Balance impairments are a common concern in aging populations and among individuals with neurological and musculoskeletal disorders. They are one of the leading contributors to falls, which are associated with significant morbidity, mortality, and healthcare costs worldwide. Accurate assessment of balance function is thus crucial for the identification of fall risk, prevention planning, and rehabilitation. Among the many tools available for clinical balance assessment, the Berg Balance Scale (BBS) stands out as one of the most widely accepted and validated instruments [1].
The BBS, originally developed by Katherine Berg in the late 1980s, is a performance-based measure consisting of 14 tasks that assess balance during common functional activities, such as standing, turning, and reaching. Each task is scored on a 5-point scale, with a maximum score of 56 indicating good balance. The BBS has been extensively used across multiple populations, including older adults, individuals recovering from stroke, and people living with Parkinson’s disease, dementia, or other balance-compromising conditions [2].
Despite its widespread use, successful implementation of the BBS in diverse cultural and linguistic settings requires not only accurate linguistic translation but also cross-cultural adaptation, ensuring the tool remains conceptually equivalent and psychometrically valid in different populations. This process has been well documented in numerous studies across various languages and regions, each emphasizing the importance of tailoring clinical tools to the sociocultural context of their users.
Simon et al. conducted a cross-cultural validation of the BBS in Hungarian among institutionalized older adults [3]. The study demonstrated strong internal consistency (Cronbach’s α = 0.96), excellent inter-rater reliability (ICC = 0.99), and robust construct validity, highlighting the BBS’s utility in the Hungarian-speaking population. Similarly, Kashif et al. validated the Urdu translation of the BBS for individuals with Parkinson’s disease in Pakistan [4]. Their findings confirmed that the Urdu version retained the psychometric properties of the original, showing excellent test-retest and inter-rater reliability (ICC > 0.9) and high internal consistency (Cronbach’s α = 0.95).
In Brazil, the BBS has also been widely adapted. Scalzo et al. validated the Brazilian Portuguese version of the scale for use with patients with Parkinson’s disease. Their study confirmed good validity and sensitivity in detecting postural instability in this population [5]. More recently, Viveiro et al. examined the reliability and validity of the BBS alongside other balance tools (such as the BESTest and Mini-BESTest) in Brazilian older adults residing in nursing homes [6]. Their results again confirmed the BBS as a reliable and valid screening tool for identifying individuals at risk of falling.
Beyond translation and validation, broader reviews have emphasized the role of the BBS in clinical screening and fall risk prediction [7–10]. Lima et al. conducted a systematic review analyzing the BBS as a clinical tool to predict fall risk in older adults. The review concluded that the BBS has moderate-to-high predictive validity, making it an effective screening tool across various settings [11]. Complementing this, Beck Jepsen et al. performed an umbrella review of instruments for assessing gait, balance, and functional mobility in older adults. Their findings placed the BBS among the most frequently validated and cited tools, reinforcing its global clinical relevance [12].
Despite these global efforts, no validated Albanian version of the BBS currently exists, representing a significant gap in clinical and research capacities within Albanian-speaking populations. Albania, along with Kosovo and parts of North Macedonia and Montenegro, is home to a growing older adult population. Given the demographic trends and increasing prevalence of age-related conditions such as Parkinson’s disease and dementia, the absence of a validated BBS impedes efforts to systematically assess and address balance impairments and fall risks.
In line with best practices for instrument adaptation, the process of translating and validating the BBS into Albanian must follow internationally recognized guidelines [13]. These include forward and backward translation, expert committee review, pre-testing through cognitive interviews, and psychometric validation studies. As demonstrated in the translation of related tools such as the Fear of Falling Avoidance Behavior Questionnaire into Brazilian Portuguese from Nunes et al., each step is critical to ensuring semantic, idiomatic, experiential, and conceptual equivalence [14].
Moreover, the growing use of telehealth and digital platforms underscores the need for accessible and reliable balance assessment tools. Gillespie et al. compared in-person and telerehabilitation BBS scores among stroke survivors and found no significant differences, suggesting the BBS’s adaptability to remote assessment contexts. This further supports the necessity of having a localized version of the scale for Albanian clinicians working both in-person and remotely [15, 16].
In summary, the translation and cultural adaptation of the BBS into Albanian is both timely and essential. Given the tool’s global reputation, the demonstrated success of prior adaptations, and the pressing healthcare needs of the Albanian-speaking elderly population, this review seeks to emphasize the clinical importance of the BBS, summarize key findings from previous translation and validation efforts across various languages, and outline methodological considerations for adapting the tool into Albanian. Through this work, we aim to contribute to the growing literature on cross-cultural validation and support the development of equitable, evidence-based care practices across diverse linguistic and cultural contexts.
Methods
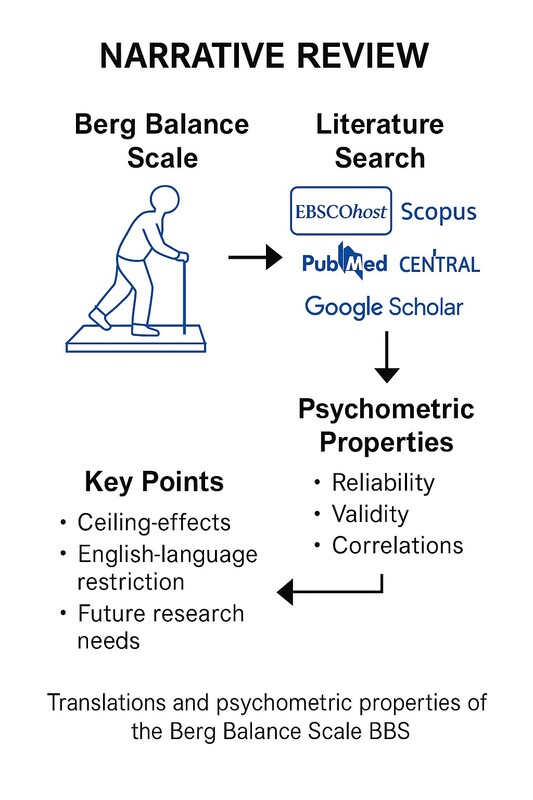
This narrative review aims to explore the importance of the BBS in the context of its translation and psychometric evaluation across various cultural and linguistic settings. The BBS, a widely used tool to assess balance and fall risk in older adults and other populations, has undergone several translations and cross-cultural adaptations. To understand the global applicability and reliability of the BBS, this review evaluates translations into languages such as Portuguese, Persian, Korean, Norwegian and others, as well as psychometric properties in diverse patient populations. The review synthesizes studies that address the translation process, cross-cultural validation, and psychometric testing of the BBS.
Search strategy
This study was designed as a narrative review aimed at synthesizing and critically discussing the literature on translations and psychometric evaluations of the BBS.
A broad literature search was undertaken across several academic databases, including EBSCOhost, Scopus, PubMed, Lilacs, IBECS, CENTRAL, Web of Science (WOS), SciELO, and Google Scholar, covering the period from 2000 to 30 March 2025. Search terms included “Berg Balance Scale”, “translation”, “cross-cultural adaptation”, “psychometric properties”, and “language versions”. Additional sources were identified by reviewing the reference lists of relevant publications and review articles concerning the BBS. For the purposes of this narrative review, emphasis was placed on studies that reported translation efforts, cross-cultural adaptations, or psychometric evaluations (e.g., reliability and validity) conducted with human participants, with priority given to works published in English.
Selection criteria
The selected studies for this review included those that focused on the translation and psychometric evaluation of the BBS in different populations, including older adults, patients with Parkinson’s disease, stroke survivors, and those with balance disorders. Studies were included if they presented data on the reliability (inter-rater reliability, test-retest reliability), validity (construct validity, criterion validity), and internal consistency of the translated BBS. Studies that evaluated the ability of the scale to predict fall risk, as well as its sensitivity and specificity in different clinical settings, were also considered relevant.
Study selection process
The initial screening of studies involved reviewing titles and abstracts. Duplicates were removed, and studies that did not meet the inclusion criteria were excluded. Full-text articles of the remaining studies were reviewed for relevance and quality. All studies that provided robust psychometric evaluation data and described the translation process in detail were retained. Studies were categorized based on their region of translation and the clinical population studied. The final sample of studies included publications from various countries.
Data extraction and analysis
Data from the included studies were collected using a standardized extraction form, covering the following categories: author(s) and year of publication; the language version of the BBS; the population studied (older adults, individuals with Parkinson’s disease, stroke survivors); psychometric properties assessed; and details regarding the translation and adaptation process. The analysis was focused on synthesizing the findings related to the reliability and validity of the translated versions of the BBS. Studies were reviewed for their methodology, sample sizes, statistical techniques, and outcome measures to provide a comprehensive summary of the psychometric evaluation of the BBS in different linguistic and cultural settings.
Psychometric evaluation
The validity of the scale was assessed through construct validity (the degree to which the scale measures the intended balance construct), criterion validity (the ability of the BBS to predict fall risk and other clinical outcomes), and content validity (the degree to which the items on the scale adequately represent the construct of balance).
Psychometric properties of the BBS were examined based on the studies’ evaluation of reliability and validity. Key measures of reliability include inter-rater reliability, test-retest reliability, and internal consistency. Inter-rater reliability refers to the agreement between different raters or clinicians using the BBS in a clinical setting. Test-retest reliability assesses the stability of the scale over time when used with the same individuals. Internal consistency evaluates the degree to which items on the BBS measure the same construct.
Statistical analysis
The statistical analysis of psychometric properties was conducted using various techniques, including correlation coefficients (for reliability measures), factor analysis (for construct validity), and regression analysis (to assess the scale’s predictive validity). Studies often report Cronbach’s α as a measure of internal consistency and use intraclass correlation coefficients (ICC) for test-retest and inter-rater reliability.
Quality assessment
To ensure the quality and methodological rigor of the included studies, each study was evaluated based on established criteria for psychometric research, such as sample size, statistical methods, and clarity of reporting. Studies that met the methodological standards for psychometric testing and translation procedures were included in the final review. Additionally, studies were assessed for potential biases, such as selection bias or language bias, based on the populations studied and the translation process used.
Results
From all the research databases such as EBSCOhost, Scopus, PubMed, Lilacs, IBECS, CENTRAL, Web of Science (WOS), SciELO and Google Scholar databases, a total of 17 articles were found with special interest in translation, cross-cultural adaptation, validity, and reliability.
The results summarized in Supplementary Table SI A highlight the global effort to validate and adapt the BBS across diverse populations, languages, and clinical conditions. Most studies adopted cross-sectional or validation designs, focusing on psychometric evaluation such as reliability, validity, and cultural adaptation of the BBS. The included countries ranging from Hungary, Pakistan, Brazil, and Iran to Japan, Norway, and Greece demonstrate widespread interest in ensuring the scale’s applicability beyond its original context [17–23]. Participants varied widely in number and characteristics, with most studies involving older adults or individuals with Parkinson’s disease, dementia, or stroke. Where reported, participant ages generally ranged from 60 to 70, reflecting the BBS’s relevance for aging populations. Gender was consistently mixed, although specific breakdowns were often omitted. Several studies, like those from Brazil and Italy, reported strong psychometric properties, supporting the BBS’s use for balance assessment across settings [5, 9]. Notably, studies emphasized inter-rater reliability and construct validity, critical components for clinical tools. The general consistency in findings supports the BBS as a robust instrument across cultures, though variability in reporting sample size, age, disease duration suggests a need for standardized methodologies in future validation efforts. Overall, the BBS proves adaptable and clinically useful across a spectrum of international contexts.
The findings in Supplementary Table SI B illustrate that most studies used a cross-sectional or validation design, focusing on the translation, cultural adaptation, and psychometric assessment of the BBS. The BBS was the primary tool used, with minimal implementation of additional assessments. Frequency of testing was generally a single administration, with few studies conducting test-retest evaluations. Only Jung et al. clearly reported a test-retest interval of 10 days [20]. Overall, the findings show that while BBS validation is widely conducted, standardized reporting of intervention frequency and test-retest intervals is limited, indicating a need for more consistent methodological transparency.
The extended Table I A presents a comprehensive synthesis of studies evaluating the validity and reliability of the BBS across different cultural contexts and populations. Most studies confirmed high inter- and intra-rater reliability, with ICCs ranging from 0.95 to 0.99, indicating excellent consistency across raters and test sessions. Internal consistency, measured by Cronbach’s α, was also strong in several translations (α = 0.98 in Turkish, α = 0.90 in the Fear of Falling Avoidance Behavior Questionnaire (FFABQ-B) context). Correlational analyses, where available, further reinforced construct validity. For example, moderate to strong correlations were reported between BBS and other functional assessments, such as the Timed Up and Go Test (TUG) (r = –0.75), Modified Barthel Index (MBI) (r = 0.67), and Unified Parkinson’s Disease Rating Scale III (UPDRS-III) (r = –0.78), supporting BBS’s relevance in assessing balance and motor function in elderly and Parkinson’s populations. Some studies also reported significant correlations with age, as seen in the Norwegian version (r = –0.36). However, despite the strong psychometric support, several articles lacked detailed statistical reporting on validity measures or did not assess correlations. Overall, the findings confirm the BBS as a robust, reliable tool for cross-cultural clinical use, though further standardization in reporting and broader psychometric evaluations would enhance its global applicability.
Table I A
Studies results
The bias assessment of the psychometric studies included in Table I B reveals an overall moderate to low risk of bias across the selected research. Most studies reported appropriate sample sizes for psychometric evaluations, with several exceeding 60 participants a number generally considered sufficient for basic reliability and validity testing [3, 4, 19]. However, a few studies, such as those by Scalzo et al. and Sahin et al., had relatively smaller samples (< 50), which may affect the generalizability and stability of their psychometric estimates [5, 10].
Table I B
Clarity of studies reporting
Regarding statistical methods, almost all studies applied robust and recognized techniques such as Intraclass Correlation Coefficient (ICC), Cronbach’s α, and Pearson correlations to assess reliability and validity. Some studies, like Salavati et al. and Viveiro et al., also included Standard Error of Measurement (SEM) and Receiver Operating Characteristic (ROC) curves, enhancing their methodological rigor [6, 7].
Clarity of reporting was generally strong. Most studies provided detailed descriptions of their translation, adaptation, and validation procedures. Nevertheless, a few older studies [5, 16] offered less comprehensive methodological explanations, potentially leading to moderate interpretative bias.
While minor concerns related to sample size and reporting detail exist in some studies, the majority of the reviewed research demonstrates high methodological quality, reinforcing the reliability and validity of the BBS across diverse cultural contexts.
Discussion
The BBS has been extensively validated across a variety of populations, languages, and cultural settings, emerging as one of the most reliable and widely used tools for assessing balance impairments, especially among older adults and individuals with neurological conditions such as Parkinson’s disease and stroke. The present review of international literature provides compelling evidence supporting the scale’s psychometric robustness, while also highlighting a significant gap the absence of an Albanian version of the BBS. Considering the growing elderly population and increasing burden of age-related balance disorders in Albania, the development and validation of a culturally adapted BBS is both timely and necessary.
The validation of the BBS across various linguistic and clinical contexts has consistently shown strong inter-rater and intra-rater reliability. For instance, studies conducted in Turkey, Brazil, Norway, and Korea indicated almost perfect reliability [10, 18, 20, 21]. Similarly, Cronbach’s α values, which assess internal consistency, were frequently above 0.90, suggesting that the items within the scale are measuring a coherent construct.
The Urdu version validated by Kashif et al. in people with Parkinson’s disease showed excellent reliability (α = 0.81; ICC = 0.99) and strong correlations with established Parkinson’s measures, demonstrating both reliability and construct validity [4]. Likewise, the Turkish study [10] confirmed convergent validity through significant correlations with the MBI (r = 0.67) and TUG (r = –0.75). These correlations are crucial because they demonstrate that the BBS is not only internally consistent but also meaningfully related to other functional mobility measures.
Successful adaptation of the BBS has occurred in a variety of linguistic and cultural contexts, including Hungarian, Persian, Japanese, and Brazilian-Portuguese [3, 5, 7, 8, 22]. These studies followed standardized cross-cultural adaptation procedures, which typically involve translation, back-translation, expert committee reviews, and pilot testing. Despite differences in health systems, rehabilitation practices, and socio-cultural norms, the scale demonstrated strong measurement equivalence, reinforcing its versatility and applicability across different countries.
This context strengthens the argument for an Albanian translation and validation of the BBS. Albania currently lacks a standardized and validated balance assessment tool. The introduction of the BBS, following cross-cultural adaptation protocols, such as those outlined by Beaton et al., would offer clinicians and researchers in Albania/would provide clinicians and researchers in Albania with a validated, internationally recognized instrument for use in clinical and research settings [13]. Moreover, considering the BBS’s widespread usage, an Albanian version would facilitate international collaboration, comparative research, and evidence-based rehabilitation practices.
The clinical utility of the BBS is underscored in studies such as Viveiro et al., who compared the BBS with other balance assessments (BESTest, Mini-BESTest, Brief-BESTest) in older nursing home residents [6]. While all tools were reliable, the BBS demonstrated solid validity in identifying fall status (ICC = 0.94), though slightly less sensitive than the more dynamic BESTest. Nevertheless, its brevity, simplicity, and minimal equipment requirements make the BBS particularly suitable for resource-limited settings such as many areas in Albania.
Further support comes from the systematic review by Lima et al., which evaluated the BBS’s ability to predict fall risk [11]. While the review acknowledged moderate predictive validity, it also pointed out some limitations, such as ceiling effects in high-functioning individuals and lower sensitivity to subtle balance deficits. These findings imply that while the BBS is a reliable screening tool, it should be complemented with additional assessments for more comprehensive balance evaluation, especially in individuals with higher functional levels.
From a methodological perspective, many studies employed rigorous psychometric analyses, including test-retest reliability, construct validity, and correlation with established scales. For example, Gillespie et al. compared in-person and telerehabilitation BBS scoring in stroke survivors, highlighting the scale’s adaptability to telehealth applications, an increasingly relevant consideration in post-pandemic rehabilitation [15].
However, some articles lacked complete psychometric reporting. Several studies, such as those by Scalzo et al. and Babaei-Ghazani et al., affirmed reliability but omitted detailed correlation analyses or construct validity measures [5, 8]. This variation in reporting standards underscores the need for more uniform methodology and comprehensive data presentation, especially when developing a new cultural adaptation such as an Albanian version.
Although numerous studies included in this review reported psychometric indicators such as ICC, Cronbach’s α, and correlation coefficients, a meta-analysis was not undertaken. This decision was driven by the substantial heterogeneity across the available evidence, which varied in cultural and linguistic adaptations, clinical populations, sample sizes, measurement procedures, and statistical approaches. Such variability limits the comparability of results and challenges the assumptions required for valid data pooling. Conducting a meta-analysis under these conditions could lead to misleading summary estimates that overlook important contextual nuances. Instead, the narrative synthesis applied here allows for a more critical appraisal of the evidence, highlighting methodological differences, population-specific findings, and the broader implications for the cross-cultural applicability of the BBS.
This review was restricted to studies published in English, a decision taken to ensure accurate interpretation of methodological procedures and psychometric results. However, this choice inevitably introduces the possibility of language and publication bias, as relevant evidence from other high-output languages such as Chinese, Spanish, and Portuguese may not have been captured. Future reviews would benefit from adopting a multilingual approach to provide a more comprehensive overview of the cross-cultural performance of the BBS. In addition, it is important to acknowledge the limitations of the instrument itself. While the BBS is widely used and supported by strong psychometric evidence, it is subject to ceiling effects in high-functioning or community-dwelling individuals, which can reduce its sensitivity to change in these populations. These limitations should be taken into account when interpreting results and when selecting outcome measures for research and clinical practice.
Despite the robust global evidence base, no validated version of the BBS currently exists in the Albanian language. This absence limits clinicians’ ability to objectively assess and monitor balance deficits among Albanian-speaking populations, both within Albania and in diaspora communities. As the country’s population ages and the burden of falls, Parkinson’s disease, stroke, and frailty increases, the need for standardized, evidence-based assessment tools becomes urgent.
An Albanian version of the BBS would support early detection of balance impairments, guide individualized rehabilitation planning, and facilitate outcome monitoring. Moreover, a culturally adapted tool could account for local language nuances, health beliefs, and environmental challenges that may influence balance, such as uneven terrain in rural areas or lack of accessibility infrastructure.
The process of translation and validation should follow internationally accepted protocols to ensure content validity and reliability. This would typically include: forward translation by bilingual experts; back-translation into the original language; review by an expert committee for semantic and conceptual equivalence; pilot testing on a sample of older Albanian adults and full psychometric evaluation including factor analysis, test-retest reliability, and construct validity.
Given Albania’s limited access to sophisticated rehabilitation technologies, the simplicity, cost-effectiveness, and portability of the BBS make it an ideal candidate for widespread use in both urban clinics and rural health posts.
Future directions and recommendations
To address existing research gaps, several supportive measures should be considered in future studies. First, extending literature searches to include non-English publications would provide a more comprehensive understanding of cross-cultural adaptations and psychometric evaluations of the BBS. Second, studies should investigate strategies to mitigate known limitations of the scale, such as ceiling effects in high-functioning populations, potentially through complementary balance measures or modified scoring approaches. Third, the use of standardized methodologies across diverse populations would facilitate comparison and synthesis of findings, strengthening the evidence base. Implementing these measures will enhance the validity, applicability, and clinical utility of the BBS across different contexts and populations.
To enhance the utility of the BBS in Albania and beyond, the following recommendations are proposed:
Translation and validation: develop an Albanian version of the BBS following cross-cultural adaptation guidelines.
Training and dissemination: educate clinicians and physiotherapists on proper administration and interpretation of the scale.
Research integration: use the Albanian BBS in future research on falls, frailty, and balance rehabilitation to build national evidence.
Complementary tools: combine BBS with other assessments (Mini-BESTest, TUG) in higher-functioning individuals for comprehensive analysis.
Technology utilization: explore mobile or digital BBS applications for tele-rehabilitation and rural outreach.
In conclusion, the international literature confirms that the BBS is a reliable, valid, and clinically useful tool across a wide range of settings and populations. The absence of an Albanian version represents a clear gap in national rehabilitation capacity. Developing and validating an Albanian BBS would significantly improve the assessment and management of balance disorders and align Albania with global standards in physical therapy and geriatric care. The strong psychometric foundation from other cultural adaptations offers a roadmap for implementation and underscores the BBS’s enduring relevance in modern clinical practice.