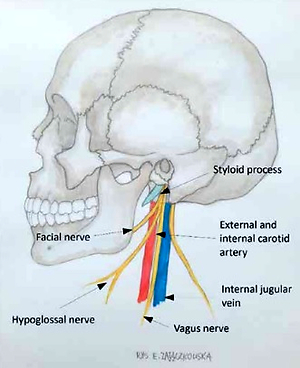
Eagle syndrome (ES) is a rare (4–8/10,000) condition characterized by an abnormally elongated styloid process (SP) with/without abnormal direction and/or ossification of the styloid ligament (SL). Among the spectrum of symptoms, the most frequent are related to pain: throat and neck with radiation to the ear, and unilateral headache. Odynophagia, dysphagia, foreign body sensation in the throat, and tinnitus can be frequent. Eye pain with visual disturbances and syncope are reported. They may be due to internal carotid artery (ICA) compression or dissection as the cause of ischemic stroke [1]. There are two types of ES. Type 1 is diagnosed with ipsilateral headache, odynophagia, dysphagia, and foreign body sensation in the pharynx. An elongated SP impinges on cranial nerves (V, VII, IX, X). Type 2, carotid, is connected with compression or dissection of the ICA, and neck pain is typical. In this variant, known as stylocarotid artery syndrome (SAS), the elongated SP compresses or protrudes into the ICA (Figure 1), causing transient neurologic symptoms, including transient ischemic attacks (TIA) and stroke [2, 3]. Therefore, identification of the cause and diagnosis of the underlying disease are often delayed [4]. Surgery (styloidectomy) is indicated in cases of refractory pain where other methods, including pharmacological treatment, have failed but it seems to be a necessary procedure in the diagnosis of pressure and/or dissection of the ICA. At present, there is no expert consensus or treatment guidelines for the disease. ES is classified in the ICHD-3 (as 11.8) [5]. Its description includes unilateral headache, with neck, pharyngeal, and/or facial pain, caused by inflammation of the SL and usually provoked or exacerbated by a head twist.
We present 3 patients (Table I) hospitalized in the Department of Neurology, diagnosed with ES type 2. In all of them, headache and neck pain were the main symptoms of ES as a risk factor for stroke (compression and dissection of ICA), so they underwent preventive surgery.
Table I
Demographic, clinical, and radiological data from our series of patients with ES type 2
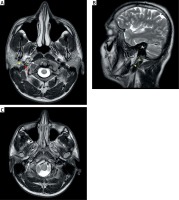
A 34-year-old man was admitted due to a dull headache, intense in the morning, on the right side, radiating to the right eye, which started a few days earlier for no apparent reason. In an examination, mild Horner’s syndrome on the right side and asymmetry of tendon reflexes were detected. After the ES diagnosis (see MRI of the brain – Figure 2), resection of the styloids was performed. Control Doppler ultrasound examination showed a visible improvement – the flow in the intracerebral vessels was without any abnormalities. In a neurological examination, no significant deviations were observed.
Figure 2
Magnetic resonance imaging of case 1 with sequence T2. A – White arrow – visible stratified right ICA in the cross-section over a 10 mm segment; Red arrow – narrowed jugular vein against the background of pressure by the styloid-hyoid ligament; Yellow arrow – styloid process and its extension, the styloid-hyoid ligament. B – Yellow arrow – styloid process and its extension – styloid-hyoid ligament. C – White arrow – stratified RICA, calcifications within the hyoid stylus ligament, on both sides, which on the right side are adjacent to the RICA, and the possibility of isthmus syndrome of the above-mentioned structures were taken into account
A 44-year-old woman was admitted due to right internal carotid artery (RICA) dissection identified in the ambulatory magnetic resonance imaging (MRI), performed because of headaches in the temporal area on the right side, pulsating, lasting a few seconds, occurring several to ten times a day. The patient fell downstairs some weeks before with subsequent short-term pain in the neck. No abnormalities were found in a general/neurological examination.
A 41-year-old man was admitted with a headache radiating from the neck’s right side, followed by a few minutes of right-sided numbness, which started during training, possibly with a neck injury. Transient right-sided Horner’s syndrome was found in a neurological examination. In the angio-CT RICA dissection and thrombosis were suspected, due to the unclear image with the obstruction of the artery and its compression by the SP.
ES was initially described in 1937 by W.W. Eagle, as facial, neck, and laryngeal pain associated with elongation of the ipsilateral SP, with or without calcification of the SL. The length of the SP ranges from 25 to 30 mm and is elongated in 4–7% of the population [4], usually asymptomatic (up to 30%), and symptomatic, as we mentioned aboved – in about 4% to 10%. Between the external and ICA lies the clinically important apex of the SP, as in our patients. Symptoms due to the elongated SP are believed to be caused by direct pressure of the SP on the nearby facial nerves and vessels – the external and ICAs. ES may cause ICA disease (especially after a trauma targeted to the neck as in our cases 2 and 3), including vessel stenosis and artery dissection, and pseudoaneurysm may be complicated by cerebrovascular events or may be an indirect cause of stroke. In our patients, ES was responsible for stenosis of the ICA associated with compression (cases 1 and 3) and dissection (cases 1 and 2), so our diagnosis and consecutive treatment were stroke and TIA prevention in young patients.