1 | 46,XN | – | |
| Abnormal ultrasound | 47,XXY | 1 | 47,XXY | – |
| 47,XN,+21 | 2 | 47,XN,+21 | – | |
| 45,XY,der(13;14)(q10;q10) | 1 | 46,XN | arr(1-22)x2,(X,N)x1 | |
| 46,XX,der(21)t(14;21)(q24.3;q22.2) | 1 | 46,XN | 14q24.3q32.33(76759640-107284437)x3; 21q22.2q22.3(40187740-48093361)x1 | |
| 48,XXY,+18 | 1 | – | arr(X)x2,(Y)x1,(18)x3 | |
| Chromosomal disorder history from the couples | 46,XY,t(8;11)(q24.1;q21) | 1 | 46,XN | – |
| 45,XY,der(14,21)(q10;q10) | 1 | 46,XN | – | |
| 46,XY,t(1;6)(q12;q21) | 1 | 46,XN | – |
Chromosomal results detected by BoBs assay
Out of the 1,700 samples analyzed using the BoBs assay, 49 cases were identified with chromosomal abnormalities, yielding a detection rate of 2.88% (49/1700) (Tables II and III). Of these, 32 cases exhibited numerical abnormalities involving chromosomes 13, 18, 21, X, and Y, which were consistent with karyotyping findings. Additionally, 7 cases showed chromosome duplication detected by the first probe of Xp22.31, while 1 case was identified with chromosome duplication using the second probe of Xp22.31. Chromosomal deletions were observed in 4 cases using the first probe of Xp22.31, and 1 case was identified with a microdeletion using the third probe of Xp22.31. Furthermore, 4 cases were reported with deletions at 22q11.21 (Table II). All cases with abnormalities detected by BoBs were recommended for CMA analysis to ensure comprehensive evaluation. These results demonstrate the BoBs assay’s reliability in prenatal diagnostics.
Chromosomal results detected by CMA assay
Among the 194 samples analyzed using CMA, 37 cases were identified with chromosomal structural abnormalities. Notably, 1 case had a karyotyping result of 45,XY,der(13;14)(q10;q10), while the CMA analysis revealed a normal chromosomal complement of 46,XN. In addition, 35 cases with normal karyotyping results of 46,XN were found to have chromosomal microdeletions or microduplications detectable only through CMA. These findings highlight the superior sensitivity of CMA in identifying submicroscopic chromosomal abnormalities that are undetectable by conventional karyotyping, emphasizing its importance in comprehensive prenatal chromosomal evaluation.
Discussion
Chromosomal abnormalities are a leading cause of fetal anomalies. With advancements in biological, imaging, and genetic technologies, the accuracy of prenatal screening and diagnosis for chromosomal disorders has markedly improved [6]. Early screening and diagnosis facilitate timely intervention, underscoring the critical role of research in prenatal diagnostics. Currently, serological screening and NIPT are routine methods for detecting chromosomal abnormalities, but with lower accuracy in detecting chromosomal abnormalities compared to karyotyping (Supplementary Tables SII and SIII). Furthermore, the abnormal results of serological screening and NIPT should be detected by karyotyping for prenatal diagnosis [7, 8]. However, karyotyping takes a long time to obtain the results, the culture may fail, and has low detection of microdeletions or microduplications (greater than 10 Mb in size). Therefore, the combination of molecular detection techniques and chromosome karyotyping play an important role in the prenatal examination and screening.
Since 2020, we have introduced the BoBs technique to combine with karyotyping for additional detection of aneuploidies and microdeletions/microduplications in 9 regions. However, the microdeletion/microduplication results detected by BoBs techniques with a single probe were not included in the final diagnostic report. Therefore, CMA technology can detect microdeletions/microduplications of all chromosomes, further making up for the deficiencies of BoBs technology. In this study, we identified 5 microdeletion and 6 microduplication events in the Xp22.31 region by BoBs. CMA confirmed all microdeletion and microduplication results obtained through the BoBs technique in 6 patients (Table III). Previous studies have established that the steroid sulfatase (STS) gene is located in the Xp22.31 region. The duplication of the Xp22.31 fragment has also been linked to developmental delay, autism, language delay, and other clinical phenotypes [9]. In addition, this study identified 3 microduplication events in the 22q11.21 region, with CMA confirming the chromosomal microduplication results initially detected by the BoBs technique (Table III). The 22q11.21 region is known to contribute to conditions such as mental retardation, learning disabilities, and dystonia when duplicated [10]. Notably, all microdeletion/microduplication results detected using single probes in the BoBs assay were corroborated by CMA, underscoring the accuracy and reliability of the BoBs technique [11]. These findings highlight the pivotal role of molecular detection techniques, including BoBs and CMA, in enhancing the accuracy of prenatal diagnostic evaluations.
Table III
Abnormal results of BoBs and CMA detection
Ultrasound diagnostics have been widely adopted for prenatal examinations. Major structural abnormalities identified through fetal ultrasound are frequently associated with chromosomal abnormalities [12]. Therefore, if the ultrasound results of the fetus indicate abnormalities, amniocentesis is used to examine the chromosomes of the fetus. Among these cases, 6 fetuses with abnormal ultrasound findings were confirmed to have chromosomal abnormalities via karyotyping. For example, 3 cases of thickened nuchal translucency (NT) corresponded to karyotypes of 47,XXY and 47,XN,+21. One case with absent nasal bone was associated with a karyotype of 45,XY,der(13;14)(q10;q10) (Table II). Additionally, a case suspected of tetralogy of Fallot exhibited a karyotype of 48,XXY,+18. One fetal growth restriction (FGR) case revealed a karyotype of 46,XX,der(21)t(14;21)(q24.3;q22.2), with CMA detecting a duplication at 14q24.3q32.33(76759640-107284437)x3 and a deletion at 21q22.2q22.3(40187740-48093361)x1.
Notably, 19 cases with abnormal ultrasound findings had normal karyotype results (46,XN), but CMA detected significant microdeletions/microduplications (Table III). This study underscores the vital role of molecular detection techniques, particularly BoBs and CMA, in augmenting the diagnostic capabilities of prenatal evaluations. One notable case involved a fetus with abnormal ultrasound findings, including a double-row “bead-like” pattern of the spine, small lumbar vertebrae, and localized scoliosis. Amniocentesis for chromosomal testing showed normal results for both karyotyping and BoBs, but CMA detected a deletion at 16p11.2 (29,428,532-30,190,029)x1. The 16p11.2 region contains genes such as PRRT2, TBX6, and KCTD13, with mutations in TBX6 associated with spondylocostal dysostosis 5 (SCDS5) [13]. Another case involved a fetus with partial colon and rectal dilation. While karyotyping and BoBs results were normal, CMA revealed a deletion at 16p11.2 (28,748,617-29,088,624)x1. This segment contains TUFM, SH2B1, and ATP2A1 genes [14]. Additionally, a fetus with posterior fossa widening underwent amniocentesis. The karyotyping and BoBs results were normal, but CMA revealed a 280.8 kb deletion at 16q12.1 (47,300,786-47,581,673)x1. This deletion is associated with glycogen storage disease type Ixb [15]. Finally, 1 case involved a fetus with a “honeycomb-like” placental appearance and localized intestinal echogenicity. CMA revealed a deletion at 16q23.2 (81,015,510-81,341,306)x1. This segment contains five OMIM genes, including GCSH and BCO1, which have been associated with intellectual disability, developmental delay, and epilepsy in previous reports.
In this study, two fetuses with thickened NT underwent amniocentesis [16]. While karyotyping and BoBs results were normal, CMA revealed significant findings. One fetus exhibited duplications at 2p12 (80,543,113–81,624,924)x3 and 3q29 (195,262,561–197,851,444)x3, though the clinical significance of these duplications remains unclear. Additionally, a 5.1 Mb deletion at 14q32.31q32.33 (102,099,986–107,284,437)x1 was identified [17]. Another fetus displayed a 482.1 kb deletion at 2q13 (110,498,142–110,980,295)x1, affecting the NPHP1 gene [18]. Furthermore, a fetus with ultrasound findings of abnormal cavum septum pellucidum, suspected corpus callosum agenesis, shortened limbs, and a right aberrant subclavian artery underwent chromosomal analysis. Karyotyping revealed a derivative chromosome 21 due to a translocation between chromosomes 14 and 21 [46,XX,der(21)t(14;21)(q24.3;q22.2)]. CMA identified a 30.5 Mb duplication at 14q24.3q32.33 (76,759,640–107,284,437)x3 and a 7.9 Mb deletion at 21q22.2q22.3 (40,187,740–48,093,361)x1. Two fetuses with FGR underwent amniocentesis. Both had normal karyotyping and BoBs results, but CMA revealed abnormalities. One fetus exhibited a 2.7 Mb duplication at 1q21.1q21.2 (145,146,209–147,933,973)x3, associated with 1q21.1 recurrent region syndrome, which includes phenotypes such as developmental delays, intellectual disabilities, and autism [19]. The other fetus exhibited a 3.4 Mb deletion at 4q35.2 (187,519,399–190,957,460)x1, involving four OMIM genes, including FAT1, ZFP42, and FRG1, which have potential associations with intellectual disabilities, learning difficulties, and facial abnormalities [20]. Based on the above observations, it is necessary to use molecular diagnostics combined with karyotyping to reduce the risk of missing chromosomal abnormalities. During prenatal examinations, when performing amniocentesis for patients with abnormal ultrasound findings, doctors should more strongly recommend that they undergo integration of molecular diagnostics and karyotyping for enhanced detection of chromosomal abnormalities in fetuses.
This study highlights the importance of molecular diagnostic techniques such as CMA and BoBs in detecting submicroscopic chromosomal abnormalities that traditional karyotyping cannot identify. These findings emphasize the necessity of integrating molecular diagnostics into prenatal care for fetuses. The combined use of traditional and molecular techniques provides a comprehensive approach to prenatal diagnosis, enabling accurate diagnosis, genetic counseling, and informed decision-making for parents, ultimately improving the management of pregnancies with chromosomal abnormalities.