Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
METABOLIC SYNDROME / RESEARCH PAPER
Coexistence of low testosterone and metabolic syndrome associated with increased arterial stiffness in male patients with type 2 diabetes
1
Division of Endocrinology and Metabolism, Department of Internal Medicine, Mackay Memorial Hospital, Taipei, Taiwan
2
Department of Medicine, Mackay Medical College, Taipei, Taiwan, Taiwan
3
Mackay Junior College of Medicine, Nursing, and Management, Taipei, Taiwan, Taiwan
4
Division of Endocrinology and Metabolism, Department of Internal Medicine, Mackay Memorial Hospital, Taitung, Taiwan
5
Division of Nephrology, Department of Internal Medicine, Mackay Memorial Hospital, Taipei, Taiwan
6
Graduate Institute of Physiology, College of Medicine, National Taiwan University, Taipei, Taiwani, Taiwan
Submission date: 2022-04-22
Final revision date: 2022-07-05
Acceptance date: 2022-07-17
Online publication date: 2022-07-18
Corresponding author
Sung-Chen Liu
Division of Endocrinology and Metabolism, Department of Internal Medicine, Mackay Memorial Hospital, Taipei, Zhongshan N. Rd, No. 92, Sec. 2, ,, 10449, Taipei, Taiwan
Division of Endocrinology and Metabolism, Department of Internal Medicine, Mackay Memorial Hospital, Taipei, Zhongshan N. Rd, No. 92, Sec. 2, ,, 10449, Taipei, Taiwan
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Male patients with type 2 diabetes (T2D) have a high prevalence of low testosterone (LT) or metabolic syndrome (MetS). While LT or MetS are associated with arterial stiffness, few studies have investigated the effect of these conditions when manifested together. Our study was performed to explore the influence of coexistence of LT and MetS on arterial stiffness in male patients with T2DM.
Material and methods:
We recruited 332 male patients with T2D at the endocrine and metabolic clinic of the Taitung branch of the Mackay Memorial hospital. Subjects were divided according to the presence of LT or MetS as follows: normal (neither condition present), LT only, MetS only and the coexistence of LT and MetS. All enrolled subjects consecutively underwent brachial-ankle pulse wave velocity (PWV) to evaluate arterial stiffness.
Results:
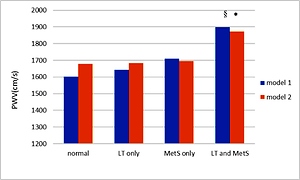
Patients with LT have a higher prevalence of MetS than those without LT (80.1% vs. 64.2%; P=0.03). Age, weight, triglycerides and PWV were significantly higher in patients with coexisting LT and MetS than in the groups with LT or MetS alone. Multiple linear regression analysis was performed to demonstrate that PWV was significantly positively associated with age (P <0.001), SBP (P=0.002) and triglycerides (P=0.001) and negatively associated with testosterone (P=0.039). ANCOVA analysis revealed that PWV remained highest in patients with coexisting MetS and LT compared to the other groups, even after adjusting for confounding factors.
Conclusions:
In our study, the coexistence of MetS and LT was significantly associated with a high risk of increased arterial stiffness in male patients with T2D.
Male patients with type 2 diabetes (T2D) have a high prevalence of low testosterone (LT) or metabolic syndrome (MetS). While LT or MetS are associated with arterial stiffness, few studies have investigated the effect of these conditions when manifested together. Our study was performed to explore the influence of coexistence of LT and MetS on arterial stiffness in male patients with T2DM.
Material and methods:
We recruited 332 male patients with T2D at the endocrine and metabolic clinic of the Taitung branch of the Mackay Memorial hospital. Subjects were divided according to the presence of LT or MetS as follows: normal (neither condition present), LT only, MetS only and the coexistence of LT and MetS. All enrolled subjects consecutively underwent brachial-ankle pulse wave velocity (PWV) to evaluate arterial stiffness.
Results:
Patients with LT have a higher prevalence of MetS than those without LT (80.1% vs. 64.2%; P=0.03). Age, weight, triglycerides and PWV were significantly higher in patients with coexisting LT and MetS than in the groups with LT or MetS alone. Multiple linear regression analysis was performed to demonstrate that PWV was significantly positively associated with age (P <0.001), SBP (P=0.002) and triglycerides (P=0.001) and negatively associated with testosterone (P=0.039). ANCOVA analysis revealed that PWV remained highest in patients with coexisting MetS and LT compared to the other groups, even after adjusting for confounding factors.
Conclusions:
In our study, the coexistence of MetS and LT was significantly associated with a high risk of increased arterial stiffness in male patients with T2D.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.