Faced with one of the most pressing public health, social, and economic challenges of our time, the STOP OBESITY Partnership (Partnership for the Prevention and Treatment of Obesity) was established in 2022 as a direct response to the growing obesity epidemic in Poland. This initiative represents the most significant emerging expert-driven and social movement in the country, bringing together scientific, academic, patient, social, and self-governmental organizations as well as companies that actively engage in, or support, effective solutions for preventing obesity and treating it as a chronic disease.
The STOP OBESITY Partnership is the first initiative of its kind in Poland (and among the first in the CEE region) – an independent and open platform that brings together experts in public health, representatives of civil society, local governments, and the business community. Entirely non-promotional in nature, the partnership is committed to developing a multisectoral, coordinated response to the growing challenge of obesity.
The prevalence of obesity continues to rise steadily. Compared with 1990, the global prevalence of obesity has increased by 155.1% in males and 104.9% in females, accompanied by an increasing incidence of obesity-related complications that affect virtually every organ system, including the heart, thereby elevating the risk of cardiovascular disease and cancer [1, 2]. In response to this growing public health challenge, various scientific and professional communities are intensifying efforts to prevent and manage obesity. Notably, in 2024, the latest edition of the Clinical Recommendations for the Management of Obesity was published under the auspices of the Polish Society for the Treatment of Obesity [3]. As reported by the National Health Fund in its publication The NFZ on Health: Obesity and Its Consequences, 56.6% of individuals in Poland over the age of 15 are affected by overweight or obesity, with 18.5% classified as obese. Moreover, projections indicate that by the end of 2025, 25.9% of women and 30.3% of men aged 20 years and older in Poland will be living with obesity – nearly 9 million individuals. This positions obesity as the third most prevalent risk factor for cardiovascular disease (CVD), behind lipid disorders and hypertension. This trend is particularly concerning given that obesity is consistently identified as a primary risk factor for CVD in various guidelines and algorithms [4]. This rising tide of obesity poses significant implications not only for the health of the population but also for the sustainability and capacity of the healthcare system [5].
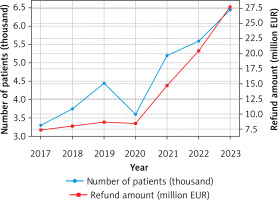
According to data from the International Agency for Research on Cancer (IARC), Poland is among the four member states of the current European Union with the highest proportion of malignant cancers attributable to elevated body mass index (BMI) – nearly 7% of all cases. For comparison, this proportion is approximately 4.3% in France and 4.5% in Sweden [6]. Furthermore, data from the public healthcare payer (Figure 1) indicate a rapidly escalating financial burden associated with funding bariatric surgery [5].
Figure 1
Bariatric procedures in Poland (2017– 2023) with trends in the number of patients and corresponding National Health Fund (NFZ) refund amounts (converted from PLN to EUR using an exchange rate of 1 EUR = 4.5 PLN)
Fiscal policy remains one of the most effective instruments for mitigating the adverse health consequences of unhealthy dietary patterns, including the consumption of sugar-sweetened beverages – a major contributor to obesity [7]. Among such measures, the introduction of a sugar tax stands out as both a powerful public health intervention and a potential sustainable source of funding for obesity prevention strategies. Implemented in Poland in 2021 with the aim of reducing the intake of highly sweetened drinks, the tax generated revenues of PLN 1.5 billion (~EUR 333 million) in 2021, PLN 1.6 billion (~EUR 356 million) in 2022, and PLN 1.4 billion (~EUR 311 million) in 2023 (as of 7 December 2023), despite falling short of the projected annual target of PLN 2.7 billion (~EUR 600 million). Even at current levels, these funds could provide a stable foundation for long-term, systematic efforts to curb overweight and obesity, provided they are strategically allocated. However, the revenues from the sugar tax are not earmarked as a separate budgetary category, leading to significant concerns over their ultimate use [8].
According to the March 2025 post-audit statement of the Supreme Audit Office, the proceeds from the sugar tax were spent in ways inconsistent with their intended purpose. There is no dedicated system within the National Health Fund for monitoring, recording, and accounting for these funds. While they are identifiable on the revenue side, they remain undifferentiated within overall expenditures, making it impossible to determine the amounts and purposes for which they were allocated [6]. The sugar tax strategy can be accompanied by implementation of public physical activity policies and other approaches redesigning the obesogenic environment [9].
As the authors of this letter and representatives of the STOP OBESITY Partnership, we urge policymakers, public health authorities, and the National Health Fund to exercise rigorous, transparent oversight of sugar tax revenues, ensuring that these funds are used exclusively for their intended purpose. We call for a decisive shift in focus towards robust, evidence-based primary prevention strategies – addressing the root causes of obesity, rather than relying predominantly on costly treatment of its consequences. We therefore propose the establishment of a dedicated public health financing mechanism (fund), sustained by revenues from the sugar tax as well as alcohol and tobacco excise duties, as a transparent and stable basis for a comprehensive, multi-level public health strategy. Such a solution is both justified and necessary to provide a stable basis for a comprehensive, multi-level public health strategy that prioritizes prevention of obesity (as well as other significant health risk factors) as a root cause of many non-communicable diseases. Allocating resources from this fund according to an algorithm that reflects demographic, epidemiological, and social differences would offer a real chance to narrow health inequalities stemming from social, economic, and environmental factors. Only through sustained investment in prevention can we reverse current trends and protect the health of future generations.



