Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
HEMATOLOGY / BASIC RESEARCH
Effect and mechanism of immune surveillance activated by autotransfusion on reducing liver cancer metastasis based on HLA-DQB1/PDCD1
1
Ningxia Medical University, Ningxia, China
2
Postgraduate Training Base in Shanghai Gongli Hospital, Ningxia Medical University, Shanghai, China
3
Graduate School of Wannan Medical College, Anhui, China
4
Department of Anesthesiology, Shanghai Gongli Hospital, Naval Military Medical University, Shanghai, China
5
Department of Anesthesiology, Lihuili Hospital, Medical School of Ningbo University, Zhejiang, China
Submission date: 2022-03-23
Final revision date: 2022-06-01
Acceptance date: 2022-06-18
Online publication date: 2022-07-18
Corresponding author
Jian-Rong Guo
Department of Anesthesiology, Shanghai Gongli Hospital, Naval Military Medical University, Shanghai 200135, China., China
Department of Anesthesiology, Shanghai Gongli Hospital, Naval Military Medical University, Shanghai 200135, China., China
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Liver cancer is a common tumor of the digestive system. Hepatectomy sometimes results in massive hemorrhage, and intraoperative autotransfusion is often required.
Material and methods:
In this basic research, a liver cancer mouse model was established, the visible liver cancer tissue was surgically removed, and the blood of the mice was recovered.
Results:
The results showed that the model group had the highest recurrence and metastasis of liver cancer, and the lowest was the autotransfusion group. Flow cytometry showed that the number of HLA-DQB1 positive cells, the content of CD4+CD25+T cells, and the proliferation of CD4+T cells were the highest in the autotransfusion group, followed by the model group, and the lowest in the auto+HLA-DQB1 group, which showed no difference from the control group. Immunohistochemistry and western blot analysis showed that the lowest expression of PDCD1 protein was in the autotransfusion group, which showed no significant difference from the control group, and the highest expression was in auto-HLA-DQB1, followed by the model group.
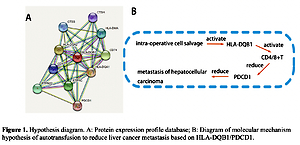
Conclusions:
The study elucidates the molecular mechanism whereby autotransfusion will activate up-regulated expression of the signal molecule HLA-DQB1, enhance the immune surveillance of CD4+T cells, reduce the expression of PDCD1 on the surface molecule of liver cancer cells, and inhibit liver cancer metastasis.
Liver cancer is a common tumor of the digestive system. Hepatectomy sometimes results in massive hemorrhage, and intraoperative autotransfusion is often required.
Material and methods:
In this basic research, a liver cancer mouse model was established, the visible liver cancer tissue was surgically removed, and the blood of the mice was recovered.
Results:
The results showed that the model group had the highest recurrence and metastasis of liver cancer, and the lowest was the autotransfusion group. Flow cytometry showed that the number of HLA-DQB1 positive cells, the content of CD4+CD25+T cells, and the proliferation of CD4+T cells were the highest in the autotransfusion group, followed by the model group, and the lowest in the auto+HLA-DQB1 group, which showed no difference from the control group. Immunohistochemistry and western blot analysis showed that the lowest expression of PDCD1 protein was in the autotransfusion group, which showed no significant difference from the control group, and the highest expression was in auto-HLA-DQB1, followed by the model group.
Conclusions:
The study elucidates the molecular mechanism whereby autotransfusion will activate up-regulated expression of the signal molecule HLA-DQB1, enhance the immune surveillance of CD4+T cells, reduce the expression of PDCD1 on the surface molecule of liver cancer cells, and inhibit liver cancer metastasis.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.