Perioperative care is crucial for improving postoperative survival in children with congenital heart disease. The duration of mechanical ventilation is one of the important factors influencing the outcomes. Complications and mortality are higher in patients with prolonged mechanical ventilation (PMV) [1]. On average weaning from mechanical ventilation is performed within 24 h after cardiac surgery [2, 3]. The prolonged mechanical ventilation may be influenced by several factors, some of which may occur pre-operatively and result from baseline characteristics [2, 4]. Identification of preoperative factors that may influence the postoperative period is essential for paediatric intensive care [5, 6].
The aim of the study was to analyse which parameters have a prognostic value for PMV in children after cardiac surgery.
One hundred and eighteen consecutive patients were operated on between July 2020 and March 2021. Children who underwent procedures without cardiopulmonary bypass (CPB) and those who had been intubated in preceding days were excluded from the analysis. Finally, 103 patients were included to the study group. Several definitions for PMV are reported in the literature [1–3, 5]. According to most common literature descriptions and anaesthesia assessment, we defined PMV in the present study as a continued intubation after 24 h following surgery [2, 4].
Demographic and clinical history, laboratory and peri-operative data were collected. Blood samples were collected at baseline and routinely after the surgery. Whole blood count parameters were analysed using routine haematology analyser. The inflammatory indices were calculated based on the whole blood sample analysis. The normal ranges of red cell distribution width (RDW) were 37–54 fl. The association between baseline blood parameters and post-surgical outcomes including PMV was analysed.
The study was approved by the Local Ethics Committee (545/22).
Data were tested for normality with the Shapiro-Wilk test. Continuous parameters which were not normally distributed were presented as median with interquartile range (IQR) and compared with nonparametric Mann-Whitney test. Categorical data were presented as numbers and percentages and compared with Fisher’s exact test. Differences in the intubation time between surgeries due to different types of heart defects were analysed with Kruskal-Wallis test. Then, a correlation between intubation time and RDW was checked with Spearman’s rho test. Receiver operating characteristic (ROC) analysis was performed and the area under the curve (AUC) values with optimal cutoff values of RDW for predicting PMV over 24 h were assessed. The AUC values were compared using the DeLong test.
We performed uni- and multivariable logistic regression with backward stepwise selection to evaluate predictors of PMV. The multivariable model was adjusted for data presented in Table I.
Table I
Association of clinical and peri-operative factors and PMV in the univariate and multivariable analysis
P < 0.05 was considered statistically significant. Statistical analysis was performed using JASP statistical software and SPSS ver. 23.
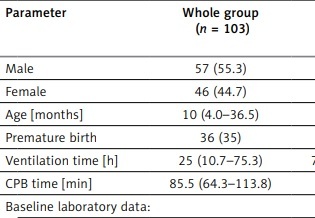
A total of 103 patients were analysed (46 females, 57 males, median age of 10 months, IQR: 4–36.5 months) operated on due to cyanotic congenital heart disease, valvular disease or shunt lesions. The duration of intubation differed between patients depending on the surgery type (p = 0.041), with the shortest duration in patients undergoing valvular procedures. Fifty-five (53.4%) patients had PMV (PMV group). Demographical and peri-procedural data are presented in Table II.
Table II
Demographic and peri-procedural data of study patients
[i] Continuous variables are expressed as the medians (Q1–Q3) whereas categorical variables are expressed as the numbers (n) with percent (%). CPB – cardiopulmonary bypass, Leu – leucocyte count, Lymph – lymphocyte count, Hb – haemoglobin, Mono – monocyte count, Neu – neutrophil count, RBC – red blood cell count, RDW – red blood cell distribution width, PLT – platelet count.
Median RDW value in the PMV group was 41.4 fl (Q1–Q3 37.3–48.5; min.: 32.9, max.: 71.6) and 37.2 fl (Q1–O3 35.6–38.95; min.: 32.3, max.: 51.3) in the non-PMV group. RDW values over the upper reference value were observed only in the PMV group (9 vs. 0 patients, p = 0.003). The duration of intubation correlated with RDW value (p < 0.001; Spearman’s rho; r = 0.417).
In the next step, we performed univariate (Table I) and multiple logistic regression with backward selection. In the multiple model preoperative RDW (p < 0.001; OR = 1.22, 95% CI: 1.0865–1.3615), while among clinical and procedural data CPB time (p < 0.001; OR = 1.027, 95% CI: 1.0115–1.0431) were significant predictors of PMV. The risk of PMV increased by 22% for every 1 unit (fl) increment in RDW.
The ROC analysis showed that RDW over 40.8 fl had prognostic value for PMV-24 h with AUC = 0.727 with a 54.6% sensitivity and 89.6% specificity (p < 0.001). The analysis for CPB time showed cut-off value over 96 min, with AUC 0.765 yielding a 59.3% sensitivity and an 81.3% specificity (p < 0.001).
Thereafter, we combined both parameters, and the combined RDW and CPB time analysis showed AUC 0.849, with a 79.6% sensitivity and an 81.3% specificity.
Since there are different definitions for PMV, we also performed additional analyses for over 48 h and 72 h of mechanical ventilation, gaining a similar prognostic significance of RDW and CPB time.
The main finding of our study is a prognostic value of preoperative RDW and CPB time for PMV prediction.
Several studies in adult and paediatric surgery and medical therapy have demonstrated the significant value of simple blood analysis in predicting short-term and long-term outcomes [7–10]. The RDW is a simple, routinely analysed blood measurement which denotes the variability in red blood cell (RBC) size. Changes in RDW may occur acutely [11] as the release of reticulocytes to the blood stream causes an increase in RDW. According to Patel et al. [12], the reasons for increased RBC volume variance result from the cell lifecycle during their presence in the bloodstream. Increased RDW is therefore associated with reduced mean volume, increased reticulocyte volume variability, increased heterogeneity in the rate of RBC volume reduction, and delayed clearance [12]. While RBC clearance is well controlled in healthy individuals, changes and reductions occur in a wide range of pathological clinical situations, leaving older – smaller cells in the blood and increasing the RDW. Increased RDW may therefore occur in several conditions, including atherosclerosis, infections, pulmonary and autoimmune disorders. Chronic inflammation is a common feature of most pathogenetic background [7], affecting anaemia, iron release, and erythropoiesis. Importantly, increased RDW was associated with a higher risk of death and worse postoperative outcomes [13], and its decrease after intensified treatment is associated with a better prognosis [14]. However, there are less data in the paediatric literature on the usefulness of RDW compared to studies in adults. Our study showed that increased RDW is correlated with PMV. Otero et al. [11] demonstrated an inverse relationship between increased RDW and ventilation-free days in the intensive care unit.
It is reasonable that systemic inflammation deforms RBC membranes, affects RBC survival, and delays cell maturation. Moreover, RDW increase may occur in the so-called stress erythropoiesis [11] in the presence of hypoxia, stress-induced factors, glucocorticoids, which leads to increased RBC production.
Schepens et al. [15] showed that RDW increase at the time of admission to the paediatric intensive care unit was associated with respiratory failure and the need for mechanical ventilation. Said et al. [16] reported a higher RDW associated with mortality and morbidity in critically ill children. In their analysis, RDW correlated weakly with ventilation-free days.
Prolongation of CPB time is a well-known factor associated with PMV. CPB induces leucocyte and complement activation, release of inflammatory mediators including oxygen-free radicals, cytokines, platelet-activating factor, nitric oxide and endothelin. If the systemic response is greatly exaggerated, the postoperative period may be complicated by organ dysfunction [5]. CPB time and PMV are also more common in children with cyanotic heart disease and those undergoing surgery for complex congenital heart disease [4]. In contrast, some reports suggest that the usual weaning guidelines, rather than the complexity of the operation are more appropriate for determining readiness for extubation [3].
There is an impressive number of papers in the literature evaluating the factors that may influence PMV. The wide range of PMV definition is significant, from 12 and 24 h [2, 4] to over 7 [5, 17] or even 21 days [1]. These facts indicate the importance of the issue and still serious doubts arising from this procedural complication.
One limitation of our study is its retrospective nature and the lack of RDW measurements in the days following surgery. However, the preoperative analysis was performed without blood transfusions and therefore the risk of foreign red blood cells affecting the RDW and PMV results [18] was omitted. Another limitation is a relatively low cut-off value for RDW, which results from very low RDW values in the non-PMV group. However, all upper values and values over the reference were obtained in the PMV group. Hence, our study aimed to show the association between increased RDW and the risk of PMV, rather than to set the definite RDW cut-off values.
In conclusion, higher RDW and longer CPB time might be predictors of PMV. Combined RDW and CPB time have the highest value for PMV prediction.