Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
DIAGNOSTICS, LABORATORY / CLINICAL RESEARCH
Dynamic serum amyloid A for the prediction of the trajectory of ventilator-associated pneumonia in elderly patients with acute ischemic stroke undergoing endovascular therapy and general anesthesia
1
Department of Anesthesiology, Huai’an Hospital of Huai’an City, Huai’an, Jiangsu Province, China
Submission date: 2025-03-27
Final revision date: 2025-05-26
Acceptance date: 2025-06-12
Online publication date: 2025-06-22
Corresponding author
Yipin Ji
Department of Anesthesiology Huai’an Hospital of Huai’an City Huai’an, 223200 Jiangsu Province, China
Department of Anesthesiology Huai’an Hospital of Huai’an City Huai’an, 223200 Jiangsu Province, China
KEYWORDS
TOPICS
ABSTRACT
Introduction:
In patients with acute ischemic stroke (AIS), current models for predicting ventilator-associated pneumonia (VAP) predominantly rely on multi-parameter approaches, which significantly increase data collection complexity and hinder clinical implementation. Here, we further investigate VAP-related risk factors while dynamically analyzing the predictive value of serum amyloid A (SAA) levels for VAP, aiming to bridge the gap between biomarker-driven simplicity and clinical practicality.
Material and methods:
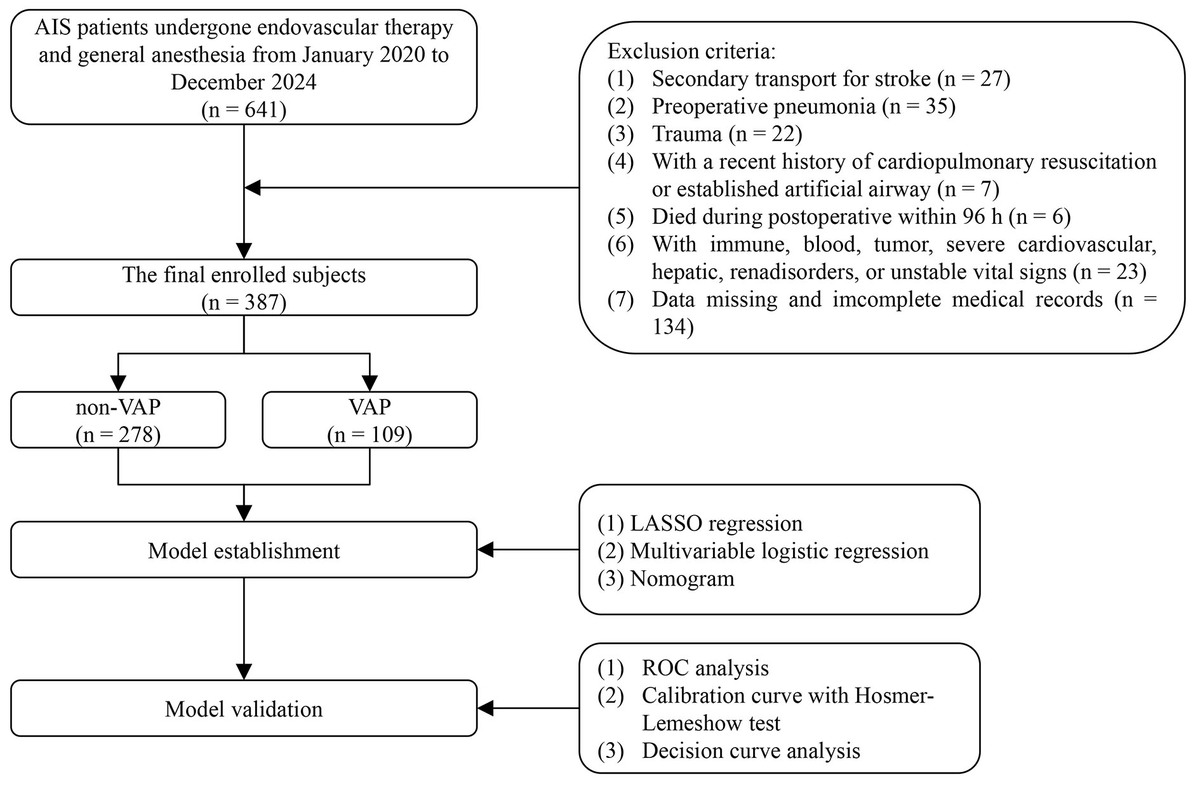
387 patients were ultimately enrolled and divided into two groups: non-VAP (n = 278) and VAP (n = 109). The least absolute shrinkage and selection operator (LASSO), univariate and multivariate logistic regression analyses were utilized to examine the independent risk factors associated with VAP. Calibration and decision curve analysis (DCA) curves were employed to assess the model’s goodness of fit.
Results:
A VAP prediction model incorporating seven multimodal clinical parameters, including age, mechanical ventilation duration, DBP, admission NIHSS score, hs-CRP, TC, and SAA-T2, was developed, achieving exceptional predictive performance with an AUC (95% CI) of 0.961 (0.942–0.980). Based on single-parameter AUC values and DCA, SAA-T2 demonstrated the highest diagnostic efficacy and net clinical benefit. The diagnostic performance of Model 1 and SAA-T2 yielded AUCs (95% CI) of 0.889 (0.853–0.924) and 0.885 (0.842–0.928), respectively, with no statistically significant difference between them. Notably, the addition of SAA-T2 to Model 1 significantly enhanced its diagnostic accuracy for VAP.
Conclusions:
We developed an excellent nomogram model incorporating seven clinical parameters to predict VAP. SAA-T2 may serve as a rapid and practical clinical indicator for predicting VAP in AIS patients, balancing accuracy with clinical feasibility.
In patients with acute ischemic stroke (AIS), current models for predicting ventilator-associated pneumonia (VAP) predominantly rely on multi-parameter approaches, which significantly increase data collection complexity and hinder clinical implementation. Here, we further investigate VAP-related risk factors while dynamically analyzing the predictive value of serum amyloid A (SAA) levels for VAP, aiming to bridge the gap between biomarker-driven simplicity and clinical practicality.
Material and methods:
387 patients were ultimately enrolled and divided into two groups: non-VAP (n = 278) and VAP (n = 109). The least absolute shrinkage and selection operator (LASSO), univariate and multivariate logistic regression analyses were utilized to examine the independent risk factors associated with VAP. Calibration and decision curve analysis (DCA) curves were employed to assess the model’s goodness of fit.
Results:
A VAP prediction model incorporating seven multimodal clinical parameters, including age, mechanical ventilation duration, DBP, admission NIHSS score, hs-CRP, TC, and SAA-T2, was developed, achieving exceptional predictive performance with an AUC (95% CI) of 0.961 (0.942–0.980). Based on single-parameter AUC values and DCA, SAA-T2 demonstrated the highest diagnostic efficacy and net clinical benefit. The diagnostic performance of Model 1 and SAA-T2 yielded AUCs (95% CI) of 0.889 (0.853–0.924) and 0.885 (0.842–0.928), respectively, with no statistically significant difference between them. Notably, the addition of SAA-T2 to Model 1 significantly enhanced its diagnostic accuracy for VAP.
Conclusions:
We developed an excellent nomogram model incorporating seven clinical parameters to predict VAP. SAA-T2 may serve as a rapid and practical clinical indicator for predicting VAP in AIS patients, balancing accuracy with clinical feasibility.
REFERENCES (29)
1.
Yang S, Li K, Huang Z, et al. Risk factors of acute ischemic stroke and the role of angiotensin I in predicting prognosis of patients undergoing endovascular thrombectomy. Front Endocrinol (Lausanne) 2024; 15: 1388871.
2.
Zhu H, Liang W, Zhu J, et al. Nomogram to predict ventilator-associated pneumonia in large vessel occlusion stroke after endovascular treatment: a retrospective study. Front Neurol 2024; 15: 1351458.
3.
Metersky ML, Kalil AC. Management of ventilator-associated pneumonia: guidelines. Infect Dis Clin North Am 2024; 38: 87-101.
4.
Frondelius T, Atkova I, Miettunen J, Rello J, Jansson MM. Diagnostic and prognostic prediction models in ventilator-associated pneumonia: systematic review and meta-analysis of prediction modelling studies. J Crit Care 2022; 67: 44-56.
5.
Shi Y, Huang Y, Zhang TT, et al. Chinese guidelines for the diagnosis and treatment of hospital-acquired pneumonia and ventilator-associated pneumonia in adults (2018 Edition). J Thorac Dis 2019; 11: 2581-616.
6.
Fernando SM, Tran A, Cheng W, et al. Diagnosis of ventilator-associated pneumonia in critically ill adult patients-a systematic review and meta-analysis. Intensive Care Med 2020; 46: 1170-9.
7.
Frondelius T, Atkova I, Miettunen J, et al. Early prediction of ventilator-associated pneumonia with machine learning models: a systematic review and meta-analysis of prediction model performance. Eur J Intern Med 2024; 121: 76-87.
8.
Li S, Shang L, Han X, Kang H, Li W. Construction and validation of a predictive model for the risk of ventilator-associated pneumonia in elderly ICU patients. Can Respir J 2023; 2023: 7665184.
9.
Lin Q, Fu F, Shen L, Zhu B. Pentraxin 3 in the assessment of ventilator-associated pneumonia: an early marker of severity. Heart Lung 2013; 42: 139-45.
10.
Bilgin H, Haliloglu M, Yaman A, et al. Sequential measurements of pentraxin 3 serum levels in patients with ventilator-associated pneumonia: a nested case-control study. Can J Infect Dis Med Microbiol 2018; 2018: 4074169.
11.
Howroyd F, Chacko C, MacDuff A, et al. Ventilator-associated pneumonia: pathobiological heterogeneity and diagnostic challenges. Nat Commun 2024; 15: 6447.
12.
Yeh SJ, Chen CH, Lin YH, et al. Serum amyloid A predicts poor functional outcome in patients with ischemic stroke receiving endovascular thrombectomy: a case control study. J Neurointerv Surg 2023; 15: 75-81.
13.
Saiki O, Uda H. Ratio of serum amyloid A to C-reactive protein is constant in the same patients but differs greatly between patients with inflammatory diseases. Scand J Immunol 2022; 95: e13121.
14.
Li L, Liu H, Zhang Q, et al. Serum amyloid A and risks of all-cause and cardiovascular mortality in chronic kidney disease: a systematic review and dose-response meta-analysis. Ren Fail 2023; 45: 2250877.
15.
Huang XB, Zhao S, Liu ZY, Xu YY, Deng F. Serum amyloid A as a biomarker for immunoglobulin resistance in Kawasaki disease. Ann Med 2023; 55: 2264315.
16.
Shridas P, Patrick AC, Tannock LR. Role of serum amyloid A in abdominal aortic aneurysm and related cardiovascular diseases. Biomolecules 2021; 11: 1883.
17.
Zhang Y, Feng Y, Zuo J, et al. Elevated serum amyloid A is associated with cognitive impairment in ischemic stroke patients. Front Neurol 2021; 12: 789204.
18.
Chang Q, Li Y, Xue M, et al. Serum amyloid A is a potential predictor of prognosis in acute ischemic stroke patients after intravenous thrombolysis. Front Neurol 2023; 14: 1219604.
19.
Zhang P, Han R, Zhang A, et al. Association between serum amyloid A level and white matter hyperintensity burden: a cross-sectional analysis in patients with acute ischemic stroke. Neurol Ther 2023; 12: 161-75.
20.
Schweizer J, Bustamante A, Lapierre-Fétaud V, et al. SAA (serum amyloid A): a novel predictor of stroke-associated infections. Stroke 2020; 51: 3523-30.
21.
Gil LA, Krattinger-Turbatu L, Schweizer J, Katan M, Sanchez JC. A panel comprising serum amyloid a, white blood cells and nihss for the triage of patients at low risk of post-stroke infection. Diagnostics (Basel) 2021; 11: 1070.
22.
Abo-Hagar HH, Abo-Elezz AAE, Mehrez M, Mabrouk MM, Elshora OA. Diagnostic efficacy of serum amyloid A protein and soluble intercellular adhesion molecule 1 in pediatric ventilator-associated pneumonia. J Intensive Care Med 2019; 34: 503-10.
23.
Lin J, Kang Z, Lin Y, Han L, Li S. Predictive values of serum amyloid A, toll-like receptor 4, and sTREM-1 for ventilator-associated pneumonia in elderly patients undergoing abdominal surgery with tracheal intubation and general anesthesia. World J Surg 2024; 48: 2383-90.
24.
Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2018; 49: e46-110.
25.
Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ 2015; 350: g7594.
26.
Li Y, Liu C, Xiao W, Song T, Wang S. Incidence, risk factors, and outcomes of ventilator-associated pneumonia in traumatic brain injury: a meta-analysis. Neurocrit Care 2020; 32: 272-85.
27.
Patel UK, Kodumuri N, Dave M, et al. Stroke-associated pneumonia: a retrospective study of risk factors and outcomes. Neurologist 2020; 25: 39-48.
28.
Li S, Shang L. Construction and validation of a predictive model for the risk of ventilator-associated pneumonia in elderly ICU patients. Can Respir J 2023; 2023: 7665184.
29.
Pelosi P, Barassi A, Severgnini P, et al. Prognostic role of clinical and laboratory criteria to identify early ventilator-associated pneumonia in brain injury. Chest 2008; 134: 101-8.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.