Introduction
Hypertension, once defined as systolic and/or diastolic blood pressure (SBP/DBP) ≥ 140/90 mm Hg [1, 2], is a major risk factor for cardiovascular disease and all-cause mortality. Prior studies have consistently shown that BP levels were positively associated with cardiovascular risks [3–6]. Furthermore, meta-analysis and randomized controlled trials have also demonstrated that decreasing BP with antihypertensive medications is beneficial for reducing cardiovascular events and all-cause mortality [3, 7–10].
In the last year, the American College of Cardiology and American Heart Association (ACC/AHA) issued a new Hypertension Guideline which recommends that the cutoff value to diagnose hypertension should be with SBP and/or DBP ≥ 130/80 mm Hg [11]. Indeed, the SPRINT trial has shown that compared to patients with a therapeutic BP goal of 140/90 mm Hg, patients with a therapeutic BP goal of 120/80 mm Hg had lower incidence of cardiovascular events and all-cause mortality [7, 12], indicating that a lower therapeutic BP goal is better than the traditional BP goal. However, a slightly higher risk of acute kidney injury and falling down was also observed in the low therapeutic BP goal group.
The evidence used in the new ACC/AHA Hypertension Guideline was predominantly derived from Caucasian populations, and whether this recommendation could be applied to Chinese hypertensive patients is unknown. In addition, compared to the Caucasian populations, the Chinese hypertensive patients were more likely to have a lower body weight index and be physically inactive [13–15]. Furthermore, epidemiological studies have shown that Chinese hypertensive patients were more likely to experience ischemic stroke than ischemic heart disease [16, 17]. Therefore, it is necessary to investigate the association of different therapeutic BP goals and cardiovascular outcomes as well as potential adverse events in Chinese hypertensive patients.
In the current study, using a retrospective design, we compared the associations of different therapeutic BP goals and cardiovascular outcomes. Data from our current study can provide foundations for randomized controlled trials aiming to evaluate the optimal therapeutic BP goal for Chinese hypertensive patients in the future.
Material and methods
Study design and participants’ enrollment
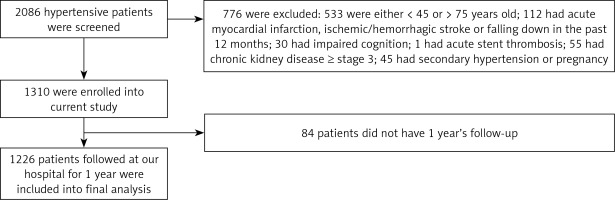
This was a retrospective observational study and the current study was approved by the Clinical Research Ethic Committee of Linyi People’s Hospital. Since this study has a retrospective design, no informed consent was required. All participants were screened and recruited from the outpatient clinic system from January 2016 to January 2017. The inclusion criteria were as follows: age 45–75 years old and patients were followed at an outpatient clinic for at least 1 year. The exclusion criteria were as follows: had acute myocardial infarction or ischemic/hemorrhagic stroke, or bone fracture due to falling down in the past 12 months; had documented cognitive impairment, chronic kidney disease ≥ stage 3, secondary hypertension or pregnancy.
Data collection
The demographics such as age, gender and body mass index (BMI) were collected from outpatient electronic health record (EHR). Body mass index was calculated by weight in kilograms divided by height in squared meters. Prior medical histories and comorbidities were also collected from the outpatient EHR. At baseline, fasting blood samples were drawn to evaluate lipid profiles, fasting plasma glucose (FPG), glycated hemoglobin A1c (HbA1c) and serum creatinine level, which was used to calculate glomerular filtration rate (GFR) in accordance with the Modification of Diet in Renal Disease (MDRD) formula [18].
Blood pressure measurements
Blood pressure measurements at the outpatient clinic were conducted based on the JNC7 guideline recommendation [19]. No smoking or caffeine-containing beverage consumption was allowed within 1 h before BP measurements. Patients sat quietly for 10 min with their back supported before BP measurements and arms were placed at heart level. The non-dominant arm was used to measure BP 3 times with a 1-minute interval between each measurement. The physician was out of office during BP measurement. The average value of the last two BP readings was considered as the clinic BP value.
Study endpoints
All participants who had at least 1-year follow-up at an outpatient clinic were included in the analysis. Study endpoints included composite of all-cause mortality, non-fatal myocardial infarction, and non-fatal ischemic stroke/transient ischemic attack (TIA); and adverse event was defined as falling down due to hypotension or orthostatic hypotension. In addition, GFR at follow-up was also compared. All the events were adjudicated by two experienced and independent physicians.
Statistical analysis
Continuous data were presented as mean ± standard deviation (SD) or median (inter-quartile range – IQR) and were compared by the Student t-test when data were normally distributed; otherwise they were compared by the Wilcoxon rank-sum test. Categorical data were presented as number (proportion) and were compared by the χ2 test or Fisher’s exact test as appropriate. The association of different therapeutic BP goals and study endpoints was evaluated by Cox proportional regression analysis. All reported p-values were 2-sided, and a p-value of < 0.05 was considered statistically significant. All statistical analyses were conducted with the SPSS statistical package for Windows version 19.0 (SPSS Inc., Chicago, Illinois).
Results
Participants’ enrollment
A total of 2086 hypertensive patients were screened during January of 2016 to January of 2017 and 776 patients were excluded due to existing exclusion criteria, and 1310 patients were enrolled in the current study and 84 patients did not have 1 year’s follow-up; therefore, 1226 patients were included in the final analysis (Figure 1). Based on therapeutic BP goal levels, all participants were divided into 3 groups, namely low (< 130/80 mm Hg) and high (< 140/90 mm Hg) therapeutic BP goal groups and the uncontrolled hypertension (≥ 140/90 mm Hg) group.
Comparison of baseline characteristics
As shown in Table I, a total of 366 (29.9%) and 570 (46.5%) patients in our study had achieved SBP/DBP < 130/80 mm Hg and SBP/DBP < 140/90 mm Hg during 1 year’s follow-up, respectively. Compared to patients in the low therapeutic goal group, patients in the uncontrolled hypertension group (SBP/DBP ≥ 140/90 mm Hg) were older and more likely to be current smokers, have longer duration of hypertension, diabetes mellitus, lower GFR and prevalent ischemic stroke at baseline (p < 0.05 for all comparisons), indicating that patients in the uncontrolled hypertension group had more comorbidities. No significant differences between high therapeutic goal and uncontrolled hypertension groups were observed.
Table I
Comparison of baseline characteristics
| Variables | < 130/80 mm Hg (n = 366) | < 140/90 mm Hg (n = 570) | ≥ 140/90 mm Hg (n = 290) |
|---|---|---|---|
| Age [years] | 56.3 ±9.2 | 59.2 ±10.4 | 62.5 ±11.2* |
| Male, n (%) | 195 (53.3) | 308 (54) | 157 (54.1) |
| Body mass index [kg/m2] | 24.4 ±4.9 | 25.6 ±4.5 | 25.0 ±4.2 |
| Systolic blood pressure [mm Hg] | 148 ±7 | 152 ±6 | 158 ±13* |
| Diastolic blood pressure [mm Hg] | 84 ±10 | 91 ±12 | 99 ±11* |
| Current smokers, n (%) | 106 (29) | 174 (30.5) | 102 (35.2)* |
| Dyslipidemia, n (%) | 124 (33.9) | 196 (34.4) | 100 (34.5) |
| Diabetes mellitus, n (%) | 130 (35.6) | 208 (36.5) | 117 (40.3)* |
| Hypertension duration [years] | 8.4 ±3.0 | 8.9 ±2.9 | 9.7 ±3.4* |
| Total cholesterol [mmol/l] | 5.0 ±0.7 | 5.1 ±0.4 | 5.1 ±0.6 |
| Triglyceride [mmol/l]# | 1.08 (0.75–2.11) | 1.12 (0.94–2.16) | 1.1 (0.83–2.19) |
| Fasting plasma glucose [mmol/l] | 5.8 ±0.8 | 5.9 ±1.0 | 5.8 ±0.9 |
| Glycated hemoglobin A1c (%) | 6.3 ±1.0 | 6.2 ±1.1 | 6.1 ±1.2 |
| Creatinine [µmol/l] | 70.3 ±26.7 | 72.5 ±23.6 | 74.8 ±27.7 |
| Glomerular filtration rate [ml/min/1.73 m2] | 79.2 ±10.7 | 76.1 ±12.3 | 74.3 ±10.8* |
| Ischemic stroke, n (%) | 93 (26.2) | 157 (27.5) | 90 (31.0)* |
| Coronary artery disease, n (%) | 40 (10.9) | 67 (11.8) | 31 (10.7) |
| Chronic heart failure, n (%) | 25 (6.8) | 40 (7.0) | 21 (7.2) |
| Peripheral vascular disease, n (%) | 32 (8.7) | 51 (8.9) | 27 (9.3) |
Comparison of medications
Medications used at follow-up were compared between groups. As presented in Table II, compared to patients in the low therapeutic goal group, patients with uncontrolled hypertension were more likely to have antiplatelet and statins treatment. In addition, the use of antihypertensive medications and the mean number of antihypertensive medications were also higher in the uncontrolled hypertension group, which might be due to more comorbidities and more severe hypertension in the uncontrolled hypertension group.
Table II
Use of medications at follow-up
| Medications | < 130/80 mm Hg (n = 366) | < 140/90 mm Hg (n = 570) | ≥ 140/90 mm Hg (n = 290) |
|---|---|---|---|
| Antiplatelet, n (%) | 185 (50.5) | 293 (51.4) | 166 (57.2)* |
| Statins, n (%) | 168 (45.9) | 285 (50) | 163 (56.2)* |
| ACEI/ARB, n (%) | 282 (77) | 456 (80) | 243 (83.8)* |
| β-Blocker, n (%) | 103 (28.1) | 166 (29.1) | 120 (41.4)* |
| Calcium channel blocker, n (%) | 115 (31.4) | 160 (28.1) | 112 (38.6)* |
| Diuretic, n (%) | 70 (19.1) | 105 (18.4) | 95 (32.8)* |
| Number of anti-hypertensive drugs | 2.3 ±0.6 | 2.5 ±0.5 | 2.9 ±0.7* |
| Oral hypoglycemic drugs, n (%) | 96 (26.2) | 178 (31.2) | 89 (30.7) |
| Insulin, n (%) | 23 (6.3) | 30 (5.3) | 20 (6.9) |
| Blood pressure at follow-up [mm Hg]: | |||
| Systolic blood pressure | 122 ±6 | 131 ±8 | 150 ±7* |
| Diastolic blood pressure | 70 ±8 | 82 ±6 | 95 ±5* |
Comparison of study endpoints and adverse events
During 1 year’s follow-up, study endpoints and adverse events were compared. As shown in Table III, compared to the low and high therapeutic goal groups, patients in the uncontrolled hypertension group had higher incidence of composite endpoints, which was driven by a higher incidence of ischemic stroke/TIA. In addition, GFR remained lower in the uncontrolled hypertension group compared to the low therapeutic goal group. However, no significant differences were observed when compared to baseline GFR within each individual group. Two cases of falling down were observed in the low therapeutic goal group compared to 1 case in the uncontrolled hypertension group. A slightly lower incidence of study endpoints was observed in the low versus high therapeutic goal group, but no statistical significance was observed.
Table III
Comparison of study endpoints and adverse events
| Study endpoints | < 130/80 mm Hg (n = 366) | < 140/90 mm Hg (n = 570) | ≥ 140/90 mm Hg (n = 290) |
|---|---|---|---|
| All-cause mortality, n (%) | 0 | 0 | 1 (0.3) |
| Non-fatal MI, n (%) | 2 (0.5) | 8 (1.4) | 6 (2.1) |
| Ischemic stroke/TIA, n (%) | 5 (1.4) | 12 (2.1) | 11 (3.8)*# |
| Composite, n (%) | 7 (1.9) | 20 (3.5) | 18 (6.2)*# |
| Falling down, n (%) | 2 (0.5) | 0 | 1 (0.3) |
| GFR [ml/min/1.73 m2] | 78.0 ±9.6 | 75.4 ±11.2 | 73.4 ±10.1* |
Cox proportional regression analysis
As presented in Table IV, in the unadjusted model, compared to the low therapeutic goal group (reference group), the hazard ratio for composite endpoints during 1 year’s follow-up was 1.16 and 1.37 in the high therapeutic goal group and uncontrolled hypertension group. With stepwise adjustment for potential confounding factors, the uncontrolled hypertension group still had nearly 12% higher risk of composite endpoints, with a 95% confidence interval of 4–21%. In addition, compared to the high therapeutic goal group, patients in the uncontrolled hypertension group also had a 6% higher risk of experiencing composite endpoints, with a 95% confidence interval of 2–17%. Compared to the high therapeutic goal group, although patients in the low therapeutic group had low risk of composite endpoints, the risk was attenuated into statistical insignificance after adjustment for confounding factors.
Table IV
Cox proportional regression analysis
[i] NS – non-significant; Model 1 adjusted for age and male gender; Model 2 additionally adjusted for smoking status, body mass index, hypertension duration, diabetes mellitus, GFR at baseline, ischemic stroke and coronary artery disease; Model 3 additionally adjusted for blood pressure at follow-up, anti-platelets, statins, anti-hypertensive drugs.
Discussion
Hypertension is an important public health problem to China due to the high prevalence and incidence [20, 21]. In addition, hypertension causes millions of strokes and heart attack in China annually [22, 23]. However, the optimal therapeutic BP goal for Chinese hypertensive patients is unclear and without solid clinical evidence. After the new ACC/AHA Hypertension Guideline was released, many researchers around the world were eager to conduct studies to evaluate how the new hypertension guideline would influence hypertensive patients in their own countries.
Using a retrospective design, we compared the differences of cardiovascular outcomes and adverse events in the Chinese hypertensive patients. Our current study for the first time showed that: (1) although some differences in study endpoints were observed between the low (SBP/DBP < 130/80 mm Hg) and high (SBP/DBP < 140/90 mm Hg) therapeutic BP goal groups, the differences did not achieve statistical significance; (2) compared to the uncontrolled hypertension group, patients in the low and high therapeutic BP goal groups had lower unadjusted and adjusted cardiovascular risk without increased risk of adverse events; and these benefits were more prominent in the low versus high therapeutic BP goal group.
Hypertension is a well-known risk factor for a variety of cardiovascular and renal diseases. Post-hoc analysis and meta-analysis have shown that therapeutic BP level was linearly correlated with cardiovascular events [3, 24, 25], suggesting that achieving a lower therapeutic BP goal might be beneficial for some hypertensive patients. However, due to the design-related limitations of prior studies, the therapeutic BP goal remained as SBP/DBP of 140/90 mm Hg for general hypertensive populations. However, after publication of the SPRINT clinical trial which demonstrated that a lower therapeutic BP goal was better than the traditional therapeutic BP goal in reducing cardiovascular events, aggregated data from prior published clinical trials and meta-analyses also showed that a lower BP therapeutic goal would be better to prevent cardiovascular and renal diseases [5, 26–28]. However, most of these data were derived from Caucasian populations, and whether the recommendation could be extrapolated to Chinese hypertensive patients is unknown.
Our current study showed that after 1 year’s follow-up, patients with a low therapeutic BP goal had significantly fewer cardiovascular events compared to the uncontrolled hypertension group even after adjusting for demographics and comorbidities, demonstrating that BP per se was an independent risk factor for cardiovascular events, which was consistent with prior reports [29–32]. Furthermore, it was found that patients in the low therapeutic BP goal group also had lower risk of cardiovascular events than patients in the high therapeutic BP goal group, although without statistical significance, which might be due to the relatively small sample size or short-term follow-up. However, from a clinical perspective, these findings still supported the notion that a lower therapeutic BP goal might be better for Chinese hypertensive patients. Notably, as shown in Table III, the significant differences in composite endpoints were driven by the difference in ischemic stroke/TIA, once again indicating that hypertension has a disproportional burden on the cerebrovascular system in Chinese hypertensive patients. Furthermore, in our current study, we did not observe any significantly increased risk of adverse events including falling down or a significant change of renal function as reflected by GFR.
Importantly, patients in the high therapeutic BP goal group also had fewer cardiovascular events than the uncontrolled hypertension group even after adjusting for demographics and comorbid conditions. Of note, as presented in Table IV, these benefits were found to be smaller than those in the low therapeutic BP goal group. From a clinical perspective, it was clinically relevant because lowering BP can absolutely reduce the risk of cardiovascular events.
The clinical implications of our current study included the following: 1) it seems that the lower therapeutic BP goal was also reasonable for the Chinese hypertensive patients and clinicians may try to lower the BP level for their patients while closely monitoring potential side effects; 2) future studies of Chinese hypertensive patients should be conducted to corroborate our current findings; 3) since the current study was conducted on Chinese hypertensive patients, we were uncertain whether our findings could be extrapolated to other population groups. However, findings from our current study provide clues for future studies.
There were some limitations of the study that need to be addressed. First, due to the observational design, no causal relationship could be drawn from our study. Unmeasured and undetected covariates might exist. The study was conducted in Chinese hypertensive patients and therefore our findings could not be extrapolated to other ethnic groups. However, data from this study should provide evidence for a future randomized controlled trial aiming to evaluate the optimal therapeutic BP goal for Chinese hypertensive patients. Last but not least, due to the relatively small sample size and short-term follow-up, we did not observe statistically significant differences in composite endpoints between low and high therapeutic BP goal groups, which deserve further investigation.
In conclusion, this study shows that in Chinese hypertensive patients, compared to uncontrolled hypertension patients, a low therapeutic BP goal is better for reducing cardiovascular events than a high BP therapeutic goal, without any significantly increased risk of adverse events.