Introduction
Stroke is the second cause of disability worldwide [1], which usually refers to the clinical syndrome of cerebral infarction, cerebral hemorrhage, and subarachnoid hemorrhage. Stroke damages the central nervous system, resulting in sensory, cognitive and motor deficits, poor physical coordination, and difficulty in maintaining balance [2]. The prevalence rate of balance dysfunction after stroke is as high as 83% [3, 4], which makes patients unable to sit, walk, or stand up normally, and leads to slower walking speed, shorter support time, inability to keep synchronized movements on both sides of the body, and proneness to falls [5]. The fear of falling leads to a sedentary lifestyle, which puts enormous psychological pressure on patients and their families [6], while greatly increasing the risk of disability and recurrence after stroke and placing a huge economic burden on families and society [7]. Therefore, it is important to seek effective ways to improve the balance function of patients. Pharmacological treatment is usually used to improve the patient’s overall function, with little mention of single symptom improvement [8], while surgical treatment requires strict surgical indications [9] and is not the preferred option in the non-acute phase.
Rehabilitation training is effective to restore balance function in stroke patients. The human brain is plastic, because it has the ability to adapt to environmental changes in structure and function [10], which provides a physiological preparation for the feasibility of rehabilitation training. Some studies have shown that the degree of brain plasticity of patients is closely related to early rehabilitation training [11, 12]. The 2018 US guidelines [13] and the 2011 Chinese guidelines [14] recommend that stroke patients begin rehabilitation as soon as they are stable.
There are many rehabilitation methods to improve the balance of stroke patients, such as balance training, smart equipment combined training, traditional Chinese medicine exercise, dual task training, core stability training [15], and whole-body vibration training. A meta-analysis showed that 1 h of balance training at least 3–5 times per week, or 30 min of gait-oriented exercises 3–5 times a week, was effective in improving balance and walking [16]. Rehabilitation requires long term perseverance, but the positive aspect is that it is flexible and in many cases, e.g. the COVID-19 epidemic where everyone cannot go out [17], and in the final phase of rehabilitation, etc., remotely supervised online exercise rehabilitation by a physiotherapist is one of the available and recommended home options to continue with the required exercise rehabilitation [18, 19]. Balance training is a relatively mature form of rehabilitation training. With the development of technology, rehabilitation combined with smart technologies has become a relatively emerging therapy, including virtual reality technology [20, 21] brain-computer interface technology [22–24] and rehabilitation robots [25–27], etc. They are mostly used for the rehabilitation of hospitalized elderly patients to improve their physical condition while increasing their self-confidence in recovery [28–30]. Although smart technology is more efficient, convenient, individualized, and interesting, it cannot be used on a large scale due to the lack of flexibility, high price of smart devices, and the application of smart technology treatment costs and other problems [31]. Traditional Chinese medicine exercises such as Baduanjin, Taichi and Yijinjing do not require external equipment, but regulate the “qi” in the meridians by completing a complete set of unique training postures, which strengthen the active participation of the brain in the process to increase the activity of the central nervous system. A meta-analysis showed that Taichi and Baduanjin were more effective in improving the balance ability of stroke patients [32]. Their limitation was that they cannot be applied to patients with severe balance loss, but they are more effective for patients with mild balance disorder.
The 2016 AHA/ASA (American Heart Association/American Stroke Association) guidelines [33] recommended rehabilitation through balance function training, treadmill, and mechanical assistance. The Chinese guidelines for Stroke Prevention and Treatment (2021 edition) [34] and the Dutch guidelines [35] recommend mirror therapy, sit-to-stand training, and training to improve respiratory muscles, and recommend that all stroke patients should receive rehabilitation of daily living activities that are suitable for them and eventually adapted to the discharge environment, and strengthen training through specific tasks. In 2019, the Department of Veterans Affairs and the U.S. Department of Defense released “The management of stroke rehabilitation: a synopsis of the 2019 U.S. Department of Veterans Affairs and U.S. Department of Defense Clinical Practice Guideline”, which recommended task-oriented training, motor imagery therapy, and so on.
This study found that different guidelines have given different advice. There was no conclusive evidence on which type of rehabilitation is more effective at restoring balance in stroke patients. In order to provide an effective reference for clinical practice, in this study a meta-analysis was conducted combining several rehabilitation training modes applied in clinical practice. The protocol for this network meta-analysis was registered with PROSPERO; the ID was CRD42022363795.
Material and methods
Information and methods
Inclusion criteria
Firstly, the included literature comprised randomized controlled trials. Secondly, the study included all patients who had a definite diagnosis of stroke. Thirdly, the control group used traditional rehabilitation training. The routine rehabilitation training was guided by three levels of rehabilitation training recommended by the “Chinese Stroke Rehabilitation Guidelines (2011 Complete Edition)”, including passive joint movement, good limb position placement, sitting and standing balance training, feeding and dressing and other life skills training, walking training, weight transfer training, and weight bearing training, etc. [14]. Also rehabilitation education was provided to the study subjects.
The intervention group used exercise therapy combined with traditional rehabilitation training, including core muscle group training, core stability training, suspension exercise, cordage therapy, sit-stand training, mirror therapy, whole-body vibration training, and respiratory muscle training;
Fourthly, the duration of intervention ranged from 4 weeks to 3 months. Fifthly, outcome indicators were as follows: Balance function is closely related to trunk control, walking ability, and life skills, and many studies have selectively examined the effects of rehabilitation training on these areas. In most of the included studies, balance function was measured using the BBS score (Berg Balance Scale), the Fugl-Meyer motor scale (balance component), and the TIS scale (Trunk Impairment Scale). In a few included studies the mini-balance evaluation systems test (mini-BES Test) and the Lindmark balance meter were used. The gross motor function measure (GMFM-66) and the Fugl-Meyer motor scale were mostly used to measure activity function. The trunk control test (TCT) was the method used in most studies to observe trunk control ability. The modified Barthel index (MBI) was used to assess self-care ability. Walking ability was evaluated using the functional ambulation category (FAC), the 6-minute walk test, and the 10-meter walk test (10-MWT). Since our study focused on observing balance ability, and there were many assessment methods for balance function, the outcome indicators of this meta-analysis were mainly compared in a uniform manner by the BBS scores used in all studies. The BBS score was the most commonly used tool to assess balance function of stroke survivors [36], with a total of 14 items, such as standing up, sitting down, and transferring. The maximum score was 6, and the minimum score was 0; the higher the score, the better the balance.
Exclusion criteria
Firstly, in the treatment group there was a combination of 8 types of rehabilitation training with other treatment methods. Secondly, the number of subjects in the control or intervention group was less than 30. Thirdly, duplicate published literature. Fourthly, literature from which one cannot extract data or with missing data, conference literature. Fifthly, non-RCT literature, such as network meta-analyses, meta-analyses, systematic reviews, reviews, theoretical literature, prominent medical practices, animal tudies, case-control literature, and cohort literature, etc. Sixthly, studies with most subjects dropping out.
Type of ending indicator
According to different versions of stroke clinical guidelines and expert consensus, in this study, combined with the frequency of outcome indicators, the BBS score values were determined as outcome indicators under the guidance of this strategy.
Literature screening and data extraction
The relevant literature screening was conducted, and a bibliography was derived based on the search strategy. Endnote X9 software was used to eliminate duplicate literature and literature that did not meet the inclusion criteria. The full text of the literature that potentially met the inclusion criteria was downloaded to determine whether it met the inclusion criteria. Two authors (Chengjiang Liu and Chunlin Li) independently screened, extracted, and cross-checked the literature based on inclusion and exclusion criteria, including first author, time of publication, sample size, sex ratio, mean age, mean duration of disease, number of cases, interventions in the trial group, interventions in the control group, treatment course, and outcome measures.
Information sources
The retrieval databases include CNKI, VIP Database, Wanfang Database, PubMed, Web of Science, Embase, Cochrane, Scopus. All searches were conducted from database creation to January 2023.
Search strategy
Taking PubMed as an example, PubMed Search Strategy:
#1 stroke [Mesh]
#2 apoplexy [Title/Abstract] OR cerebrovascular accident [Title/Abstract] OR cerebral infarction [Title/Abstract] OR cerebral hemorrhage [Title/Abstract] OR brain hemorrhage [Title/Abstract] OR intracerebral hemorrhage [Title/Abstract]
#3 #1 OR #2
#4 balance function [Title/Abstract]
#5 core muscle training [Title/Abstract]
#6 #3 AND #4 AND #5
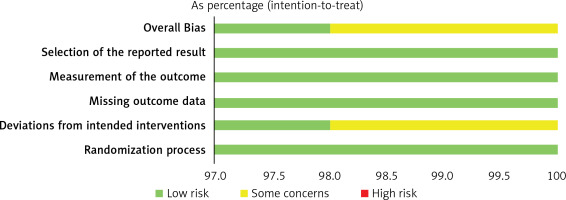
Risk of bias assessment
Two evaluators (Hui Liu and Hongbo Yin) independently used the new version of the Cochrane Collaboration Network’s RCT risk-of-bias assessment tool (Revised Cochrane risk-of-bias tool for randomized trials, RoB2) to assess the quality of each study in five areas: bias in randomization process, bias in deviation from established interventions, bias in missing outcome data, bias in outcome measures, bias in selective reporting of outcomes, and visualization of the bias risk assessment using macro-enabled Excel files. Literature quality was assessed at three levels: low risk of bias, some concerns, and high risk of bias. Disagreements were resolved through discussion with the third investigator (Yunhao Yi).
Statistical analysis
Meta-analysis was performed using STATA 17.0 software. Mean difference (MD) and 95% confidence interval (CI) were used to analyze whether there were significant differences between rehabilitation training interventions and traditional rehabilitation training. Statistical analysis was carried out using the NETWORK package to construct a network evidence map and to discuss the heterogeneity test and consistency analysis of the included data. If a closed loop was formed in the study, a consistency test was required and a p > 0.5 indicates good consistency between all studies. The likelihood ranking of each intervention was interpreted by the surface under the cumulative ranking probability curve (SUCRA) in the cumulative probability diagram to obtain the ranking among the rehabilitation training methods; the larger the value, the better the effect of intervention. The estimations of small sample effects and publication bias were evaluated using corrected comparative funnel plots.
Results
Literature search and screening
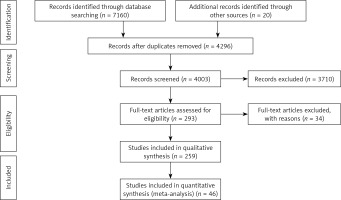
7160 related papers were obtained by initial retrieval, and 20 related papers were supplemented, among which 2884 duplicate papers were deleted by Endnote software. 4003 papers were screened manually. There were 293 papers that met the inclusion requirements, and then 34 papers for which the full text could not be found were deleted. There are 259 papers left. We rejected the literature with sample size less than 30, intervention time less than 4 weeks and an unclear grouping method, and included the literature with higher quality. Finally, 46 articles and 3741 patients were included. The process and results of literature screening are shown in Figure 1.
Figure 1
PRISMA 2009 Flow diagram. From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. PLoS Med 6(7): e1000097. doi:10.1371/joumal.pmed1000097. For more information, visit www.prisma-statement.org.
From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. PLoS Med 6(7): e1000097. doi:10.1371/joumal.pmed1000097. For more information, visit www.prisma-statement.org.
Basic characteristics of included studies
The 46 included publications [37–82] included 3731 patients with stroke. The basic information of the literature included is shown in Table I of the Materials.
Table I
Basic characteristics of included studies
| Author year [ref.] | Grouping method | Control group | Intervention group | Control group (n1) | Intervention group (n2) | Duration of inter-vention |
|---|---|---|---|---|---|---|
| Liang 2012 [37] | Random number table method | Traditional rehabilitation training | Core stability training | 34 | 34 | 6W |
| He 2012 [38] | Random lottery method | Traditional rehabilitation training | Sit-stand training | 30 | 30 | 4W |
| Bai 2013 [39] | Random method | Traditional rehabilitation training | Core muscle training | 32 | 32 | 6W |
| Wang 2014 [40] | Random method | Traditional rehabilitation training | Core muscle training | 39 | 39 | 8W |
| Lin 2014 [41] | Random method | Traditional rehabilitation training | Core muscle training | 41 | 41 | 6W |
| Yang 2015 [42] | Random method | Traditional rehabilitation training | Whole-body vibration training | 30 | 30 | 8W |
| Huang 2016 [43] | Excel random software grouping method | Traditional rehabilitation training | Suspension exercise therapy | 39 | 40 | 4W, 8W |
| Zhang 2016 [44] | Random method | Traditional rehabilitation training | Core stability training | 30 | 30 | 6W |
| Zhang 2016 [45] | Random number table method | Traditional rehabilitation training | Cordage therapy | 57 | 59 | 1M |
| Nie 2016 [46] | Random method | Traditional rehabilitation training | Sit-stand training | 40 | 40 | 3W |
| Xiao 2017 [47] | Random method | Traditional rehabilitation training | Core stability training | 49 | 48 | 6W |
| Jiang 2017 [48] | Random method | Traditional rehabilitation training | Sit-stand training | 30 | 30 | 4W |
| Li 2018 [49] | Random method | Traditional rehabilitation training | Mirror image therapy | 30 | 30 | 8W |
| Fang 2018 [50] | Random method | Traditional rehabilitation training | Core muscle training | 30 | 30 | 8W |
| Chai 2018 [51] | Random method | Traditional rehabilitation training | Core muscle training | 34 | 34 | 10W |
| Zha 2018 [52] | Random method | Traditional rehabilitation training | Suspension exercise therapy | 62 | 62 | 4W |
| Li 2018 [53] | Random method | Traditional balance training | Suspension exercise therapy | 50 | 50 | 6W |
| Liu 2018 [54] | Random number table method | Traditional rehabilitation training | Cordage therapy | 41 | 41 | 8W |
| Cao 2019 [55] | Random method | Traditional rehabilitation training | Sit-stand training | 59 | 59 | 4W |
| Wang 2019 [56] | Random method | Traditional rehabilitation training | Cordage therapy | 30 | 30 | 6W |
| Wang 2019 [57] | Random number table method | Traditional rehabilitation training | Cordage therapy | 52 | 53 | 8W |
| Jiang 2019 [58] | Random method | Traditional rehabilitation training | Core muscle training | 40 | 40 | 8W |
| Dang 2019 [59] | Random parallel grouping method | Traditional rehabilitation training | Core muscle training | 52 | 52 | 12W |
| Zhao 2019 [60] | Random number table method | Traditional rehabilitation training | Core stability training | 88 | 88 | 12W |
| Cen 2019 [61] | Random number table method | Traditional rehabilitation training | Suspension exercise therapy | 30 | 30 | 8W |
| Yuan 2019 [62] | Random number table method | Traditional rehabilitation training | Sit-stand training | 42 | 42 | 4W |
| Huang 2019 [63] | Random number table method | Traditional rehabilitation training | Mirror image therapy | 30 | 30 | 6W |
| Chen 2019 [64] | Stratified random grouping method | Traditional rehabilitation training | Mirror image therapy | 31 | 31 | 4W |
| Jin 2019 [65] | Random method | Traditional rehabilitation training | Whole-body vibration training | 35 | 35 | 6W |
| Han 2019 [66] | Random method | Traditional rehabilitation training | Respiratory muscle training | 30 | 30 | 4W |
| Jia 2020 [67] | Random method | Traditional rehabilitation training | Core stability training | 30 | 30 | 8W |
| Huang 2020 [68] | Random method | Traditional rehabilitation training | Core stability training | 36 | 36 | 12W |
| Tang 2020 [69] | Random number table method | Traditional rehabilitation training | Core stability training | 40 | 40 | 12W |
| Gao 2020 [70] | Random method | Traditional rehabilitation training | Suspension exercise therapy | 80 | 80 | 1M, 3M |
| Wang 2020 [71] | Random number table method | Traditional rehabilitation training | Whole-body vibration training | 43 | 43 | 12W |
| Wei 2021 [72] | Random method | Traditional rehabilitation training | Core muscle training | 30 | 38 | 12W |
| Luo 2021 [73] | Random method | Traditional rehabilitation training | Core stability training | 40 | 40 | 12W |
| Jia 2021 [74] | Random method | Traditional rehabilitation training | Suspension exercise therapy | 37 | 37 | 2M |
| Di 2021 [75] | Random number table method | Traditional rehabilitation training | Suspension exercise therapy | 34 | 34 | 3M |
| Ye 2021 [76] | Random method | Traditional rehabilitation training | Sit-stand training | 53 | 53 | 3M |
| Wang 2021 [77] | Random method | Traditional rehabilitation training | Mirror image therapy | 50 | 50 | 4W |
| Chi 2021 [78] | Random number table method | Traditional rehabilitation training | Mirror image therapy | 35 | 35 | 1M |
| Wei 2021 [79] | Random number table method | Traditional rehabilitation training | Whole-body vibration training | 30 | 30 | 4W |
| Lin 2022 [80] | Random number table method | Traditional rehabilitation training | Respiratory muscle training | 42 | 42 | 6W |
| Liu 2022 [81] | Random paper method | Traditional rehabilitation training | Respiratory muscle training | 40 | 46 | 8W |
| Xin 2022 [82] | Random method | Suspension exercise therapy | Respiratory muscle training | 20 | 20 | 4W |
Risk of bias assessment for inclusion in the study
The principle of randomization of allocation was used in the included literature. The main bias was due to deviations from intended interventions. 61 cases in each of the control and observation groups were initially included in one study. 2 patients in the control group failed to complete follow-up during the study due to incomplete information, 3 patients in the observation group stopped follow-up for financial reasons and 1 patient failed to complete follow-up and dropped out. The final outcome evaluation was based on 59 cases in the control group and 57 cases in the observation group. Ending data were complete. There were no cases of selective reporting bias. Overall, the majority of the literature included in this study was of medium to high quality level. Figure 2 shows the risk of bias assessment for the relevant literature.
Closing indicators
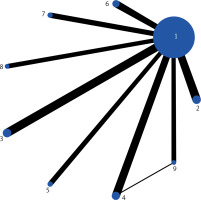
Web evidence map: Figure 3 shows the network evidence map. Numbers 1-9 are traditional rehabilitation training, core muscle training, core stability training, suspension therapy, cordage therapy, sit-stand training, mirror therapy, whole-body vibration training and respiratory muscle training. In the reticulated evidence map, dots represented the rehabilitation training modality, the size of dots represented the size of the intervention, and the lines connecting dots indicated the number of direct comparison studies between the two rehabilitation training modalities. The thicker the lines are, the larger number is. The traditional rehabilitation training was directly compared with the other 8 types of rehabilitation training, and the sample sizes of core muscle training, core stability training, and suspension therapy were all larger than other rehabilitation training methods.
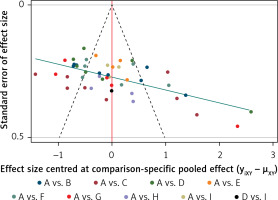
Publication bias risk: Corrected funnel plot were used to detect risk of bias for inclusion and publication of small sample effects. As shown in Figure 4, the funnel plot is largely symmetrical, with the outcome points lying roughly on either side of the zero line. This indicates that the possibility of publication bias and small sample effects in this study is minimal.
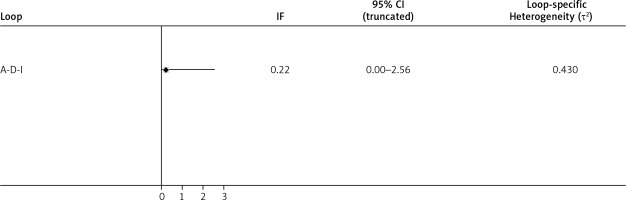
Heterogeneity test and consistency analysis: The included studies formed a closed loop and the test for heterogeneity showed IF > 0 and no heterogeneity between all studies, p > 0.5 in the consistency analysis, with good agreement between all studies, as shown in Figure 5.
SUCRA probability ranking: According to the results of the SUCRA curve area (Figure 6) and the two-by-two comparison matrix (Table II), all eight types of rehabilitative exercise training were more effective than traditional rehabilitation training. The area of the 8 rehabilitation training effects under the SUCRA curve was ranked from largest to smallest as follows: core stability training (C: 96.7%) > whole-body vibration training (H: 87.4%) > mirror therapy (G: 63.5%) > sit-stand training (F: 56.1%) > suspension training (D: 48.0%) > core muscle training (B: 39.8%) > cordage therapy (E: 31.1%) > respiratory muscle training (I: 26.9%) > traditional rehabilitation training (A: 0.4%).
Table II
Two-by-two comparison matrix of different rehabilitation training measures (shown as odds ratio and 95% confidence intervals)
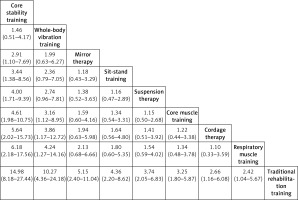
Reticulated meta-analysis: In terms of improving balance, core stability training (odds ratio (OR) = 14.98, 95% confidence interval (CI): 8.18–27.44) was more effective than traditional rehabilitation training, followed by whole-body vibration training (OR = 10.27, 95% CI: 4.36–24.18), mirror therapy (OR = 5.15, 95% CI: 2.40–11.04), sit-stand training (OR = 4.36, 95% CI: 2.20–8.62), suspension therapy (OR = 3.74, 95% CI: 2.05–6.83), core muscle training (OR = 3.25, 95% CI: 1.80–5.87), cordage therapy (OR = 2.66, 95% CI: 1.16–6.08), and respiratory muscle training (OR = 2.42, 95% CI: 1.04–5.67).
Discussion
To our knowledge, this is the first study to include eight rehabilitation training modalities for comparison of rehabilitation efficacy. In the present study, 46 studies with a total of 3741 participants were finally included. The most important result of this meta-analysis is the demonstration that core stability training is more effective in promoting the recovery of balance function in stroke patients compared to the other 7 types of rehabilitation training such as mirror therapy. It is worth noting that included studies were homogeneous, and there was no substantial publication bias. All these characteristics suggest that meta-analysis results are reliable.
Balance dysfunction after a stroke can have a significant impact on a patient’s life. Choosing more effective rehabilitation exercises can enhance the speed of recovery of balance function and reduce the patient’s burden. The ranked results showed that core stability training was most likely to be the best choice for rehabilitation, followed by whole-body vibration training. Previous meta-analyses showed that core stability training was superior to conventional rehabilitation [83], which could significantly improve patients’ static and dynamic balance. Core stability training emphasizes core stability, which was the foundation of body weight stability and movement. This type of rehabilitation involved the training of the complete dynamic chain of spinal, pelvic, deep thoracic, and abdominal muscles [84], as well as involving the muscle groups that are essential for the static and dynamic balance stability of the spine, such as synergistic contraction of the transversus abdominis and multifidus [85]. Core stability training was performed mainly to improve the stability of trunk movement by enhancing the muscle strength and power transmission of the core muscles of the limbs, and improve the balance ability of the patients by enhancing the muscle strength of the muscle groups, so as to improve the coordination of the patient’s body. In addition, effective core stability training can further strengthen the body’s sensory perception, and accelerate the rehabilitation process [86].
Whole-body vibration training was similar to core stability training, which can improve both the dynamic balance and static balance of patients [87]. Multiple randomized controlled studies have demonstrated the benefits of whole-body vibration training for balance restoration in stroke patients [88–91]. However, Alashram et al. found insufficient evidence that short-term whole-body vibration training has a positive effect on lower limb balance [92]. The reason for the different results may be related to the duration of treatment. Whole-body vibration training was a passive-induced active movement training, through the shaking table to produce repeated vertical up-down vibration and impact vibration to stimulate muscle groups to increase the degree of active muscle activation, as well as improving the excitability of the neuromuscular system to achieve the training effect [93]. The most common whole-body vibration training was whole-body vertical vibration training. One study conducted horizontal whole-body vibration training and found that it was not beneficial to improve balance function [94], and the current whole-body vibration training currently applied was based on vertical vibration.
Through network meta-analysis, this study compared 8 rehabilitation training exercises effective for balance recovery after stroke, including core muscle group training, core stability training and sit-stand training, so as to provide some reference for clinical application. However, there were still some limitations of this study. Firstly, the included studies had some geographical characteristics, and most of them were focused on China, which may lead to certain geographical deviations. Secondly, this study seldom considered the influence of rehabilitation training intensity. For example, the different frequencies of whole-body vibration training have an effect on the rehabilitation effect. Wei [95] found that there was no significant difference between 13 Hz and 26 Hz vibration frequency on the rehabilitation effect. Xiao-feng [87] found that 45 Hz whole-body vibration training was more effective after a 12-week training period. Thirdly, the study did not include long-term follow-up results and did not consider the effect of medication on the recovery of balance function. Fourthly, there is a lack of control over the timing of the start of the rehabilitation program. Fifthly, it is unclear whether special populations such as children or the elderly are included in RCTs. In the meantime, it was recommended that more standardized randomized controlled double-blind trials with good quality, large samples and multi-center participation be conducted to provide stronger evidence of effectiveness in the future.
The results of the network meta-analysis suggested that core stability training may be a more effective form of rehabilitation training in the covered literature. Nevertheless, more high-quality, large-sample, multicenter randomized controlled double-blind trials are needed for study confirmation.