Introduction
Stroke, an acute focal neurologic deficit syndrome caused by vascular injury in the central nervous system, is a leading cause of mortality and disability worldwide. Accounting for approximately 6 million deaths annually, stroke ranks as the 2nd leading cause of deaths globally [1, 2]. The burden of stroke in terms of patients, survivors, related deaths, and global disability-adjusted life years is increasing, especially in Europe [3, 4]. Specifically, the European population of 509 million had 120,000 new strokes and 530,000 stroke-related deaths in 2017, with projections indicating a substantial increase by 2047 [5].
Body mass index (BMI) is a well-established independent predictor of stroke risk, even after accounting for age, cardiovascular comorbidities (e.g., hypertension, diabetes), and lifestyle factors (e.g., smoking, physical activity) [6]. A pooled analysis of 97 prospective cohorts found that each 5 kg/m2 increase in BMI raised stroke hazard ratios (HR) to 1.18 (95%CI: 1.14–1.22) after adjusting for various confounders [7]. Elevated BMI is likely to contribute to stroke risk through mechanisms such as chronic inflammatory responses and metabolic dysregulation, which may promote the onset of stroke [8].
Interestingly, some studies report an ‘obesity paradox’, suggesting that individuals with higher BMI may exhibit lower mortality in certain conditions, including stroke. This paradox adds complexity to the relationship between BMI and stroke, indicating that BMI’s role in stroke outcomes may be more nuanced than traditionally understood and warrants further investigation. Nonetheless, large-scale studies consistently show a strong association between elevated BMI and increased stroke risk. For example, a meta-analysis of 5,798,826 participants reported that higher BMI (overweight or obese) significantly increases stroke risk, with pooled relative risk (RR) values of 1.25 (95%CI: 1.16–1.34) and 1.47 (95% CI: 1.02–2.11) [9].
Age-period-cohort effects have become an essential framework for understanding the complex relationship between BMI, stroke, and temporal trends. While the effects of age on stroke mortality are well documented, the impact of period (time) and cohort (birth group) effects remains less understood. Recent research suggests that period effects – such as shifts in public health strategies, medical interventions, and lifestyle changes – may explain some of the temporal variations in stroke rates. In addition, cohort effects may help to understand how generational differences in environmental exposures, lifestyle factors, and medical advancements influence stroke risk over time.
As elevated BMI rates rise across Europe, understanding the full scope of its role in stroke risk becomes increasingly critical [10]. Therefore, this study utilized Europe-wide stroke and BMI data from the Global Burden of Disease (GBD) database (1990–2019) to examine this association comprehensively [11, 12]. At present, relatively few studies have examined trends in stroke prevalence due to increased BMI in Europe, and traditional descriptive analyses of age-specific morbidity or mortality data at different time periods have not been able to eliminate or control for interactions between age, period, and cohort factors. The joinpoint regression (JPR) model is widely used to analyze the time trend of morbidity and mortality and the burden of disease, which can better reflect the change of epidemic trend and its impact. The age-period-cohort model improves the traditional descriptive analysis method to estimate the risk and trend of disease morbidity or mortality while adjusting for age, period, and cohort [13].
This study aimed to provide a comprehensive analysis of the relationship between elevated BMI and stroke within the European context. By examining trends in stroke incidence and disability-adjusted life years (DALYs) associated with high BMI, the JPR model and age-period-cohort analysis were employed to assess the impact of obesity on stroke prevalence. Our findings are intended to inform public health policies and clinical practices, supporting the development of targeted preventive measures and interventions. Such strategies have the potential to reduce the burden of stroke and obesity-related health issues, ultimately improving health outcomes at the population level.
Material and methods
Study design
This population-based observational study was designed to determine the relationship between an elevated BMI and stroke incidence within the European population. Subsequently, data on stroke mortality rates attributed to elevated BMI in the European population aged 20–94 years were collected from the GBD 2019 study. The selection of this age group is based on the relatively low stroke mortality rates in populations under 20 years of age, as well as the limited data reliability for those over 94 years old. Therefore, the age group 20–94 years was chosen to ensure more accurate representation and consistency in the analysis. The age-period-cohort model was then applied to analyze the risk of stroke mortality caused by an elevated BMI.
Global Burden of Disease
The data for this study were obtained from the GBD 2019 study [14], which provides comprehensive estimates of stroke mortality attributed to an elevated BMI across different regions, including Europe. Specifically, we extracted data on stroke deaths related to high BMI (defined as BMI ≥ 25 kg/m2) for the European population aged 20–94 years.
The GBD 2019 study reports age-standardized stroke mortality rates, as well as estimates of DALYs for different age groups and sex. The stroke mortality data were standardized based on the GBD 2019 world standard population, ensuring consistency in comparison across different populations and time periods.
Joinpoint regression model (JRM)
The JRM was selected to identify significant trend shifts over time, making it particularly suitable for analyzing temporal changes in stroke mortality. Unlike traditional models, which may not capture precise points of trend changes, the JRM can detect and quantify specific inflection points in mortality rates attributed to elevated BMI. The JRM was used to fit the data on stroke mortality rates, with statistical significance determined through the Monte Carlo permutation test. This approach allows for the calculation of annual percentage change (APC) and average annual percentage change (AAPC), along with 95% confidence intervals (CIs). Positive APC or AAPC values indicate an increasing mortality trend, while negative values suggest a decline.
Age-period-cohort model
To address potential collinearity between period and cohort effects in the age-period-cohort model, we used the intrinsic estimator method, which is designed to manage collinearity among these variables. This method allows for the independent estimation of age, period, and cohort effects, ensuring more accurate and transparent analysis of stroke trends over time. Compared to traditional models, the APC model provides several advantages. It allows for the separation of age, period, and cohort effects, offering a more nuanced understanding of each factor’s influence on stroke mortality.
The age-period-cohort model is based on the Poisson distribution and analyzes the risk of stroke mortality attributed to an elevated BMI in the European population based on the following: age; period; and cohort. With every 5-year increment grouped as 1 age group, individuals aged 20–94 years were assigned to 15 groups. To meet the structural requirement of the model that the age group interval equals the period group interval, the years 1990–2019 were divided into 6 groups, with each interval 5 years long. The birth cohort was calculated as the period minus age, resulting in 20 cohorts. This model helps us to understand how the effects of BMI on stroke mortality vary not only by age but also by temporal factors such as public health changes and cohort-specific risk factors. To understand the linear relationship between age, period, and cohort in the model, the intrinsic estimator method was used to estimate the effect coefficients.
Statistical analysis
The APC and AAPC were calculated using Joinpoint Regression Software (version 4.9.0.0), which provides advanced methodologies for detecting trend shifts in stroke mortality over time. Age, period, and birth cohorts were each segmented into 5-year intervals to ensure consistency in the age-period-cohort analysis. Effect coefficients and relative risks were calculated with the intrinsic estimator package in Stata 17.0, chosen for its robust capabilities in handling complex regression analyses. Relative risk (RR) was determined as [RR = exp(effect coefficient)], with a higher RR indicating a greater risk of stroke incidence. Additionally, R software (version 4.2.1) was used to project stroke mortality rates in Europe from 2020 to 2049. Statistical significance was set at p < 0.05.
Results
Trends in stroke mortality attributed to an elevated BMI in the European population
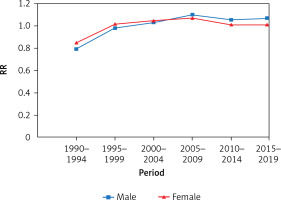
The standardized mortality rate of stroke attributed to an elevated BMI in the overall European population showed a wave-like declining trend (AAPC = –1.47%, 95% CI: –1.86 to –1.08, p < 0.001), decreasing from 21.73/100,000 in 1990 to 14.01/100,000 in 2019 (Figure 1). The most significant decline was observed between 2003 and 2013 (APC = –4.10%, 95% CI: –4.44 to –3.75, p < 0.001). The standardized mortality rate in males was generally higher than females. The male standardized mortality rate decreased from 21.48/100,000 in 1990 to 15.45/100,000 in 2019 (AAPC = –1.07%, 95% CI: –1.67 to –0.66, p < 0.001). The decline in the female standardized mortality rate was more substantial (AAPC = –1.84%, 95% CI: –2.23 to –1.44, p < 0.001), dropping from 21.40/100,000 in 1990 to 12.48/100,000 in 2019 (Table I).
Figure 1
Age-standardized mortality rate (ASMR) trends by gender from 1990 to 2019 using joinpoint regression models
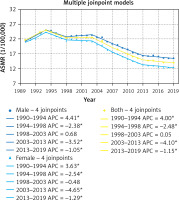
Table I
Changing trends in standardized stroke mortality rates attributed to an elevated BMI in Europe from 1990 to 2019
Trends in stroke mortality attributed to an elevated BMI by age, period, and cohort
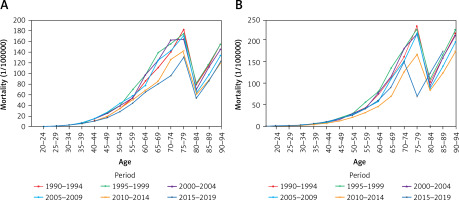
Age period mortality rate
The stroke mortality in the European population 20–94 years of age showed a similar trend in all age groups. In the 20–54-year-old age group, the stroke mortality rate gradually increased for males and females, and after 55–79 years of age, the mortality rate tended to increase. For males and females, the mortality rate was highest in the 75–79 age group, decreasing in the 80–84 age group, and continuing to increase in the 85–94-year-old age group. The RR for stroke mortality in the 75–79 age group was 2.8-fold higher compared to the 20–54 age group (95% CI: 2.5 to 3.2, p < 0.001), highlighting the significant increase in stroke risk with age (Figure 2). Compared to other periods, the mortality was higher for males and females in the period 1990–1994 (Figure 2).
Age-cohort mortality rate
Age-specific stroke mortality in the European population tended to decrease as the birth cohort increased. Males and females in the elevated BMI cohort had an increasing, then decreasing trend in stroke mortality after the 55–59-year-old age group. Mortality varied by birth cohort at the same age, and this difference was more pronounced in the earlier birth cohorts. In the 90–94-year-old age group, stroke mortality due to an elevated BMI was 1.26-fold higher in males and 1.24-fold higher in females born in 1900–1904 compared to those born in 1925–1929 (95% CI for males: 1.18 to 1.34, p < 0.001; 95% CI for females: 1.15 to 1.33, p < 0.001) (Figure 3).
Age-period-cohort analysis of stroke mortality attributed to an elevated BMI in the European population
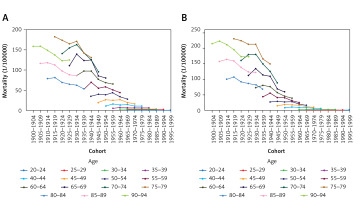
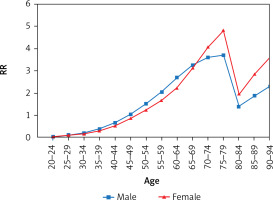
Age effect
The age effect showed that stroke mortality due to an elevated BMI generally increased with age in European males and females aged 20–79 years, with a decreasing then increasing trend after 80–94 years of age. For example, the RR of stroke death in the 75–79-year-old age group was 63.04-fold higher compared to the 20–24-year-old age group (95% CI: 60.22 to 66.30, p < 0.001). This high RR reflects the strong age-related effect of BMI on stroke mortality. The RR for females in the 75–79 age group was even higher at 87.38-fold compared to the 20–24 age group (95% CI: 83.29 to 91.56, p < 0.001) (Table II, Figure 4).
Table II
Age-period-cohort model analysis of stroke mortality rate attributed to an elevated BMI in Europe
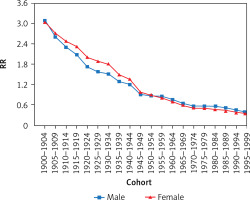
Period effect
The stroke mortality risk attributed to an elevated BMI for males and females exhibited consistent changes over the years. Except for a decline in the risk between 2010 and 2014, the mortality risk for other periods increased progressively over time. Between 2005 and 2009, the relative risk for stroke mortality was 1.38-fold higher for males and 1.26-fold higher for females compared to the 1990–1994 period (95% CI for males: 1.32 to 1.45, p < 0.001; 95%CI for females: 1.18 to 1.34, p < 0.001) (Figure 5, Table II).
Cohort effect
The cohort effect of an elevated BMI on stroke mortality risk varied significantly across different birth cohorts. Specifically, the RR for stroke death in males born between 1910 and 1914 was 8.29-fold higher than in males born between 1995 and 1999. Similarly, the RR for stroke death in females born between 1910 and 1914 was 9.10-fold higher than in those born between 1995 and 1999 (Figure 6, Table II). These differences were statistically significant, with 95% confidence intervals for males (95% CI: 8.01 to 8.57) and females (95% CI: 8.72 to 9.49), confirming the large disparities in stroke mortality across cohorts.
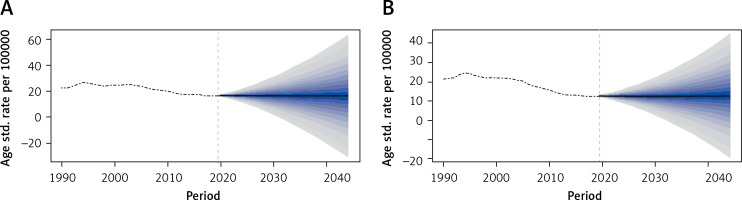
Prediction
According to the Bayesian age-period-cohort model, the age-standardized stroke mortality due to an elevated BMI is expected to gradually decline in Europe from 2020 to 2044. By 2044, the mortality rate for males in Europe is expected to continue to decline, decreasing by 12.99% compared to 2019. Similarly, stroke mortality in females is expected to continue a downward trend over the next 20 years, decreasing by 13.01% compared to 2019 (Figure 7).
Discussion
From 1990 to 2019, the stroke mortality rate attributed to BMI in the European population showed a declining trend. The age-period-cohort model revealed that the mortality rate trends in stroke caused by BMI in European males and females are influenced by age, period, and cohort effects. The joinpoint regression results showed that the stroke mortality rate attributed to an elevated BMI in Europe is generally declining, which was consistent with the overall mortality results in Europe [15]. The most significant decline in stroke-related mortality occurred between 2003 and 2013. Some studies have suggested that widespread changes in healthy behaviors and treatments for these risk factors are the reasons for the sharp decline in vascular mortality rates in high-income countries [15]. The higher mortality rate in males compared to females may be attributed not only to differences in hormone levels but also to lifestyle factors and behavioral patterns. Males are more likely to engage in habits such as smoking and alcohol consumption, which can increase the risk of overweight and obesity, thereby contributing to higher stroke mortality.
The age effect showed that the standardized mortality risk for stroke caused by an elevated BMI in the European population 20–79 years of age generally increased with age. The peak mortality for males and females occurred in the 75–79-year-old age group, which is consistent with the global trend of population growth and aging. As the global population continues to grow and age, the absolute number of stroke deaths has been increasing. The risk of stroke increases with age, and in males and females, the risk of stroke doubles after 55 years of age [16]. Moreover, as age advances and aging accelerates, population immunity decreases and risk factors related to stroke accumulate in the body. Cellular and vascular aging with collagen deposition accelerate the formation of mature atherosclerotic plaques and interact with an elevated BMI, thereby increasing the risk of death [17].
Notably, the risk of stroke mortality caused by an elevated BMI in the 80–84-year-old age group gradually decreased with age, showing contradictory results compared to previous studies. The obesity paradox has received much attention in recent years.
Several studies have shown that an elevated BMI may have a protective effect on survival after a stroke, a concept known as the obesity paradox [18]. For example, Gu et al. [19] found that obese patients were less likely to experience fatigue during the acute phase of ischemic stroke, suggesting that elevated BMI may provide a protective energy reserve. Similarly, Chaudhary et al. [18] observed that overweight and obese ischemic stroke patients had a significantly lower risk of 1-year mortality compared to those with normal weight. A cross-sectional study in Korea also found that obesity was negatively correlated with adverse outcomes in all stroke patients, and the obesity paradox may vary by stroke subtype [20, 21]. In European populations, elevated BMI may offer protective benefits through greater nutritional reserves and increased energy stores during stroke recovery. Additionally, lifestyle factors such as higher physical activity levels could mitigate the negative effects of obesity on stroke outcomes. Exploring these biological and lifestyle mechanisms in European populations could provide deeper insights into the obesity paradox and its role in stroke survival and recovery.
The period effect showed that the risk of stroke mortality caused by an elevated BMI in Europe has shown a trend of first rising, then falling, then rising again over the years, but the overall trend was not significant. The cohort effect showed that the mortality risk for males and females declined with the progression of the birth cohort. The World Health Organization 2015 World Health Statistics report showed that the overall obesity rate for adults was 21.5% for males and 24.5% for females in Europe [22]. An abundance of clinical and epidemiologic evidence indicated that obesity is associated with a wide range of cardiovascular diseases (CVDs). Obesity can directly or indirectly increase the incidence and mortality of CVDs. The direct effects are through cardiovascular system structural and functional adaptations induced by obesity to accommodate the excess weight and the impact of adipose factors on inflammation and vascular homeostasis, leading to a pro-inflammatory and pro-thrombotic environment. Indirect effects are mediated by accompanying CVD risk factors, such as insulin resistance, type 2 diabetes mellitus, visceral fat, hypertension, and dyslipidemia. Therefore, there should be an emphasis on controlling the overweight and obesity rates, advocating for a healthy weight [22]. People from later birth cohorts, with the advancement of economy and technology, pay more attention to pursuing a healthy lifestyle, enhancing health literacy, and maintaining a healthy BMI. Socioeconomic and biological factors can have a significant impact on stroke risk, severity, and outcomes. For example, approximately 68% of the variability in stroke incidence rates in different European countries can be explained by differences in the gross domestic product, reflecting the living standards and well-being of the population [23].
These findings have important public health implications. The observed decline in stroke mortality linked to BMI, together with the obesity paradox, suggests the need for a nuanced approach to stroke prevention. Policymakers should promote healthy lifestyle modifications for individuals with elevated BMI, while acknowledging that BMI alone may not fully predict stroke outcomes. Integrating these insights into preventive strategies could inform more effective health policies, especially for high-risk populations.
Although this study primarily examines the relationship between BMI and stroke mortality, it is essential to consider the role of socioeconomic factors. Income level, education, and healthcare access likely influence obesity and stroke outcomes across European regions. Individuals with fewer resources may have limited access to preventive care and face barriers to adopting healthier lifestyles, which can impact both BMI and stroke risk. Additionally, other contributors to the decline in stroke mortality, such as advancements in stroke management (e.g., improved treatment protocols and rehabilitation strategies) and expanded healthcare access, likely interact with BMI-related trends, collectively shaping stroke outcomes. Future research incorporating socioeconomic dimensions and other health determinants would deepen our understanding of these complex interactions, providing valuable insights for targeted public health interventions.
In conclusion, from 1990 to 2019, the stroke mortality rate caused by an elevated BMI in Europe has continuously increased. Stroke mortality was affected by age, period and cohort. Europe urgently needs to strengthen weight control for stroke patients and raise public health awareness through health education, with a particular focus on males and the elderly to reduce the death burden caused by stroke. There should be an emphasis on strengthening the three levels of stroke prevention and early screening to achieve early detection, control, and treatment to avoid unnecessary waste of public health resources and decreased public health.
This study’s findings, based on the GBD database, may be influenced by inherent biases and data accuracy limitations. We restricted the age range to 20–94 years due to low stroke incidence in those under 20 and limited data for those over 94, which affects the generalizability of our results, particularly to younger and older populations. Additionally, we did not analyze visceral vs. peripheral obesity, which may impact stroke risk differently. While we acknowledge the obesity paradox, its underlying mechanisms were not explored in this study, representing a gap in understanding.
Furthermore, our stroke mortality projections are based on pre-pandemic data, and the COVID-19 pandemic may have influenced stroke risk through changes in healthcare access and lifestyle behaviors. Post-pandemic data would be valuable for refining these projections. Lastly, the GBD database lacks detailed subgroup data, limiting our ability to conduct more granular analyses of specific populations, such as ethnic minorities or socioeconomically disadvantaged groups.