Patient experience, a key indicator of high-quality care, is gaining increasing attention among healthcare institutions aiming to strengthen their performance metrics and maintain competitiveness in the evolving healthcare landscape [1]. Variations in the quality of care provided to cancer patients across healthcare facilities influence not only clinical outcomes but also patient experiences and perceptions, underscoring the growing importance of quality assessment in the context of safety and healthcare efficiency. This emphasis on patient experience aligns with the broader shift toward patient-centered cancer care delivery models, when the doctor–patient relationship, medical staff-patient relationship, and support services-patient relationship, when a cancer diagnosis is being communicated, is an important aspect that defines a patient’s situation [2, 3].
Today, patient experience is increasingly acknowledged as a core pillar of healthcare quality, on par with/comparable to clinical effectiveness and safety [4]. Its systematic assessment is regarded as essential for driving continuous quality improvement. Nutrition, as an integral part of therapy, plays a critical role in supporting health, preventing complications, and optimizing treatment outcomes. However, numerous studies have reported low levels of patient satisfaction with hospital food services. Hospital meals are often mass-produced, relying on frozen, canned, or highly processed ingredients, which limits both their nutritional value and taste. Consequently, patients frequently report dissatisfaction, encounter mealtime challenges, and depend on family members to bring food from outside, leading to varied experiences of care [5, 6].
Patient satisfaction is widely recognized as a reflection of an institution’s commitment to delivering high-quality, patient-centered care. In the United States, for example, patient satisfaction scores are publicly reported and tied to reimbursement through Medicare and Medicaid programs. Research has primarily focused on aspects such as communication with healthcare providers, psychological support, and access to patient education. In contrast, the physical environment – though known to impact patient experience – has received less systematic attention. Nevertheless, factors such as cleanliness of hospital wards, clarity of signage, ease of navigation, and room conditions play an important role in shaping patients’ and caregivers’ overall impressions of care [7].
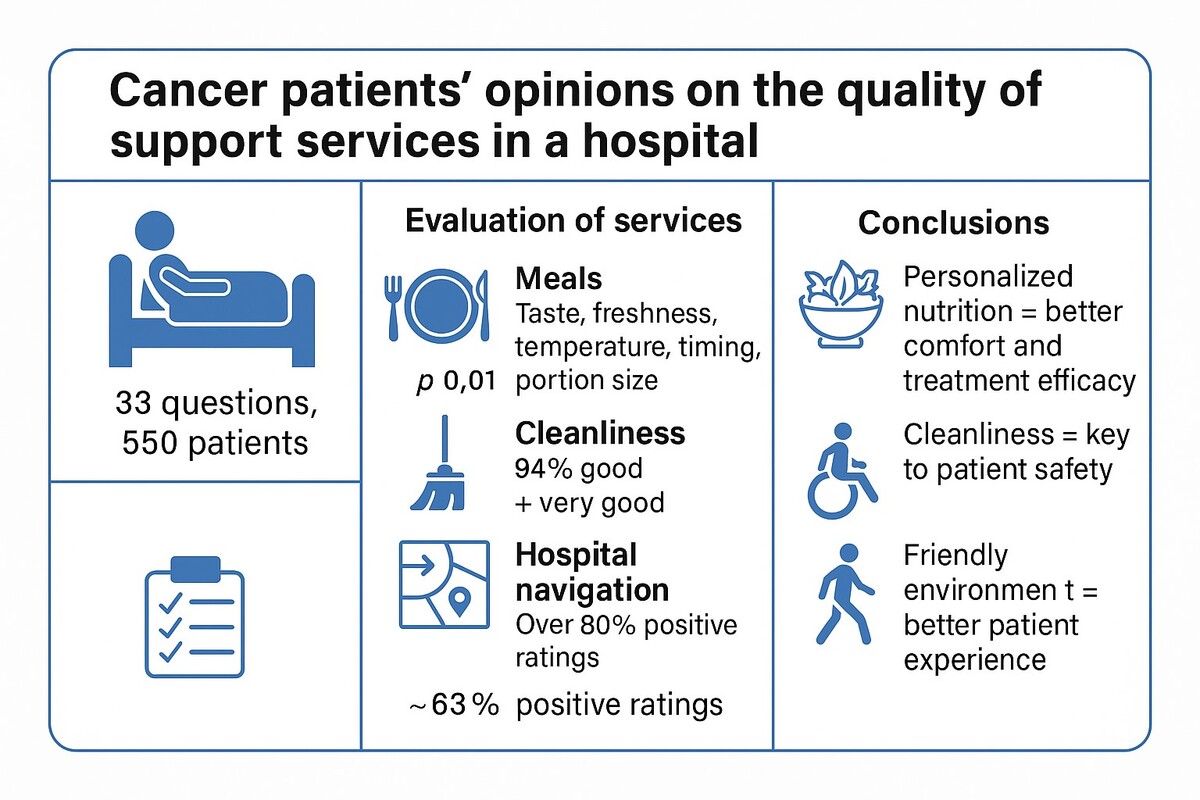
This study aims to explore cancer patients’ perspectives on the quality of selected support services in healthcare, including meal services, ward cleanliness, clarity of signage, and ease of hospital navigation. The findings are expected to help identify areas for safety and service improvement, particularly in the context of therapeutic nutrition and the patient care environment.
Methods
The study was conducted in 2021 at a specialized oncological hospital. A purposive sampling method was applied. Participants were patients hospitalized in one of the hospital wards who met the inclusion criteria: current hospitalization and the provision of informed consent to participate in the study.
Data were collected using a structured questionnaire comprising 33 closed-ended questions, divided into seven thematic sections to enhance clarity and facilitate patient comprehension. Additionally, the survey included one open-ended question inviting patients to provide further comments or suggestions. Patients received detailed instructions emphasizing the importance of completing the questionnaire accurately.
Due to the breadth of the collected material, the analysis was divided into two thematic areas, each presented in a separate manuscript. This manuscript focuses on patient perceptions of selected support services, including meal delivery, hospital cleanliness, clarity of signage within hospital facilities, and ease of navigation throughout the hospital.
Meal quality was comprehensively assessed. Patients were asked to evaluate various aspects of food services, including taste, freshness, serving temperature, hygiene of delivery, meal timing, and portion size. Furthermore, they were asked whether the meals served were consistent with their individual dietary requirements.
The subsequent section addressed auxiliary/support services such as the cleanliness of hospital wards, the clarity and transparency of directional signage, the ease of moving around hospital premises, and room facilities – such as the presence of a chair for visitors. Patients were also asked whether they believed the hospital infrastructure was adapted to the needs of individuals with physical disabilities and elderly people with mobility limitations.
The final part of the survey consisted of an open-ended question concerning the overall quality and safety of care within the hospital ward, allowing patients to express their general opinions about the institution.
Statistical analysis
Statistical analyses were conducted using statistica software, version 13.0 (StatSoft Inc., 2017; www.statsoft.com). To assess the relationships, strength, and direction between categorical variables, Pearson’s χ2 test and Cramér’s V were employed. A p-value < 0.05 was considered statistically significant.
Results
Patients who positively evaluated the taste (p < 0.01), freshness (p < 0.01), temperature of meals (p < 0.01), meal timing (p < 0.01), and portion size (p < 0.01) were satisfied with the quality of meals served at the hospital. Cramér’s V test indicated that these relations were moderately strong, and in the case of meal timing, this relation was quite strong, suggesting that this aspect is particularly important for patients.
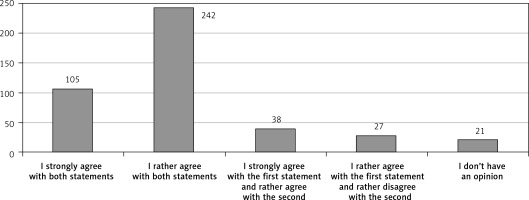
Figure 1 is a synthesis of patients’ responses to questions about the quality of meals served at the hospital, as well as questions about meal timing. For clarity, the chart includes only variants that were obtained more than 20 times. The total number of responses provided was 530.
Patients who received meals in accordance with their individual dietary recommendations (p < 0.01), had the option to heat meals (p < 0.01), and store them in the refrigerator (p < 0.01) were satisfied with the quality of meals received at the hospital. The Cramér’s V test indicated that the first relation was moderately strong, while the remaining ones were rather weak.
Overall, patients rated cleanliness, clarity of the hospital’s signage, ease of reaching its various parts, equipment in hospital/patient rooms, and adaptation to the needs of physically disabled individuals as good or very good (Table I).
Table I
Hospital evaluation in terms of various aspects by patients
Patients positively assessed the clarity of the hospital’s signage (p < 0.01) and the ease of reaching its various parts (p < 0.01) and believed that it is well adapted to the needs of physically disabled individuals. Cramér’s V test showed that these relations were rather weak.
An open-ended question was answered by 44 patients. Many patients highlighted the courteous treatment by nursing staff, especially in the day chemotherapy unit. Additionally, in the open-ended question, patients commented on the meals – their taste and the frequency of meal service. Several patients also noted the somewhat lengthy admission process to the ward.
Discussion. Nutrition. A properly balanced diet can impact not only the overall condition of the patient but also reduce the toxicity of therapy and improve drug tolerance. The diet should be tailored to the individual needs of the patient, taking into account both the type of tumor and the type of therapy. In many research studies, nutrition is one of the most basic ways to maintain good health, prevent sickness, and maximize clinical benefit – as a part of therapy [6]. According to the recommendations of the European Society for Clinical Nutrition and Metabolism (ESPEN), such studies should be conducted regularly, at least once a year. As part of meal evaluation, the input of staff responsible for meal preparation and distribution on the ward may also be significant [8].
The results of our study indicate that there are several factors that determine overall patient satisfaction with meals, including taste, freshness, temperature, meal timing, and portion size. These are elementary meal characteristics that must be taken care of to ensure patient satisfaction. Similar conclusions are drawn from other scientific publications examining patient experiences with hospital food [9, 10].
Maintenance of cleanliness
The cleanliness is a key element for the patient’s stay in the facility, and neglect in this area is not only a visual problem but can also pose a potential health hazard to the patient’s health [11]. The assessment of cleanliness can also be conducted in various ways, with the least effective method appearing to be the visual method, which does not allow verification of whether pathogens are present on a given surface [12].
Other support services such as signage and ease of movement
Patients spend the majority of their hospital stay in the wards, and the wards have more floor space than any other hospital department and ease of movement around the ward and ward signage are crucial in terms of patient safety and their experiences [13].
Studies about nutrition and mobility risks include complex and interrelated physiological, medical, and social factors. A growing body of evidence demonstrates that the built environment can affect patients’ experience, safety and recovery. In 1-day annual cross-sectional study used online questionnaires in 31 different languages to collect ward-specific and patient-specific variables in connection with architectural features. The main result is that the hospital environment may affect hospitalized patients’ mobility, independence, and nutritional intake [14]. Barriers to mobility in hospital settings can be complex, encompassing various aspects related to the patient and their supportive relatives. These factors may include relational and communication issues, such as those related to staff and treatment, attitudes towards mobility, and environmental factors like insufficient space, and lack of signage, equipment, and furniture in patient rooms [15, 16]. Safe and well-marked walking areas, adequate lighting, well-designed and organized communal areas, access to equipment, and functional furniture have been identified by nurses as factors that could facilitate patient mobility [15]. Conversely, physicians have noted that the physical configuration of patient rooms discourages mobility and encourages patients to remain in bed [16]. Although the built environment has been identified as a barrier to mobility, its role in patient mobilization within hospital settings remains under-researched [15].
In conclusion, dietary care should be individualized, taking into consideration both the type of tumor and the specific therapeutic regimen. Proper nutritional support tailored to the patient’s clinical condition may not only improve comfort but also support the effectiveness of oncological treatment.
Maintaining cleanliness in hospital wards and patient rooms is another critical factor highlighted by patients. It plays a fundamental role in shaping their perception of care quality and contributes significantly to their sense of safety. Cleanliness should be understood broadly – not only as the visual cleanliness of facilities but also as adherence to aseptic protocols and the prevention of microbial transmission, all of which are essential components of patient safety.
Additionally, the presence of clear hospital signage and infrastructure adapted to the needs of older adults and individuals with mobility impairments contributes to a more accessible and patient-friendly environment. These elements represent important, though often underestimated, dimensions of the overall quality of care.
The findings of this study suggest that healthcare systems – both in Poland and globally – should prioritize personalized nutritional care for cancer patients and ensure the highest standards of hospital hygiene. Furthermore, efforts should be made to improve wayfinding systems and infrastructure accessibility for vulnerable patient populations. Such actions can enhance both the efficacy/effectiveness of treatment and the overall patient experience, thereby supporting a more holistic, patient-centered model of care.
Limitations of the study
As with any research, this study has certain limitations that should be acknowledged. The primary limitation is the lack of detailed demographic data, which may constrain the ability to analyze the influence of sociodemographic factors on patient perceptions. Additionally, the study focused exclusively on hospital-based care without specifying the type of hospital ward in which patients were admitted. Given the potential variability in services and patient experiences across different wards, this omission may limit the depth of interpretation.
Furthermore, the study did not encompass other levels of healthcare, such as inpatient rehabilitation, outpatient specialist care, or primary healthcare settings, where patient experiences and support services may differ significantly. Future research should aim to include a broader spectrum of healthcare contexts and more comprehensive patient characteristics to enhance the generalizability and applicability of the findings.